Understanding Your Heel Pain

If you're dealing with heel pain, you're not alone. It's a really common problem that can make everyday tasks tough. Think about it: Every mile you walk puts 60 tons of stress on each foot. That's a lot! When your feet take too much stress, pain can pop up.
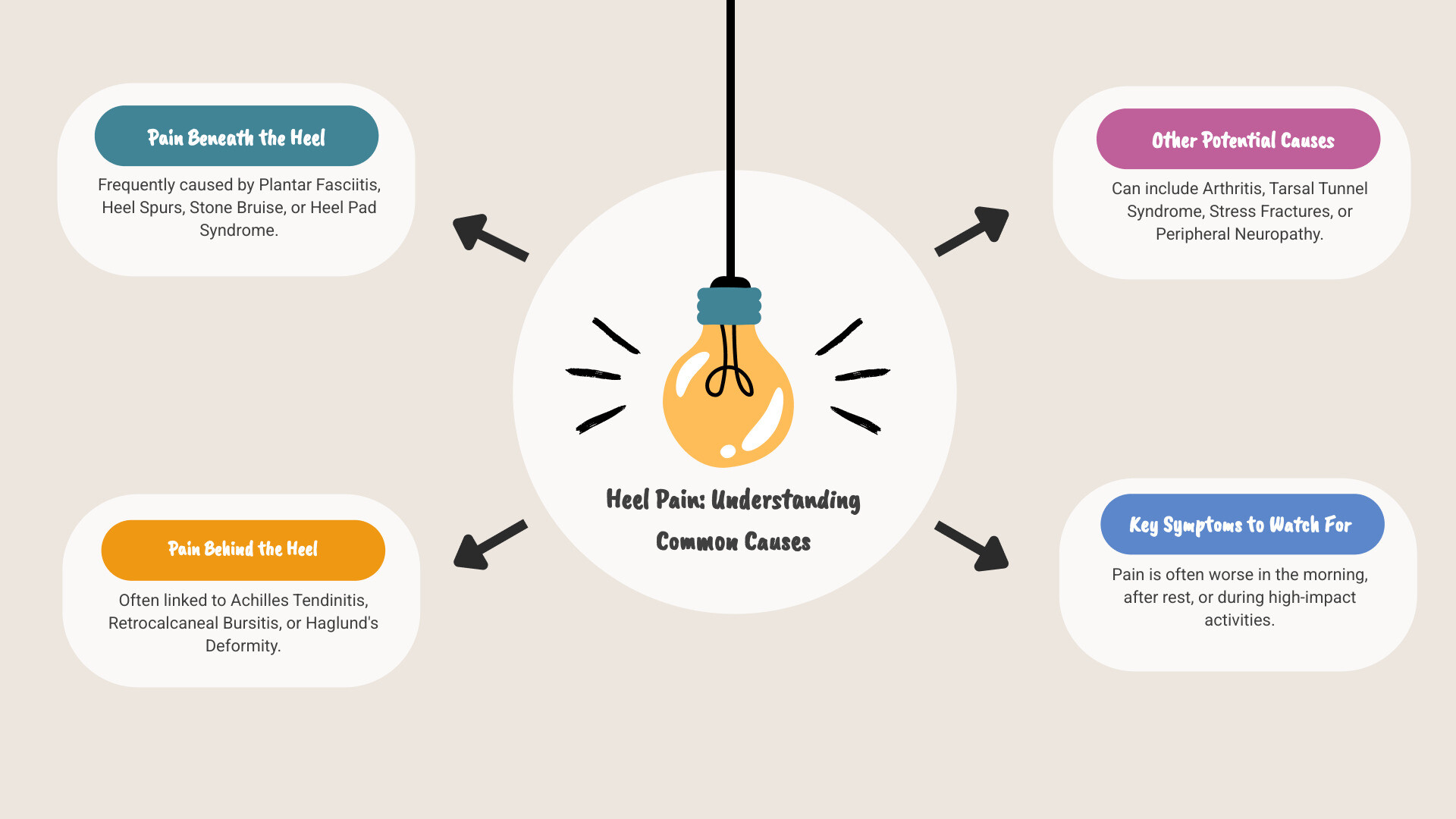
Here’s a quick overview of what heel pain means and what you can do:
- What is it? Pain that shows up in or around the heel bone.
- Why it happens? Often from overuse, like lots of walking or running. Injuries can also cause it.
- Most common cause? Plantar fasciitis, which affects the bottom of your heel. Achilles tendinitis is another big one, causing pain behind the heel.
- Can it be helped? Yes! Most heel pain gets better with simple care like rest, ice, and stretching.
- When to see a doctor? If your pain is severe, gets worse, or doesn't improve after a few weeks of home care.
Heel pain can really slow you down. It might hurt to take those first steps in the morning, or after sitting for a while. Even just standing can become a problem.
The good news is, understanding why your heel hurts is the first step to feeling better. This guide will walk you through the most common causes and how to find relief.
Understanding the Causes of Your Heel Pain
When that sharp, stabbing pain hits your heel, it can leave you wondering what went wrong. Did you step on something? Sleep funny? Or is something more serious happening? The truth is, heel pain can stem from many different causes, and figuring out exactly what's bothering you is the key to getting better.
Here's something we've learned that makes diagnosis much easier: where your pain shows up tells us a lot about what's causing it. Think of it like being a detective – the location of your discomfort gives us important clues about what's going on inside your foot.
Pain Beneath the Heel
If you're feeling pain on the bottom of your heel, you're in good company. This is where most heel pain happens, and it usually involves the tissues that support the sole of your foot.
Plantar fasciitis is the biggest troublemaker here, affecting over 2 million people every year. It happens when a thick band of tissue called the plantar fascia gets inflamed. This tissue runs along your foot's bottom, connecting your heel to your toes like a bowstring. The classic sign? That awful stabbing pain when you first get out of bed or stand up after sitting. It's like your foot is saying "Good morning!" in the rudest way possible.
Heel spurs often get blamed for pain, but they're usually innocent bystanders. These bony growths appear on about half of people with plantar fasciitis, but they're more like a side effect than the actual problem. The real culprit is usually that inflamed tissue we just talked about.
A stone bruise is exactly what it sounds like – you feel like you're stepping on a rock even when you're walking on carpet. This happens when the fat pad under your heel gets bruised from stepping hard on something or landing awkwardly. It's your foot's way of reminding you to watch where you're going.
Calcaneal stress fractures are tiny cracks in your heel bone that develop gradually from too much pounding. Runners and athletes see this more often, and it creates a deep, aching pain that gets worse when you're active.
Sometimes the natural cushioning in your heel starts wearing thin, causing heel pad syndrome. It's like your foot's built-in shock absorber is breaking down, leaving you with a deep, bruised feeling after standing or walking for long periods.
Nerve entrapment can create burning, tingling, or shooting sensations that might spread into your arch or toes. This tricky condition happens when a nerve gets pinched or irritated, and it can be hard to pin down. If you're dealing with nerve-related discomfort, you might find helpful information in our guide on nerve pain relief with Neuropasil.
Pain Behind the Heel
When pain strikes the back of your heel, it's usually your Achilles tendon or the surrounding area that's having trouble.
Achilles tendinitis affects your body's largest tendon – the thick cord that connects your calf muscles to your heel bone. This is a classic overuse injury that loves to target people who suddenly ramp up their activity or runners pushing too hard. You'll feel a dull ache, stiffness, or tenderness just above your heel, especially first thing in the morning or after exercise. For more detailed information about this condition, check out this scientific research on Achilles Tendinitis.
Retrocalcaneal bursitis happens when a small, fluid-filled cushion behind your heel gets inflamed. Think of it as a tiny water balloon that helps your tendon glide smoothly – when it gets angry and swollen, you'll notice pain, warmth, and maybe even a tender bump on your heel's back.
Haglund's deformity has earned the nickname "pump bump" because it's common in women who wear high heels. It's a bony bump that forms on the back of your heel bone from repeated pressure, and it can trigger both bursitis and tendinitis.
In kids and teens, Sever's disease is the top cause of heel pain. Despite its scary name, it's just inflammation of the growth plate in growing heel bones, usually hitting active kids between 8 and 12 years old.
Other Conditions That Can Cause Heel Pain
Sometimes heel pain has less obvious causes that can make diagnosis trickier.
Arthritis in its various forms – including rheumatoid, psoriatic, and others – can settle into your heel area, causing chronic pain and morning stiffness. If arthritis is making your life difficult, our guide on managing arthritis pain: a guide to long-lasting relief offers practical strategies for finding comfort.
Tarsal tunnel syndrome occurs when a nerve gets squeezed in a narrow space near your ankle, creating burning, tingling, or shooting pain that can affect your heel, arch, and toes.
Peripheral neuropathy is nerve damage that can stem from conditions like diabetes, causing numbness, tingling, or burning sensations that sometimes reach your heels.
Stress fractures in other foot bones can send pain signals to your heel area, while systemic diseases like bone infections, tumors, or other rare conditions can occasionally show up as heel discomfort.
The good news is that most heel pain comes from common, treatable conditions. Understanding where your pain is and what it feels like gives you and your healthcare provider a great starting point for getting you back on your feet comfortably.
A Closer Look: Plantar Fasciitis and Achilles Tendinitis
Let's get up close and personal with the two troublemakers that cause most heel pain cases. Understanding these conditions better can be your roadmap to feeling better faster.
What is Plantar Fasciitis?

If heel pain had a poster child, plantar fasciitis would win hands down. This condition affects that thick, sturdy band of tissue called the plantar fascia that runs along your foot's bottom like a bowstring. Think of it as your foot's natural shock absorber and arch supporter rolled into one.
The pain from plantar fasciitis has a very distinctive calling card: stabbing pain right in the bottom of your foot near the heel. But here's the kicker - it's almost always worst with your first steps in the morning. You know that moment when you roll out of bed, put your feet on the floor, and suddenly feel like you've stepped on a shard of glass? That's plantar fasciitis saying good morning.
This happens because while you sleep, your plantar fascia tightens up like a guitar string. When you suddenly put weight on it, it stretches quickly and painfully. The good news? The pain often eases up as you start moving around. The bad news? It can come roaring back after you've been sitting for a while or after periods of rest.
Several factors can put you in the plantar fasciitis danger zone. Age is a big one - most people who develop this condition are between 40 and 60. If you're carrying extra weight, that puts more stress on your poor plantar fascia too. Obesity basically means your foot's shock absorber is working overtime.
Your foot mechanics matter a lot here. Having flat feet or super high arches can throw off how your weight gets distributed, putting extra strain where it shouldn't be. And if you love high-impact exercise like running or dancing, you're asking your plantar fascia to handle a lot of repetitive pounding.
Don't forget about your job either. If you spend long hours on your feet, especially on hard surfaces, you're giving your plantar fascia quite the workout every day.
Here's something important to remember: plantar fasciitis isn't a quick fix. Most cases take three to six months to fully heal with consistent care. Patience really is a virtue here.
What is Achilles Tendinitis?
When heel pain strikes the back of your heel, you're likely dealing with Achilles tendinitis. This involves your Achilles tendon - that thick, rope-like cord you can feel at the back of your ankle. It's actually your body's largest and strongest tendon, connecting your powerful calf muscles to your heel bone.
The pain at the back of your heel from Achilles tendinitis feels different from plantar fasciitis. Instead of that sharp, stabbing sensation, you'll usually feel a dull ache or stiffness. You might notice some swelling and tenderness right along the tendon itself. Sometimes the area feels warm to the touch.
Just like plantar fasciitis, Achilles tendinitis loves to make its presence known in the morning or when you first start moving after sitting still. The pain typically gets worse with activity, which can be really frustrating if you're trying to stay active.
Most of the time, Achilles tendinitis develops from overuse. Maybe you decided to train for a marathon and ramped up your mileage too quickly. Or perhaps you jumped back into basketball after years on the couch. Your Achilles tendon basically says, "Whoa there, slow down!"
Tight calf muscles are often the sneaky culprit behind Achilles problems. When your calves are tight, they pull extra hard on that tendon with every step. It's like having a guitar string wound too tight - eventually, something's got to give.
The connection between your calf muscles and Achilles health is huge. Keeping those muscles flexible and strong isn't just good advice - it's essential for recovery. For helpful insights on how staying active and maintaining muscle health can support your overall comfort, check out our guide on the best ways to relieve muscle aches with physical activity and healthy living.
Both of these conditions might seem daunting, but the good news is that they're very treatable with the right approach and some patience.
Diagnosis and Effective Treatments
Dealing with heel pain can really put a damper on your day, but here's some good news: most cases get much better with simple, non-surgical treatments! The first step to feeling like yourself again is figuring out exactly what's causing your discomfort. Then, we can explore the best ways to get you back on your feet, literally!
How is Heel Pain Diagnosed?
When you finally decide to see a doctor about your heel pain, think of them as a friendly detective. They're going to gather all the clues to pinpoint the problem.
First, they'll do a physical exam. This means they'll gently check your foot and ankle. They'll probably touch around your heel to find exactly where it hurts and if there’s any swelling. They might also ask you to move your foot in different ways or watch you walk. This helps them see how your foot works and where the stress might be.
Next up is your medical history. This is your chance to tell your story. They'll ask things like: When did your pain start? What does it feel like – a sharp stab, a dull ache, or a burning sensation? Does it hurt more at certain times of day, like first thing in the morning? Have you recently changed your shoes, started a new exercise, or had an injury? Every detail you share is a valuable piece of the puzzle!
Sometimes, your doctor might suggest imaging tests to get a clearer picture.
- X-rays are like looking at the bones. They're great for ruling out broken bones (stress fractures), bone spurs, or arthritis. Even if you have a heel spur, it's not always the actual source of your pain.
- More detailed scans like an MRI (Magnetic Resonance Imaging) or Ultrasound might be used if your pain is really stubborn or if your doctor thinks it might be a problem with soft tissues, like tendons, ligaments, or nerves. These give super detailed images of everything under your skin.
At-Home and Conservative Treatments
For most kinds of heel pain, especially common culprits like plantar fasciitis and Achilles tendinitis, the journey to relief often starts right at home! The key here is being consistent and patient.
One of the most important things you can do is rest. Give your painful heel a break from activities that make it worse. Sometimes, this means easing up on running or long walks. For really tough cases, a walking boot or crutches might even be recommended to take all the pressure off.
Then there's the famous RICE method:
- Ice: Applying an ice pack to your heel for 10-20 minutes, a few times a day (especially after activity), can work wonders to calm down pain and swelling. Just be sure to wrap the ice pack in a thin towel so it's not directly on your skin.
- Compression and Elevation: If you have swelling, wrapping your foot gently with a bandage (compression) and propping your foot up above your heart (elevation) can help reduce fluid buildup.
Stretching exercises are super important! Tight calf muscles and Achilles tendons can really pull on your heel, making pain worse. Regular stretching helps loosen things up.
- For your calf muscles, try leaning against a wall with one leg back, keeping your heel down. You can do this with your knee straight (to stretch the top calf muscle) and then with your knee slightly bent (to stretch the deeper calf muscle).
- To stretch your plantar fascia, sit down and cross your sore ankle over your other knee. Grab your toes and gently pull them back towards your shin until you feel a good stretch in the arch of your foot.

Try to do these stretches for 15-30 seconds, in sets of 2 or 3, several times throughout the day. It’s especially helpful to do them before those first painful steps in the morning!
Your shoes matter more than you think! Supportive footwear with good arch support and cushioning can make a huge difference. Try to avoid walking barefoot, especially on hard floors, as this puts a lot of stress on your foot.
Orthotics, which are special inserts for your shoes, can help support your arch and cushion your heel. You can start with simple over-the-counter ones, or your doctor might suggest custom-made orthotics for a perfect fit.
For that awful morning heel pain from plantar fasciitis, a night splint can be a real game-changer. It gently keeps your foot stretched while you sleep, so you don't wake up with that "knife stab" feeling.
Finally, over-the-counter pain relievers like ibuprofen or naproxen can help reduce pain and inflammation temporarily. Always follow the directions on the bottle and chat with your doctor if you have any other health conditions.
Medical Treatment Options
If you've been diligently trying home treatments for several weeks or months and your heel pain just isn't getting better, don't lose hope! Your doctor has other tools in their kit.
Physical therapy is often the next step. A physical therapist is like a coach for your body. They can show you personalized exercises, use hands-on techniques (like massage), and even special equipment to help reduce pain, improve flexibility, and strengthen the muscles that support your foot.
Sometimes, for stubborn inflammation, your doctor might suggest corticosteroid injections. This is a shot of anti-inflammatory medicine right into the affected area. It can bring quick relief, but it's usually used carefully, especially around tendons, because it can sometimes weaken them.
For really chronic cases that just won't budge, Extracorporeal Shock Wave Therapy (ESWT) might be an option. This non-invasive treatment uses sound waves to encourage healing in your heel. Think of it as jump-starting your body's natural repair process.
Your healthcare provider or physical therapist might also show you how to use taping (with athletic or medical tape) to support your arch or heel. This can offer temporary relief and stability.
As mentioned before, if over-the-counter options aren't enough, custom orthotics can be prescribed. These are molded specifically for your feet to correct any imbalances and provide long-term support.
Lastly, surgery is very rare for heel pain. It's usually only considered as a very last resort, after you've tried everything else for many months and your pain is still severely impacting your life.
While these medical treatments are important, we understand that you might still experience lingering nerve or muscle discomfort. Our Neuropasil creams can be a wonderful complementary at-home solution. They are designed to provide targeted relief, helping you manage pain between medical appointments or as part of your daily routine for ongoing comfort.
Prevention and When to See a Doctor
The best way to deal with heel pain is to prevent it from happening in the first place! Taking proactive steps can save you a lot of discomfort. However, it's also crucial to know when your heel pain warrants a visit to the doctor.
Can Heel Pain Be Prevented?
Yes! Many cases of heel pain are preventable by adopting some simple, smart habits. It's about being kind to your feet, which carry you through life!
- Proper footwear: This is non-negotiable. Wear shoes that fit well (front, back, and sides) and offer good arch support, shock-absorbent soles, and supportive heel counters. Replace athletic shoes regularly, as their cushioning and support break down over time. Avoid shoes with excessive wear on heels or soles.

- Maintaining a healthy weight: Excess body weight puts significant additional stress on your feet and heels. Losing even a few pounds can dramatically reduce the load on your plantar fascia and other heel structures.
- Regular stretching: Keep your foot and heel tendons flexible. Incorporate daily stretches for your calves and plantar fascia, even if you're not currently experiencing pain. Think of it as preventative maintenance for your feet!
- Pacing activities: If you're starting a new exercise routine or increasing your intensity, do it gradually. Don't go from zero to marathon runner overnight! Warm up thoroughly before exercise and cool down afterward. Pacing yourself prevents overuse injuries.
- Running surfaces: If you're a runner, try to run on softer surfaces like grass or tracks rather than concrete or asphalt whenever possible. This reduces the impact on your feet. For more comprehensive advice on avoiding injuries during your runs, check out our tips to prevent running injuries.
- Listen to your body: If you feel a dull ache starting, don't push through it. Rest, ice, and give your feet time to recover before the problem escalates.
When Should You See a Doctor?
While many cases of heel pain improve with at-home care, there are times when professional medical attention is necessary. Don't hesitate to reach out if you experience any of the following:
- Severe pain and swelling: If your pain is intense, sudden, and accompanied by significant swelling or bruising, it could indicate a more serious injury like a fracture or rupture.
- Inability to walk normally: If you can't put weight on your foot, or if your pain significantly alters your gait, it's time to see a doctor.
- Pain that persists for weeks: If your heel pain doesn't improve after 2 to 3 weeks of consistent home treatment, or if it's getting worse, a medical evaluation is needed to determine the underlying cause and a more targeted treatment plan.
- Signs of infection: Redness, warmth, pus, or fever accompanying your heel pain could indicate an infection, which requires immediate medical attention.
- Numbness or tingling: These symptoms, especially if they radiate into your toes, could suggest nerve involvement, like tarsal tunnel syndrome, which needs proper diagnosis and treatment.
Early diagnosis and treatment can often prevent heel pain from becoming a chronic problem.
Take the Next Step Towards Heel Pain Relief
If you've made it this far, you now have a comprehensive understanding of heel pain – from plantar fasciitis to Achilles tendinitis, from at-home stretches to medical treatments. Here's what we hope you'll remember: heel pain is a common but treatable condition. You're not stuck with it forever, and you're definitely not alone in dealing with it.
The most important thing we've learned together is that understanding the cause is the first step to recovery. Whether your pain strikes first thing in the morning, after a long day on your feet, or during your favorite activities, knowing what's happening in your heel gives you the power to address it effectively.
Here's the encouraging news: consistent application of conservative treatments is often successful. Most people find significant relief through simple approaches like proper stretching, supportive footwear, ice therapy, and gradual activity modification. It might take some patience – remember, plantar fasciitis can take three to six months to fully resolve – but persistence really does pay off.
Sometimes, though, your heel pain might involve nerve discomfort or muscle tension that needs a little extra attention. That's where targeted topical relief can make a real difference in your daily comfort. When you're dealing with that burning, tingling sensation or persistent ache, having a reliable cream to apply can provide the soothing relief you need between stretches and doctor visits.
At Neuropasil, we understand how frustrating it can be when pain interferes with your daily life. Our specialized nerve pain relief cream is formulated to address exactly these types of discomfort, offering you a gentle yet effective way to manage those challenging symptoms. Think of it as another tool in your heel pain relief toolkit – one that you can use whenever and wherever you need it.
We're so confident that our approach can help complement your healing journey that we're offering a limited-time 25% discount and free shipping on all orders over $29.99, with even more savings available through our convenient subscription options.
Don't let heel pain keep you from living the active, comfortable life you deserve. Take that next step toward relief today. Find lasting relief with Neuropasil Nerve Pain Relief Cream and find how targeted care can support your journey back to pain-free movement.














