Why Lower Back Relief Matters More Than You Think
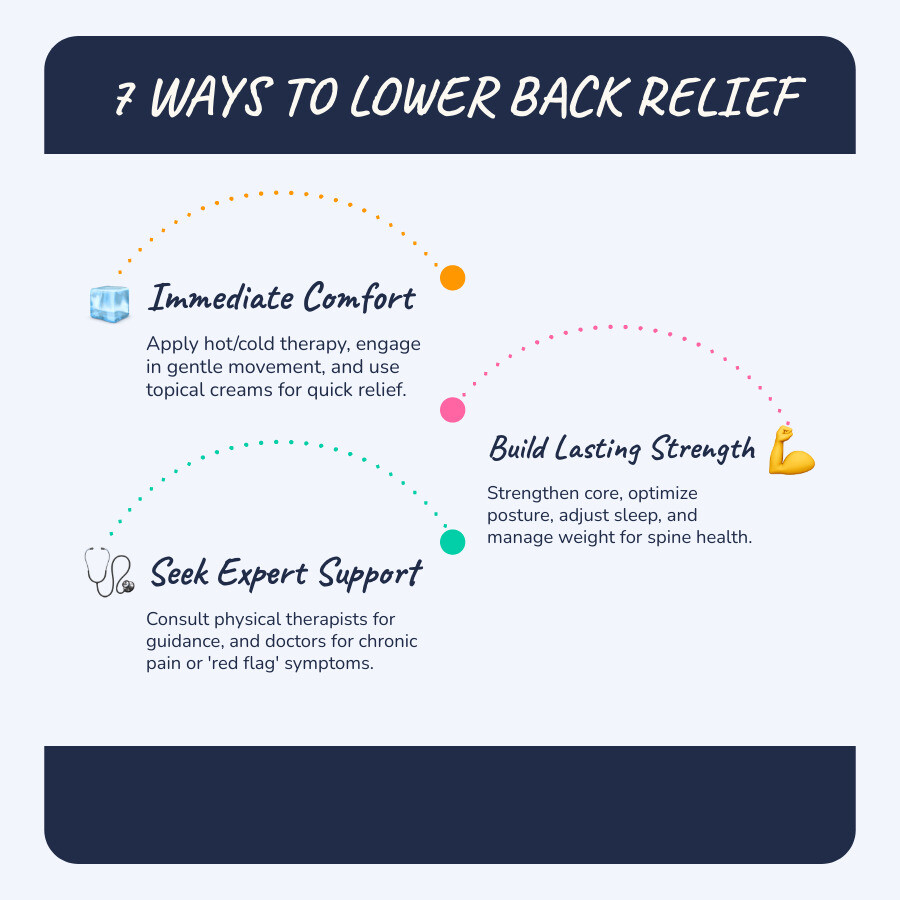
Lower back relief can be achieved through a combination of at-home therapies, targeted exercises, posture adjustments, lifestyle changes, and topical treatments. Here are the most effective strategies:
Quick Relief Strategies:
- Cold therapy (first 48 hours) to reduce inflammation and numb pain
- Heat therapy (after 48 hours) to relax tight muscles and increase blood flow
- Gentle movement like walking instead of prolonged bed rest
- Core strengthening exercises and daily stretching
- Posture corrections while sitting, standing, and sleeping
- Weight management to reduce pressure on the spine
- Topical pain relief creams with natural ingredients like menthol and aloe vera
Lower back pain affects about 80% of Americans at some point in their lives, making it one of the most common reasons people miss work or visit the doctor. Whether your pain is acute (lasting days to weeks) or chronic (persisting beyond 12 weeks), it can steal the joy from everyday activities—from playing with your kids to simply getting out of bed in the morning.
The causes vary widely. Sometimes it's a simple muscle strain from lifting something heavy or twisting the wrong way. Other times, it's related to herniated discs, sciatica, or years of poor posture catching up with you. The good news? Most lower back pain cases resolve on their own within two to four weeks, and there are proven strategies to speed up your recovery and prevent future episodes.
This guide walks you through seven professional-grade approaches to finding real, lasting relief—from immediate at-home therapies to building long-term strength and knowing when to seek medical help.
I'm Tony Enrico, and I've spent years helping people overcome the limitations of nerve and muscle pain through effective, natural solutions. My work with lower back relief has taught me that sustainable comfort comes from understanding your body and giving it the right tools to heal. Let's explore how you can take control of your pain and get back to living the life you deserve.
Lower back relief terms simplified:
- back and neck
- what is sciatica
- Sciatica Relief Cream
1. Find Immediate Relief with At-Home Therapies
When lower back pain strikes, our first instinct is often to stop moving. While short periods of rest can be helpful, prolonged inactivity can actually worsen the problem. The key is to manage the initial pain and inflammation while encouraging gentle movement. Many common causes of lower back pain, such as muscle strains or ligament sprains, respond well to these immediate at-home strategies. Most back pain cases, in fact, resolve on their own within two to four weeks, so don't overreact when the discomfort begins. Our goal is to make those weeks as comfortable and productive as possible.
Apply Hot and Cold Therapy
One of the quickest ways to tackle immediate pain is with a classic duo: hot and cold therapy. Knowing when to use each can make a big difference.
- Ice packs are your best friend for the first 48 hours after an injury, or during acute flare-ups. Cold therapy works by narrowing blood vessels, which reduces swelling and inflammation around the injured area. It also slows down nerve activity, helping to numb the pain signals that reach your brain. Apply ice for about 15-20 minutes at a time, wrapped in a towel to protect your skin, several times a day.
- Heating pads come into play after the initial 48-hour period, or for chronic stiffness and muscle spasms. Heat therapy opens up blood vessels, increasing blood flow to the affected muscles. This improved circulation helps relax tight muscles, soothe stiff joints, and promote healing by delivering oxygen and nutrients. Use a heating pad on a low to medium setting for 15-20 minutes. Just be careful not to fall asleep with it on, as this could lead to burns.
- Alternating therapy can also be effective. After the initial acute phase, some people find relief by switching between cold and heat. This can help reduce inflammation while also relaxing muscles.
Stay Active, But Listen to Your Body
The old advice to rest completely in bed for days on end is a myth that can actually prolong your recovery. While severe pain might warrant a day or two of limited bed rest (a few hours at a time, no more than one to two days), early movement is crucial for lower back relief.
Keeping active helps prevent muscle stiffness, improves blood flow, and strengthens the muscles that support your spine. Gentle activities like walking are highly recommended. A brisk 30-minute walk can be incredibly beneficial. Light stretching also keeps your muscles pliable. The trick is to listen to your body and avoid any movements that increase your pain. Our goal is consistent, gentle activity rather than strenuous exertion.
For more detailed information on managing muscle injuries, check out our guide on Back Strain.
2. Build a Stronger Back with Targeted Exercise
Exercise isn't just about looking good; it's fundamental to achieving and maintaining lower back relief. When you increase your strength, flexibility, and endurance, back pain typically decreases. Your spine needs strong surrounding muscles—especially your core, hips, and back—to support your entire upper body and reduce pressure. Since our core muscles aren't always engaged in daily activities, targeted exercises are essential.
Scientific research supports the benefits of these practices. We've seen that consistent exercise can significantly improve pain and functioning for individuals with chronic back pain. You can find excellent resources, including simple core exercises, to get started.
Stretches for Targeted Lower Back Relief
Stretching daily helps prevent tight muscles from stressing your spine and can provide significant lower back relief. Here are a few effective stretches to incorporate into your routine:
- Knee-to-Chest Stretch: Lie on your back with knees bent and feet flat on the floor. Bring one knee towards your chest, holding it with your hands. Gently pull it closer while tightening your abdominal muscles and pressing your spine into the floor. Hold for five seconds, then release. Repeat with the other leg, and then with both legs simultaneously. Aim for 2-3 repetitions per leg and both legs, ideally once in the morning and once in the evening.
- Cat-Cow Pose: Start on your hands and knees, with your wrists directly under your shoulders and knees under your hips. As you inhale, arch your back, dropping your belly towards the floor and lifting your head (Cow pose). As you exhale, round your spine towards the ceiling, tucking your chin to your chest (Cat pose). Repeat 3-5 times, twice a day, flowing gently between the two positions.
- Pelvic Tilt: Lie on your back with your knees bent and feet flat on the floor. Flatten your lower back against the floor by tightening your abdominal muscles and slightly tilting your pelvis upwards. Hold for 10 seconds, then relax. Repeat 20 times.
- Hamstring Stretches: Tight hamstrings can pull on your pelvis and contribute to lower back pain. However, be cautious with traditional "touch your toes" stretches, as they can sometimes strain lumbar discs. Focus on gentler methods that isolate the hamstring, perhaps using a strap or towel while lying down to pull your leg straight up.
These stretches help release tension and improve flexibility, which are crucial for a healthy back. To understand more about muscle tightness, read our article on Muscle Tension.
The Power of Yoga and Mind-Body Practices

Yoga is a powerful tool for lower back relief, offering both short-term soothing and long-term prevention. Research shows that yoga can significantly reduce back pain by increasing flexibility, improving posture, and strengthening the muscles that support the spine. One small study found that people with chronic low back pain who practiced yoga reported significantly less pain after just eight weeks.
Here are some yoga poses that can particularly help:
- Downward-Facing Dog: This pose stretches the hamstrings, calves, and spine while strengthening the arms and legs. Start on your hands and knees, then lift your hips towards the ceiling, forming an inverted "V" shape. You can keep your knees slightly bent to protect your lower back.
- Child's Pose: A gentle resting pose that can relieve stress and stretch the lower back. Kneel on the floor, sit your hips back towards your heels, and fold your torso forward, resting your forehead on the mat. Extend your arms forward or rest them alongside your body.
Yoga not only builds physical strength and flexibility but also fosters body awareness and stress relief, which are vital for managing pain. If you're dealing with radiating pain, explore our insights on Sciatica Relief.
3. Optimize Your Daily Posture and Positions
Our daily habits—how we sit, stand, and even sleep—have a profound impact on our spinal alignment and the pressure on our discs. Poor posture is a common culprit behind persistent lower back pain. Making conscious adjustments to these positions can provide remarkable lower back relief.
Perfect Your Sitting and Standing Posture
We spend a lot of time sitting, whether at a desk, in a car, or on the couch. Unfortunately, poor sitting posture increases disc pressure more than standing.
- Sitting Posture: When sitting, aim to keep your knees and hips at a 90-degree angle. Ensure your feet are flat on the floor. Your head should be centered over your pelvis, and your shoulders relaxed. Use a lumbar support—a rolled towel or a cushion—between your lower back and the chair to maintain the natural curve of your spine. If you work at a desk, ensure your monitor is at eye level and your arms rest evenly. The most important tip? Take regular breaks. Get up and walk around every 30-60 minutes to relieve pressure.
- Standing Posture: When standing, imagine a string pulling you up from the crown of your head. Keep your shoulders back and down, and your core gently engaged. Avoid locking your knees. Distribute your weight evenly across both feet.
Adjust Your Sleeping Position for Lower Back Relief

The way you sleep can either exacerbate or alleviate your back pain. Achieving a neutral spine position while you rest is key.
- Side Sleeping: This is often recommended for lower back relief. Lie on your side and place a pillow between your knees. This keeps your hips, pelvis, and spine in better alignment, reducing strain on your lower back.
- Back Sleeping: If you prefer sleeping on your back, slide a small pillow or rolled towel under your knees. This helps maintain the natural curve of your lumbar spine and takes pressure off your lower back.
- Mattress Firmness: Your mattress plays a big role. While personal preference varies, a comfortably firm mattress that provides adequate support for your spine is generally best. If your mattress is old and sagging, it might be time for an upgrade.
4. Make Key Lifestyle Changes
Beyond immediate pain management and targeted exercises, long-term lower back relief often hinges on broader lifestyle modifications. Our overall health, body weight, and daily habits directly influence spinal health, inflammation levels, and nutrient delivery to our discs and bones.
Manage Your Weight
Excess body weight, particularly around the abdomen, places significant strain on your lower back. A body mass index (BMI) greater than 25 (indicating overweight or obesity) increases the likelihood of back pain. Losing even a small amount of weight can make a big difference in reducing pressure on your vertebrae and discs, leading to substantial lower back relief.
A healthy diet and regular exercise go hand-in-hand with weight management. Focus on nutrient-rich foods that reduce inflammation and support overall well-being. For comprehensive support, consider how our Body Pain Creams can complement your weight management efforts by providing targeted relief during your journey.
Support Your Spine Health
Several habits can either nurture or harm your spine.
- Quit Smoking: This is a big one. Smoking restricts blood flow to the discs that cushion your vertebrae, leading to quicker disc degeneration. It also reduces calcium absorption and new bone growth, increasing the risk of fractures due to osteoporosis. Quitting smoking is one of the best things you can do for your overall health, including your spine.
- Stay Hydrated: Dehydration can exacerbate lower back pain. Your spinal discs are largely made of water, and proper hydration helps them remain plump and cushioning. Aim for at least 4-6 cups of water a day to keep your spine flexible and supportive.
- Nutrient-Rich Diet: Ensure your diet includes adequate vitamins and minerals. Optimizing your vitamin D and K2 levels, for example, is crucial for bone health and can prevent the softening of bones that contributes to lower back pain.
For more invaluable tips on maintaining strong bones and healthy nerves, explore the resources from the National Institute on Aging on osteoporosis.
5. Explore Professional Guidance for Lasting Relief
Sometimes, despite our best efforts at home, lower back pain persists. This is when professional guidance becomes invaluable. Chronic pain, defined as pain lasting three months or longer, often requires a more personalized, multidisciplinary approach. Experts can help us understand the root cause of our pain and develop a custom management strategy.
Physical Therapy-Inspired Movements and Self-Care
Physical therapists are experts in movement and function. They can create custom exercise plans designed to strengthen weak muscles, improve flexibility, and correct improper posture and body mechanics. Their techniques often include:
- Targeted Exercises: Focusing on core, hip, and back muscles to build strength and stability.
- Posture Retraining: Teaching you how to move and hold your body in ways that minimize strain.
- Self-Massage Techniques: Guiding you on how to use tools or your own hands to release muscle tension.
Physical therapy can be incredibly effective in preventing symptoms from returning. For more on managing muscle discomfort, dig into our article on Muscle Pain.
Alternative Approaches for Comfort
Beyond traditional physical therapy, several complementary and alternative therapies have shown promise for lower back relief:
- Chiropractic Care: Spinal manipulation, performed by licensed specialists, is a recommended non-invasive treatment for low back pain. It aims to improve pain, range of movement, and flexibility. Some studies even suggest that for sciatica, chiropractic care can offer comparable relief to surgery.
- Massage Therapy: This hands-on manipulation can relax tight muscles, reduce pain, and improve posture and alignment. One study found that weekly massage over a 10-week period improved pain and functioning for people with chronic back pain, with benefits lasting about six months.
- Acupuncture: This ancient practice involves inserting thin needles into specific points on the body. Research has shown it can be effective for chronic back pain, with some patients experiencing complete relief from sciatica symptoms.
- Mindfulness and Biofeedback: Chronic pain can be emotionally draining. Mindfulness and meditation help manage the psychological aspects of pain, reducing stress and improving coping mechanisms. Biofeedback, which teaches you to control physiological responses like muscle tension, has even been shown to reduce pain intensity by about 30%, sometimes more effectively than medication.
These approaches can often be combined with other home remedies for better results, offering comprehensive strategies for managing conditions like a Pinched Nerve in the Lower Back.
6. Know When to See a Doctor
While many cases of lower back pain resolve with self-care, there are times when medical attention is crucial. Knowing these "red flag" symptoms can help you determine when to move beyond home remedies and seek professional help.
Identifying "Red Flag" Symptoms
These are signs that your back pain might indicate a more serious underlying condition requiring immediate medical evaluation:
- Numbness or weakness in your legs that is new or worsening.
- Loss of bowel or bladder control, which could indicate a serious nerve compression.
- Fever or unexplained weight loss accompanying your back pain.
- Severe abdominal pain that could be referred pain from another issue.
- Pain after a fall, injury, or trauma.
- Severe night pain that disrupts sleep or pain that doesn't improve with rest.
- A history of cancer (back pain could be related to metastasis).
- Age over 55 with no obvious reason for the pain.
- If you are immunocompromised (at increased risk of infection).
If you experience any of these symptoms, don't hesitate to contact a healthcare provider in New York City immediately.
Understanding Chronic Pain and Medical Options
If your lower back pain persists for more than three months, it's considered chronic. At this point, a thorough medical evaluation is essential to accurately diagnose the cause and explore appropriate treatments. This might involve physical exams, imaging tests (like X-rays, MRI, or CT scans), or blood tests.
When conservative treatments like physical therapy and medication haven't provided sufficient lower back relief, your doctor might discuss other options:
- Injections: Epidural steroid injections can help reduce inflammation around nerve roots, providing temporary relief and allowing you to participate more effectively in physical therapy.
- Surgical Interventions: Surgery is typically considered a last resort, reserved for cases where there's a clear structural issue (like a bulging disc pressing on a nerve) that hasn't responded to extensive non-surgical treatments. Procedures like discectomy (removing part of a disc), laminectomy (removing bone to decompress nerves), or spinal fusion (joining vertebrae) carry risks and are irreversible. The best spine surgeons will advocate for surgery only after all other conservative options have been exhausted.
Understanding the potential Lower Back Pain Causes can help you have a more informed discussion with your healthcare provider.
7. Use a Soothing Topical Cream
For localized lower back relief, topical creams offer a convenient and effective solution. These creams are designed to be applied directly to the skin over the painful area, delivering active ingredients right where you need them most.
Here's why topical creams can be a game-changer for many:
- Targeted relief: They act directly on the site of pain, providing focused comfort.
- Fast-acting: Many topical creams are formulated to penetrate quickly, offering rapid relief from discomfort.
- Non-systemic side effects: Unlike oral medications, topical creams typically have fewer systemic side effects because less of the active ingredient enters your bloodstream.
- Soothes muscles and nerves: Ingredients are often chosen for their ability to calm muscle spasms and soothe irritated nerves.
At Neuropasil, we've harnessed the power of natural ingredients to create fast-acting topical creams for both nerve pain and sore muscles. Our creams feature:
- Menthol: Known for its cooling sensation, menthol provides immediate pain relief by distracting nerve endings and reducing discomfort.
- Aloe Vera: A natural anti-inflammatory, aloe vera helps soothe irritated skin and tissues.
- Urea: This ingredient helps improve the penetration of other active ingredients, ensuring deeper and more effective relief.
Many of our loyal customers, including athletes recovering from intense workouts, testify to using Neuropasil for a wide range of conditions, including neuropathy, sciatica, fibromyalgia, strains, sprains, general aches and pains, joint discomfort, and specific issues like back and neck pain, cramps, and aching feet. When your body feels stiff or tense, and you find it hard to complete daily tasks, a soothing topical cream can provide that much-needed comfort.
To explore more about how topical solutions can help manage your pain, check out our guide on Muscle Pain Relief Oral vs. Topical Options.
Frequently Asked Questions about Lower Back Pain
How long does lower back pain typically last?
The duration of lower back pain varies significantly depending on its cause and severity.
- Acute pain is usually short-term, lasting from a few days to a few weeks. Many common causes like muscle strains or sprains fall into this category, with 75-80% of cases resolving on their own within two to four weeks.
- Subacute pain typically lasts between 4 to 12 weeks.
- Chronic pain is defined as pain that persists for three months or longer, even after initial treatments. Factors influencing duration include the underlying cause (e.g., disc issues, arthritis), your overall health, and adherence to treatment and lifestyle recommendations.
What is the fastest way to relieve lower back pain?
The fastest way to achieve lower back relief often involves a combination of strategies:
- Cold therapy immediately after an injury to reduce inflammation.
- Heat therapy for muscle relaxation after the acute phase.
- Over-the-counter pain relievers like ibuprofen or acetaminophen (if appropriate for you).
- Gentle movement such as walking, avoiding prolonged bed rest.
- Topical pain relief creams for targeted, fast-acting comfort.
- For severe pain, consulting a healthcare professional for stronger medications or injections might provide quicker relief, though these are often part of a broader treatment plan.
Should I rest or keep moving with lower back pain?
This is a common question, and the answer is nuanced. The old advice of prolonged bed rest is largely outdated, as it can actually worsen back pain by leading to muscle deconditioning and stiffness.
- Avoid prolonged bed rest: For most cases of lower back pain, staying active is crucial.
- Gentle activity is key: Engage in light activities like walking, gentle stretching, or performing simple movements that don't aggravate your pain. This helps maintain mobility, improve blood flow, and strengthen supporting muscles.
- Listen to your body: If a movement causes sharp, intense pain, stop. However, don't confuse mild discomfort with harm. Gradually increase your activity level as your pain subsides.
- Short rest periods: If your pain is severe, short periods of rest (a few hours at a time, up to a day or two) might be necessary, but try to resume gentle movement as soon as possible.
Conclusion: Your Path to a Pain-Free Back
Experiencing lower back pain is incredibly common, but it doesn't have to be a permanent fixture in your life. By adopting a proactive and consistent approach, you can find significant lower back relief and reclaim your comfort and mobility. We've explored seven powerful strategies, from immediate at-home remedies like hot and cold therapy to building long-term strength through targeted exercises and yoga. We've also highlighted the importance of optimizing your posture, making key lifestyle changes like weight management and quitting smoking, and knowing when to seek professional medical guidance.
Consistency is truly key on this journey. Each small step—a daily stretch, a mindful posture adjustment, a hydrating glass of water—contributes to a healthier, more resilient back. Empower yourself with knowledge, listen to your body, and don't hesitate to seek expert help when needed.
For targeted, fast-acting topical relief that soothes sore muscles and nerve discomfort, consider a natural cream like Neuropasil. Our unique blend of Aloe, Urea, and Menthol is designed to provide the comfort you need to keep moving forward.
Ready to say goodbye to discomfort? Find the best creams to soothe your nerves and start on your path to lasting lower back relief.
References
NIH (National Institute of Neurological Disorders and Stroke). Low Back Pain Fact Sheet. Available at: https://www.ninds.nih.gov/low-back-pain-fact-sheet Cleveland Clinic. Lower Back Pain. Available at: https://my.clevelandclinic.org/health/diseases/7936-lower-back-pain National Center for Complementary and Integrative Health. Yoga: What You Need To Know. Available at: https://www.nccih.nih.gov/health/yoga-effectiveness-and-safety Harvard Health Publishing. Home remedies for low back pain. Available at: https://www.health.harvard.edu/pain/home-remedies-for-low-back-pain WebMD. Simple Core Exercises. Available at: https://www.webmd.com/back-pain/ss/slideshow-exercises National Institute on Aging. Osteoporosis. Available at: https://www.nia.nih.gov/health/osteoporosis NIH (National Center for Biotechnology Information). Effectiveness of massage therapy for subacute low-back pain: a randomized controlled trial. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1231369/














