What is Peripheral Neuropathy?

Peripheral neuropathy symptoms arise when nerves outside the brain and spinal cord (the peripheral nervous system) become damaged, disrupting communication signals throughout the body.
Common symptoms include:
- Numbness, tingling, or a "pins and needles" feeling, often in the hands or feet.
- Sharp, burning, or throbbing pain.
- Extreme sensitivity to touch (allodynia).
- Muscle weakness, affecting movement or walking.
- Loss of balance or coordination.
- Heat intolerance or abnormal sweating.
Peripheral neuropathy is an "umbrella term" for many nerve conditions affecting various body parts. Globally, it affects about 2.4% of people, with the rate rising to 5-7% for those over 45. The risk increases significantly with age. Understanding these symptoms is the first step toward managing the condition.
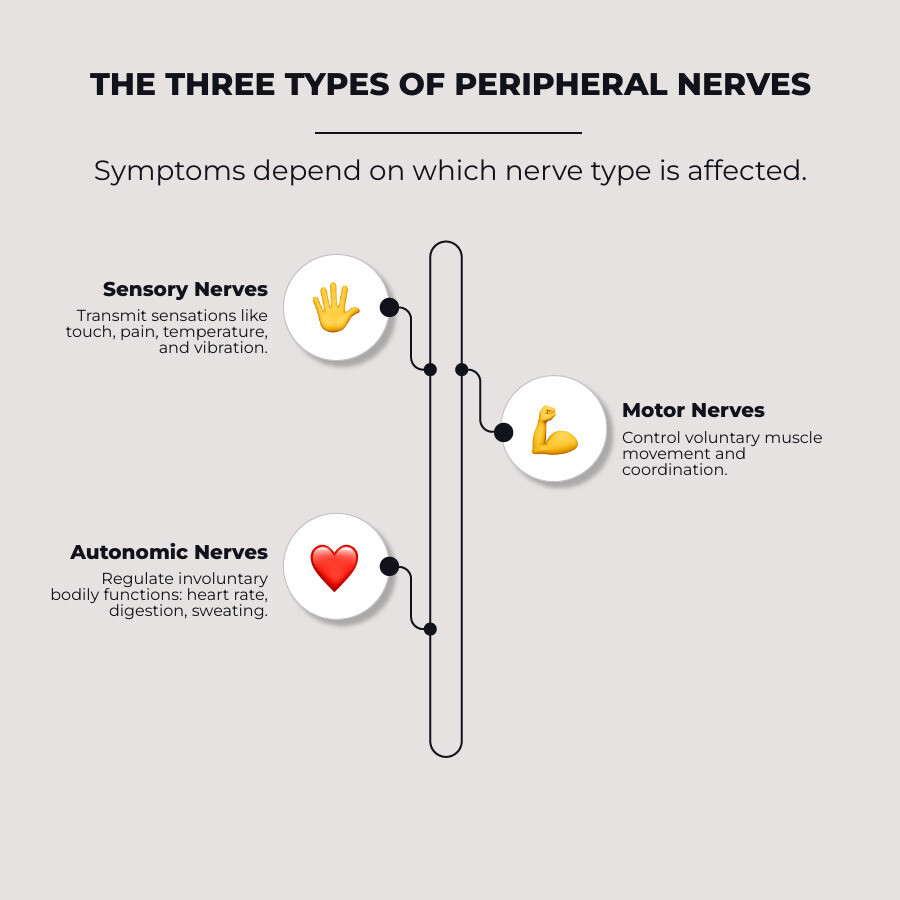
The Three Faces of Nerve Damage: A Guide to Peripheral Neuropathy Symptoms
Peripheral neuropathy symptoms vary widely because our peripheral nervous system has three distinct types of nerves, each with a different job. Damage to these different nerve types leads to different issues.
- Sensory nerves: Transmit sensations like touch, pain, and temperature from the body to the brain.
- Motor nerves: Send signals from the brain to muscles to control movement.
- Autonomic nerves: Control involuntary functions like heart rate, digestion, and blood pressure.
The symptoms you experience depend on which nerve types are affected. For a deeper dive, you can explore resources like Understanding Peripheral Neuropathy Symptoms.
Common Sensory Symptoms
When sensory nerves are damaged, the signals they send can become scrambled, leading to unusual sensations. This is common in conditions like diabetic neuropathy.
- Numbness: A feeling that a limb has "fallen asleep" or a complete loss of sensation. It often starts in the toes or feet.
- Tingling or pins and needles: A persistent prickling sensation, much like a limb "waking up."
- Burning or freezing sensations: Intense burning pain or a persistent icy coldness, even when the skin temperature is normal.
- Sharp, jabbing, or electric-like pain: Sudden, intense shocks or deep, throbbing pain that can be worse at night.
- Extreme sensitivity to touch (allodynia): A condition where a light touch, such as from clothing, causes severe pain.
- Loss of balance and coordination: When nerves can't tell the brain where your limbs are in space (proprioception), it can lead to unsteadiness and an increased risk of falls.
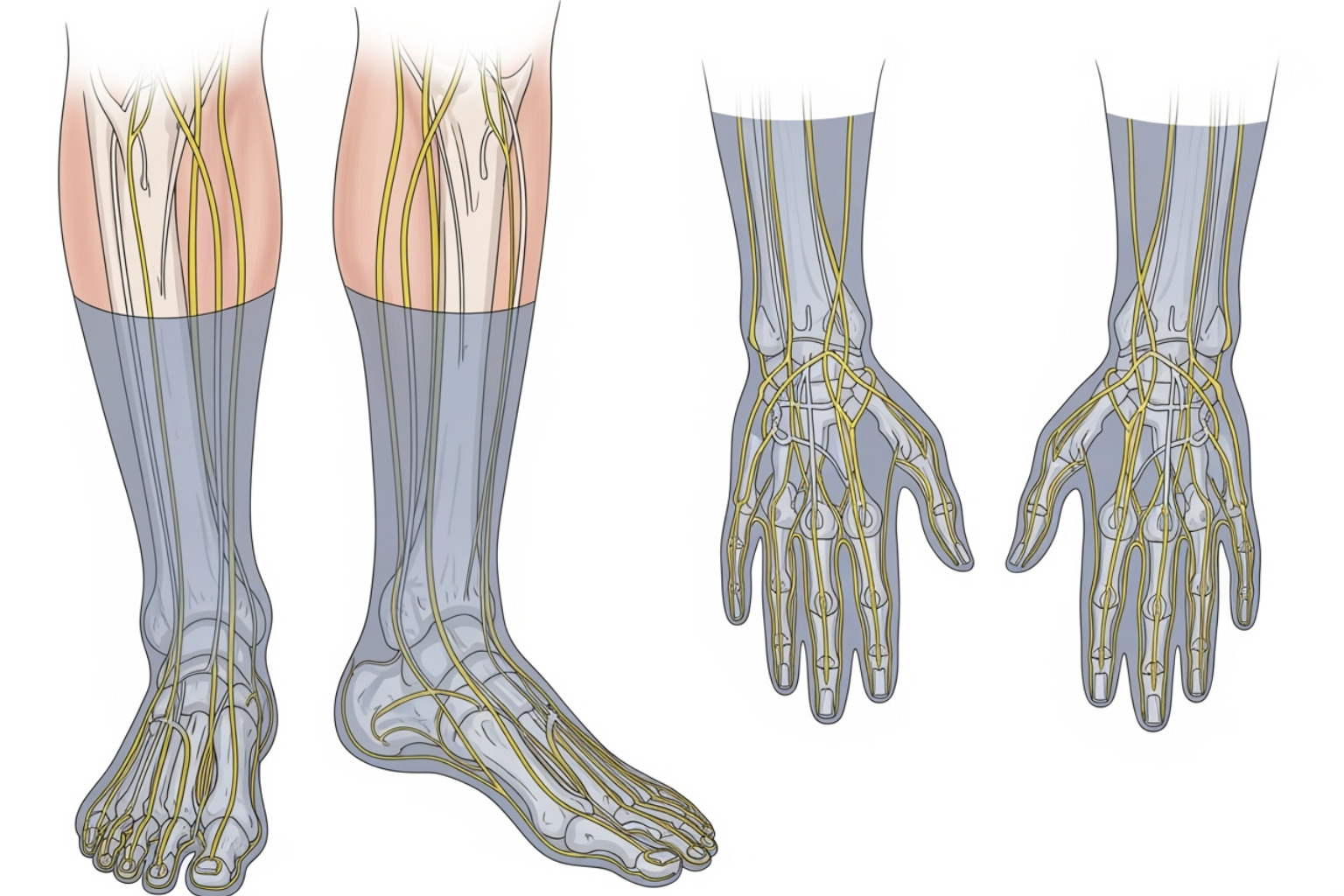
Many of these sensory peripheral neuropathy symptoms follow a "stocking-glove" pattern, starting in the feet and later affecting the hands.
Common Motor Symptoms
Motor nerve damage disrupts signals from the brain to the muscles, impacting movement and function.
- Muscle weakness: Difficulty lifting feet, gripping objects, or standing up from a chair.
- Uncontrolled muscle twitching (fasciculations): Small, involuntary muscle contractions visible under the skin.
- Painful cramps: Sustained, painful muscle contractions, often in the feet, legs, and hands.
- Muscle atrophy (wasting): A noticeable loss of muscle mass over time due to lack of nerve stimulation.
- Difficulty with fine motor tasks: Challenges with buttoning a shirt, writing, or picking up small objects.
- Foot drop: Weakness in the muscles that lift the front of the foot, causing it to drag while walking.
Common Autonomic Symptoms
These symptoms affect the body's automatic functions and can be easily overlooked or misattributed.
- Heat intolerance: Difficulty cooling down due to improper sweat gland regulation.
- Abnormal sweating: Either excessive sweating (hyperhidrosis) or a lack of sweating (anhidrosis).
- Bowel, bladder, or digestive problems: Issues like chronic constipation, diarrhea, nausea, or difficulty emptying the bladder.
- Dizziness from blood pressure changes: Lightheadedness upon standing (orthostatic hypotension) because nerves fail to regulate blood pressure properly.
- Sexual dysfunction: This can include erectile dysfunction in men or issues with arousal or lubrication in women.
Understanding which nerve type is affected helps doctors pinpoint the problem. For more information on managing nerve-related issues, you can explore resources like More info about Neuropathy.
From a Single Nerve to Many: How Neuropathy Type Affects Symptoms
The pattern of your peripheral neuropathy symptoms depends on how many nerves are affected. This helps doctors determine the cause and gives you a clearer picture of your condition. The main types are mononeuropathy (one nerve), polyneuropathy (many nerves), and multiple mononeuropathy (several separate nerves).
For those who want to dive deeper into nerve disorders, you can find comprehensive information at Peripheral Nerve Disorders.
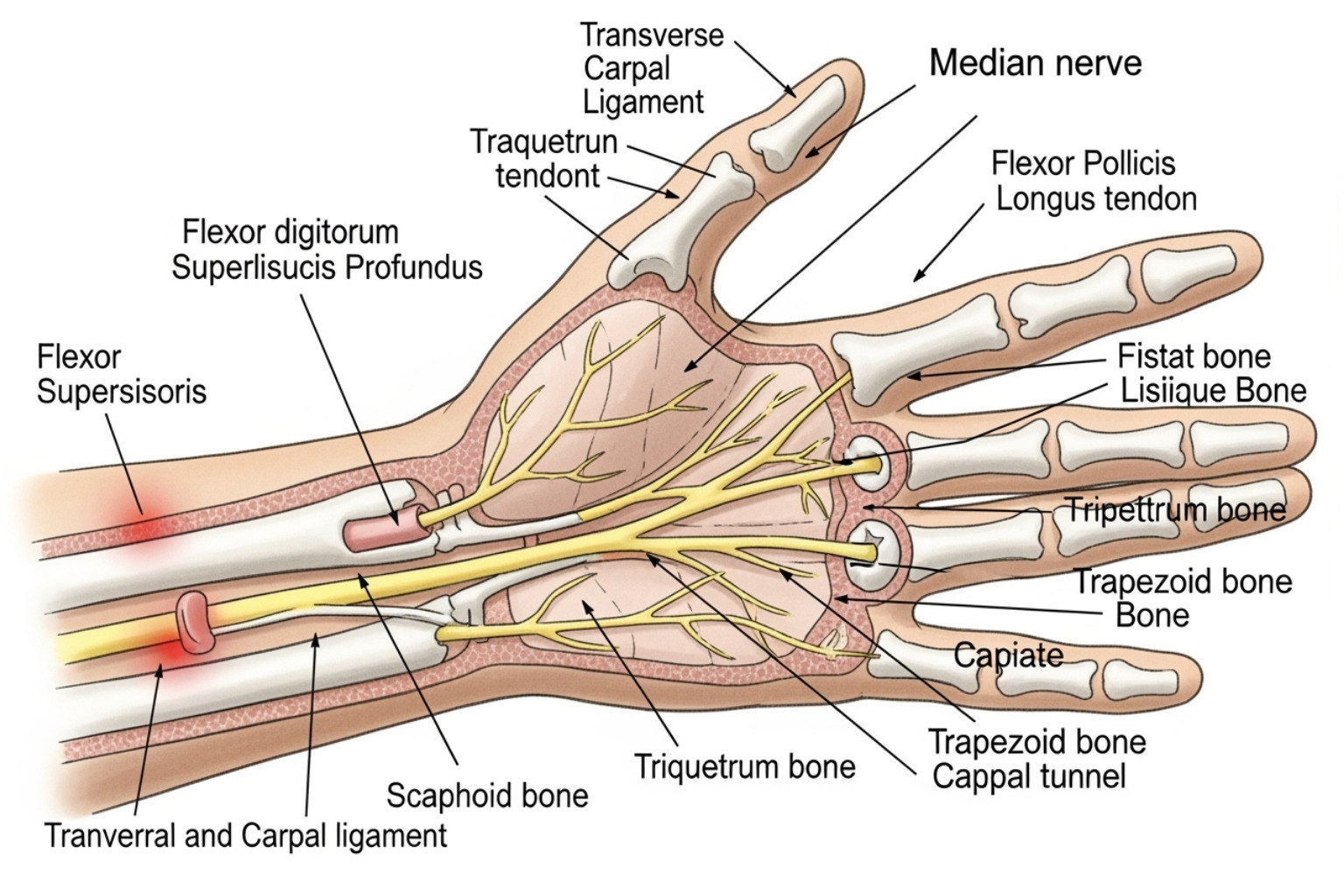
Mononeuropathy: When One Nerve is the Problem
With mononeuropathy, a single nerve is damaged, so symptoms are localized to one specific area. This focused pattern makes it easier to diagnose.
Carpal Tunnel Syndrome is the most common example, where the median nerve in the wrist is compressed. This causes tingling, numbness, and pain in the thumb, index, middle, and part of the ring finger.
Other examples include:
- Ulnar nerve palsy: Compression of the nerve at the elbow (the "funny bone"), affecting the pinky and ring finger and weakening grip strength.
- Peroneal nerve palsy: Occurs near the knee and causes "foot drop," making it difficult to lift the front of the foot.
Because the problem is localized, the cause can often be traced to a specific injury, pressure, or repetitive motion, making treatment more direct.
Polyneuropathy: A Widespread Challenge
Polyneuropathy is the most common type of peripheral neuropathy, where many nerves are affected simultaneously, usually in a symmetrical pattern on both sides of the body.
The classic sign is the "stocking-glove" distribution. Symptoms typically start in the toes (the ends of the longest nerves) and gradually progress up the legs before affecting the hands and arms.
This progression is often gradual, starting with subtle tingling and evolving into numbness or burning pain over time.
Diabetic neuropathy is a primary example of polyneuropathy, affecting more than half of people with diabetes. Years of high blood sugar damage nerve fibers throughout the body. Unlike mononeuropathy, polyneuropathy usually results from systemic conditions like diabetes, autoimmune diseases, or vitamin deficiencies, requiring a more comprehensive management approach.
Progression, Complications, and Early Warning Signs
Peripheral neuropathy symptoms often develop gradually over months or years. This slow onset means nerve damage can be significant by the time symptoms become obvious. That's why understanding the progression and recognizing early signs is crucial for your long-term health.
Fortunately, early diagnosis opens doors to treatments that can slow progression, manage symptoms, and prevent serious complications.
How do peripheral neuropathy symptoms develop and progress?
For most people with polyneuropathy, the onset is gradual. The longest nerves, which run to your toes, are typically the first to show signs of trouble. The progression often follows a predictable pattern:
- Symptoms begin in the feet: The first signs are usually in the toes or balls of the feet, and less commonly in the fingertips.
- Creeping progression: If the underlying cause isn't addressed, symptoms gradually move up the legs and, eventually, to the hands and arms, creating the "stocking-glove" pattern.
- Worse at night: Many people find that nerve pain, tingling, and burning sensations intensify at night, disrupting sleep.
- From occasional to constant: Early on, symptoms may come and go. As nerve damage worsens, they often become more persistent.
Early Warning Signs That Warrant a Doctor's Visit
Listen to your body's warning signals. See a doctor if you experience any of the following:
- Numbness or tingling in your hands or feet, especially if it's symmetrical or spreading.
- Sharp, burning, or electric-like pain that disrupts your sleep.
- Unexplained clumsiness or feeling unsteady on your feet.
- New muscle weakness that makes daily tasks like opening jars or climbing stairs difficult.
- A sore on your foot that won't heal, which is especially serious for people with diabetes.
Trust your instincts. If something feels wrong, it's always best to get it checked out.
Potential Complications of Untreated Symptoms
Ignoring peripheral neuropathy symptoms can lead to serious issues. Taking action early is key to preventing them.
- Chronic pain: What starts as occasional discomfort can become constant, debilitating pain.
- Foot problems: Numbness can cause small cuts or blisters to go unnoticed, leading to serious infections.
- Risk of amputation: Severe, untreated infections from foot injuries can, in the worst cases, require amputation. This is a highly preventable complication.
- Falls and fractures: Poor balance and coordination significantly increase the risk of falls, which can lead to serious injuries like hip fractures.
- Decreased quality of life: The combination of pain, physical limitations, and other symptoms can rob you of simple pleasures and independence.

Most of these complications are preventable with proper medical care, lifestyle changes, and diligent self-monitoring. The key is to act early.
Frequently Asked Questions about Peripheral Neuropathy Symptoms
It's normal to have questions about peripheral neuropathy symptoms. Let's address some of the most common ones to help you understand the condition better.
How are peripheral neuropathy symptoms distinguished from other conditions?
Many conditions can mimic peripheral neuropathy symptoms, so a professional medical diagnosis is essential. Doctors use several steps to identify the cause of your symptoms:
- Medical History: Your doctor will ask detailed questions about your symptoms, overall health, medications, lifestyle, and family health history to find important clues.
- Neurological Exam: This hands-on exam checks your reflexes, muscle strength, balance, coordination, and ability to feel sensations like light touch, pain, and temperature. It helps identify patterns of sensory loss or weakness that suggest nerve damage.
-
Diagnostic Tests: To confirm nerve damage, your doctor may order specific tests:
- Nerve Conduction Study (NCS): Measures the speed and strength of electrical signals traveling through your nerves.
- Electromyography (EMG): Measures electrical activity in your muscles to determine if weakness is caused by a nerve or muscle problem.
- Ruling Out Other Causes: These exams and tests help doctors differentiate peripheral neuropathy from central nervous system disorders like multiple sclerosis or a pinched spinal cord, which can have similar symptoms.
How do underlying conditions like diabetes influence symptoms?
Underlying conditions are a major factor, and diabetes is the leading cause of peripheral neuropathy in the United States. Over time, high blood sugar is toxic to nerves and the small blood vessels that nourish them. This damage often starts in the longest nerves, which is why symptoms typically begin in the feet.
Diabetic neuropathy is a form of polyneuropathy, meaning it affects many nerves symmetrically. This results in the classic "stocking-glove" pattern of sensory loss, with numbness, tingling, and burning pain in both feet that gradually moves up the legs. It can also affect motor and autonomic nerves, causing weakness or digestive issues.
For people with diabetes, strict blood sugar control is the most critical step to prevent or slow the progression of peripheral neuropathy symptoms. For more insights, you might find More info about managing nerve pain helpful.
Can lifestyle choices make symptoms worse?
Yes, lifestyle choices can significantly influence the development and severity of peripheral neuropathy symptoms.
- Alcohol abuse: Excessive alcohol is directly toxic to nerve tissue and can lead to vitamin deficiencies (especially B vitamins) that are crucial for nerve health.
- Vitamin B deficiencies: Nerves rely on B vitamins (like B1, B6, and B12) to function. A deficiency can cause or worsen nerve damage. Conversely, too much vitamin B6 can also cause neuropathy, so balance is key and should be managed with a doctor.
- Smoking and poor circulation: Smoking damages blood vessels, reducing blood flow and the supply of oxygen and nutrients to your nerves, which can worsen nerve damage.
- Exposure to toxins: Certain industrial chemicals, heavy metals, and pesticides can be directly harmful to nerves.
- Repetitive motions: Repetitive stress or prolonged pressure can compress and damage specific nerves, leading to conditions like Carpal Tunnel Syndrome.
Making healthy lifestyle choices gives you an active role in protecting your nerve health.
Conclusion: Taking Control of Your Nerve Health
We've explored the many faces of peripheral neuropathy symptoms, from tingling and burning pain to muscle weakness. We've seen how they vary based on the affected nerves and often begin quietly in the hands and feet.
The most important takeaway is to listen to your body. Persistent numbness, tingling, burning pain, or unexplained weakness are signals that need attention. Seeking prompt medical consultation is your best first step. Early diagnosis can help identify the root cause, allowing for treatment that can slow progression and prevent serious complications like chronic pain, foot ulcers, or dangerous falls.
Managing nerve health also involves tackling underlying causes. For those with diabetes, controlling blood sugar is vital. Healthy lifestyle modifications also make a huge impact: eat a balanced diet, stay active, limit alcohol, and quit smoking. These steps actively support your nerve health.
Living with nerve discomfort is challenging. While professional medical guidance is essential, many people also seek natural solutions. At Neuropasil, we are dedicated to supporting your journey. If you're looking for topical relief from nerve discomfort, we invite you to explore our specialized creams. You can Find natural solutions for nerve pain relief on our website. Taking control of your nerve health is a journey, and we're here to help.














