Understanding the Most Common Cause of Heel Pain

What is plantar fasciitis is one of the most frequently searched questions by people experiencing stabbing heel pain, especially during those first painful steps out of bed each morning.
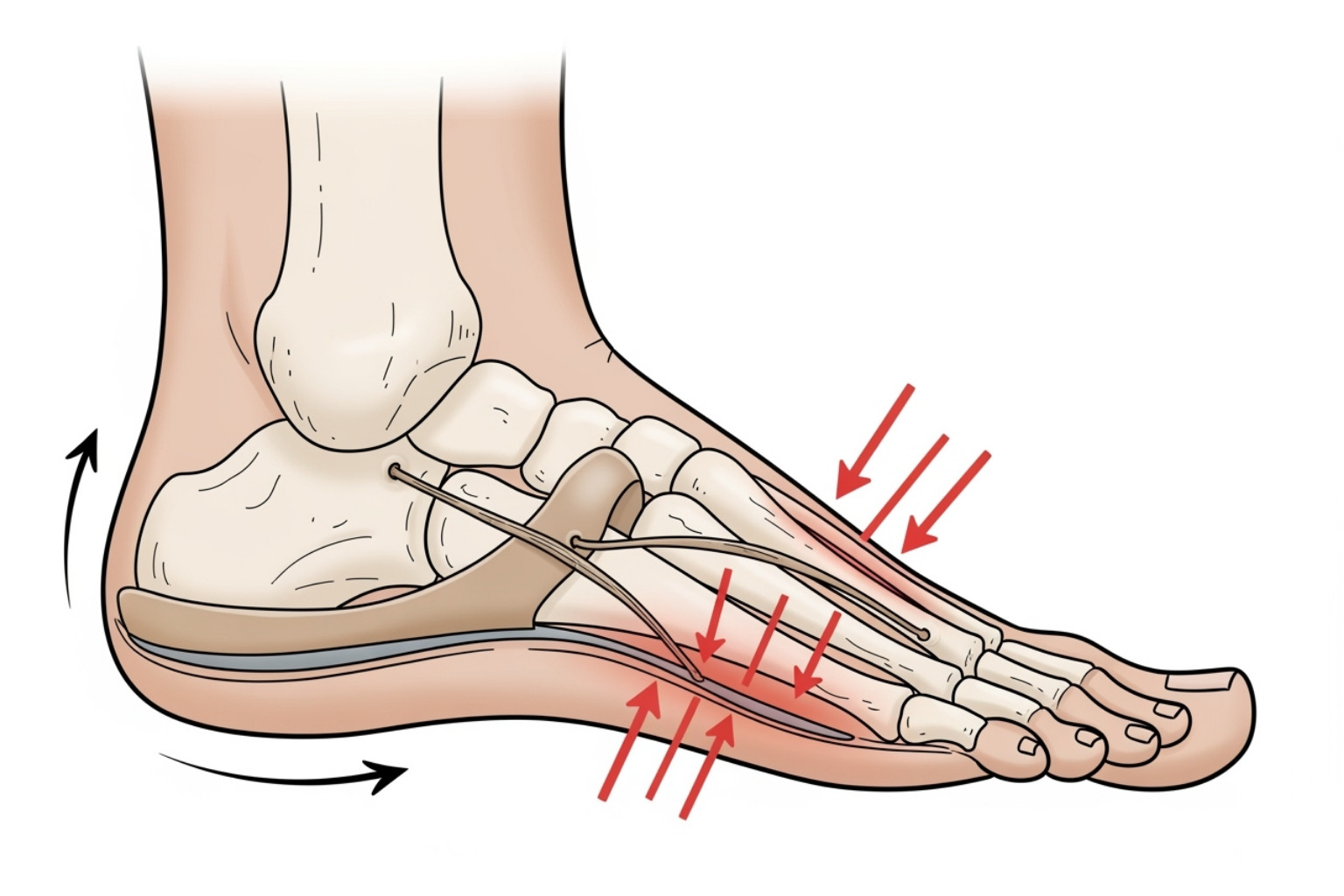
Plantar fasciitis is inflammation of the plantar fascia - a thick band of tissue that runs across the bottom of your foot, connecting your heel bone to your toes. This fibrous tissue supports your foot's arch and acts like a shock absorber during walking and movement.
Here's what you need to know:
- Most common cause: Plantar fasciitis is responsible for heel pain in approximately 2 million Americans each year
- Peak age group: Most common in people between 40-60 years old
- Key symptom: Sharp, stabbing pain in the bottom of the heel, worst with first steps after rest
- Recovery rate: More than 90% of patients improve within 10 months with simple treatments
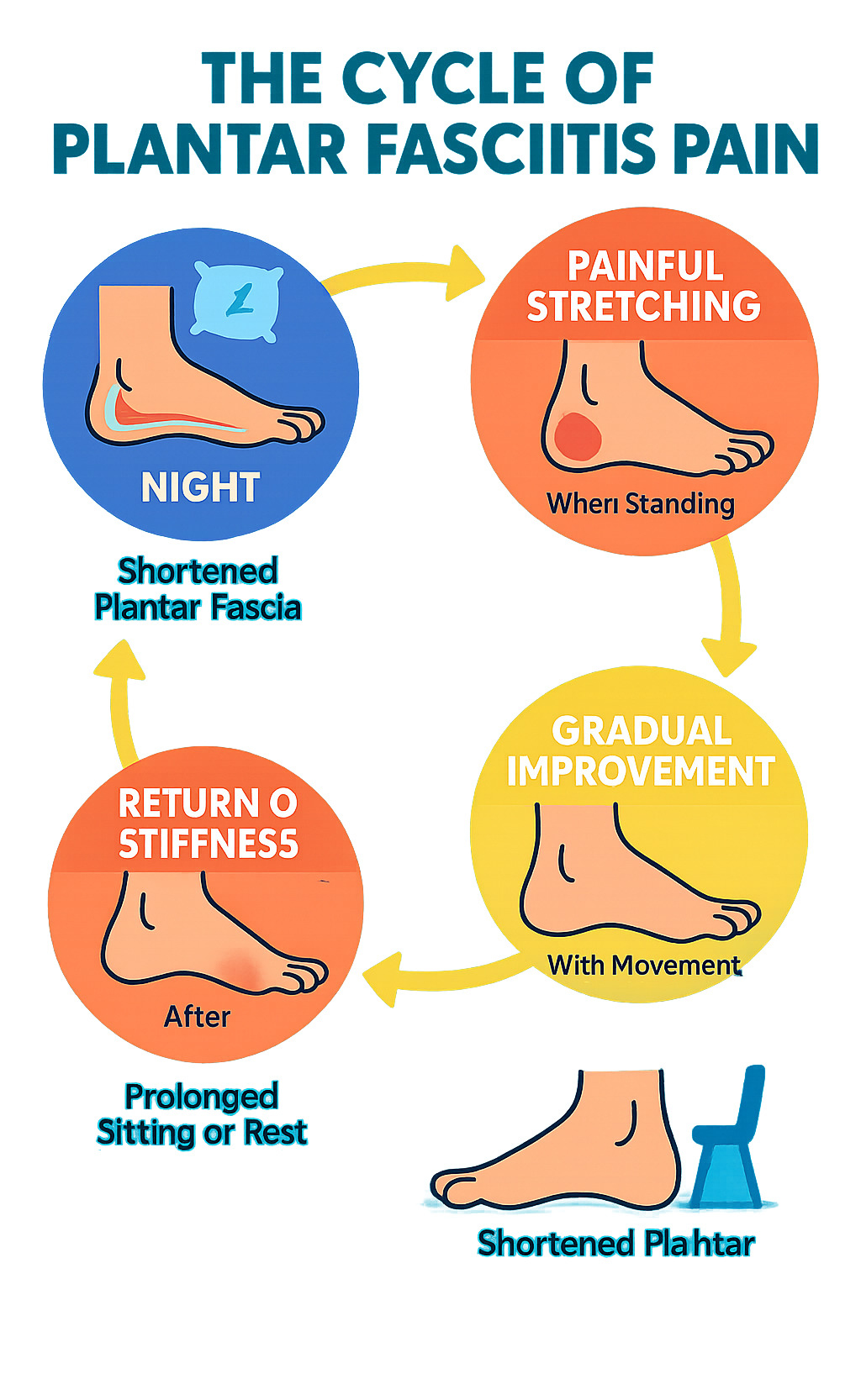
- Pain pattern: Often described as "first-step pain" - severe upon waking or after sitting, then improving with movement
The condition occurs when the plantar fascia becomes overstretched or overused, causing small tears and inflammation near where it attaches to the heel bone. While the exact cause isn't fully understood, repeated stress and tension on this tissue leads to the characteristic heel pain that can make walking difficult.
"Patients often describe the pain as sharp and worse with the first few steps out of bed in the morning," according to medical research. This happens because the plantar fascia tightens during rest and then stretches painfully when you put weight on your foot.
Understanding plantar fasciitis is the first step toward finding relief from this frustrating condition that affects about 1 in 10 people at some point in their lives.
Understanding What is Plantar Fasciitis: Causes and Symptoms
Think of your plantar fascia as nature's built-in shock absorber. This thick, fibrous band of tissue stretches across the bottom of your foot like a bowstring, connecting your heel bone to your toes. Its main job? Supporting your arch and cushioning every step you take.
When this vital tissue gets overworked, you end up with plantar fasciitis - and trust me, your foot will let you know about it.
Here's something interesting that might surprise you: despite the name ending in "-itis" (which usually means inflammation), what is plantar fasciitis is actually more of a degenerative condition than a purely inflammatory one. Recent research shows it's really about tiny tears and breakdown in the tissue - what doctors sometimes call "fasciosis."
This matters because it changes how we think about treatment. Instead of just fighting inflammation, we need to focus on healing those microscopic tears and strengthening the tissue. It's essentially an overuse injury where repetitive strain causes small breakdowns in the fascia over time.
The good news? Studies show this approach works. One study on stretching effectiveness found that heel pain improved by 52% after just eight weeks of plantar fascia stretching. That's the power of helping your tissue heal properly.
Common Symptoms to Watch For
The classic sign of plantar fasciitis is that stabbing heel pain that hits you like a lightning bolt - especially with those first steps out of bed in the morning. You know the feeling: you swing your legs over the side of the bed, put your feet down, and wham - sharp, searing pain right in your heel.
This "morning pain" isn't just limited to when you wake up. You'll likely feel it after any period of rest - getting up from your desk, stepping out of the car after a long drive, or standing up from your favorite chair. It's like your foot "forgets" how to walk again every time you rest.
As you start moving around, the pain often gets better. Your foot seems to "warm up" and loosen up. But here's the tricky part - the pain typically worsens after activity, not during it. You might feel fine during your morning walk, only to have increased pain later in the day.
You might also notice arch pain, stiffness in your foot, or even some mild swelling around the heel area. Some people describe it as feeling like they're walking on a bruise or have a stone in their shoe.
If you're experiencing any unusual pain patterns or suspect nerve involvement might be contributing to your discomfort, it's worth exploring your options. More on managing nerve pain.
What Causes Plantar Fasciitis?
Picture a rubber band that gets stretched over and over again. Eventually, those tiny fibers start to fray and tear. That's essentially what happens with plantar fasciitis - repetitive strain and overstretching of the fascia leads to microscopic damage.
The tension and stress on your plantar fascia builds up over time, creating small tears in the tissue. It's rarely a sudden "pop" like you might get with other injuries. Instead, it's more like the slow wear and tear on your favorite pair of jeans - gradual, but eventually noticeable.
What makes this condition particularly frustrating is that the causes are still poorly understood in many cases. Sometimes it develops without any obvious trigger. Your body is incredibly resilient, but even the best engineering has its limits.
Key Risk Factors
While plantar fasciitis can happen to anyone, certain factors stack the deck against you. Age is a big one - most people who develop it are between 40 and 60 years old. As we get older, our tissues naturally lose some of their bounce-back ability.
If you're into high-impact exercise like running or dancing, you're at higher risk. Runners are particularly prone to this condition, with plantar fasciitis accounting for about 10% of running-related injuries. All that pounding takes its toll.
Your foot mechanics play a huge role too. Whether you have flat feet or high arches, unusual foot structure can change how weight gets distributed across your foot. It's like having uneven tire wear - some parts get more stress than others.
Obesity adds extra strain because your plantar fascia has to support more weight with every step. Think of it as asking your shock absorbers to handle a heavier load than they were designed for.
Certain occupations that require prolonged standing put you at risk too. Nurses, teachers, factory workers, and retail employees often develop plantar fasciitis because their feet get a workout all day long on hard surfaces.
Finally, improper footwear can be the final straw. Those worn-out sneakers with no arch support or those cute but flat sandals might look good, but they're not doing your feet any favors. Your plantar fascia ends up working overtime to make up for what your shoes should be doing.
Getting a Diagnosis and Exploring Treatment
When that sharp heel pain first hits, you might find yourself wondering, "What is plantar fasciitis, and how do I know if that's what I have?" The good news is that getting to the bottom of your heel pain is usually pretty straightforward. Most healthcare providers can diagnose plantar fasciitis through a simple physical examination and by listening to your story about when and how the pain started.
Your doctor will want to rule out other possible causes of heel pain, like stress fractures, nerve compression, or arthritis. Think of it as detective work – they're gathering clues to solve the mystery of your foot pain. If you need help finding a specialist in your area, you can Find an Orthopaedist through this helpful directory.
How Doctors Diagnose Plantar Fasciitis
Your appointment will likely start with a conversation. Your doctor will ask about your symptoms – when did the pain begin, what makes it better or worse, and what your typical day looks like. They're particularly interested in that telltale morning pain pattern.
During the physical exam, your doctor will gently press on different areas of your heel, especially where the plantar fascia attaches to your heel bone. This spot is often quite tender if you have plantar fasciitis. They'll also check your foot structure and watch how you walk. Your gait can reveal a lot about what's causing your pain.
Most of the time, imaging tests like X-rays or MRIs aren't needed. Your doctor can usually diagnose plantar fasciitis based on your symptoms and physical exam alone. However, if they suspect something else might be going on – like a stress fracture or nerve problem – they might order additional tests to be thorough.
Effective Treatment Options for Plantar Fasciitis
Here's some encouraging news: more than 90% of people with plantar fasciitis get better with simple, non-surgical treatments. The key is patience and consistency. Your plantar fascia didn't develop problems overnight, and it won't heal overnight either – but it will heal.
Rest is your friend, even though it might feel frustrating to slow down. You don't have to become a couch potato, but switching from high-impact activities like running to gentler options like swimming can give your foot the break it needs.
Ice therapy works wonders for many people. Try rolling a frozen water bottle under your foot for 15-20 minutes several times a day. It's like getting a mini massage while icing – two benefits in one simple technique.

Stretching might be your most powerful tool. Regular stretching of your plantar fascia, calf muscles, and Achilles tendon can dramatically improve your pain. Some studies show stretching alone can reduce heel pain by over 50%. You'll find some excellent stretching exercises in this helpful guide: Helpful stretches for plantar fasciitis.
Your shoes matter more than you might think. Supportive footwear with good arch support and cushioning can make a huge difference. Avoid walking barefoot on hard surfaces – your feet need that extra support while they're healing. Over-the-counter arch supports or custom orthotics can help distribute pressure more evenly.
Night splints might sound uncomfortable, but many people swear by them. These devices gently stretch your plantar fascia while you sleep, which can significantly reduce that brutal morning pain.
For pain management, topical pain relief creams can provide targeted relief. At Neuropasil, we understand how muscle discomfort and nerve-related pain can complicate your healing journey. Our specialized creams are designed to help with muscle relief, which can be especially helpful when you're dealing with the secondary aches that come from changing how you walk due to heel pain.
Physical therapy can be incredibly valuable, especially if you're not seeing improvement on your own. A physical therapist can teach you proper stretching techniques and create a personalized exercise program.
For stubborn cases, your doctor might suggest corticosteroid injections for temporary relief, though these are used carefully. Newer treatments like platelet-rich plasma (PRP) injections are also being explored.
Surgery is rarely needed – it's typically only considered after 6-12 months of consistent conservative treatment hasn't helped.
When to Seek Medical Attention
While many people can manage their heel pain at home initially, there are times when you shouldn't wait to see a doctor. Contact your healthcare provider if your pain persists after 1-2 weeks of home care. Don't try to tough it out – early treatment often leads to faster recovery.
Seek immediate medical attention if you experience severe pain that makes walking impossible, signs of infection like fever or redness around your heel, or any numbness or tingling in your foot. These symptoms could indicate something more serious than typical plantar fasciitis.
Ignoring persistent heel pain can lead to bigger problems. When your heel hurts, you naturally change how you walk, which can create new aches and pains in your knees, hips, or back. It's like a domino effect that's much easier to prevent than to fix later.
For more information about nerve-related foot discomfort and comprehensive pain management strategies, Explore our neuropathy blog for additional insights and tips.
Prevention and Lifestyle Management
Once you've experienced the sharp sting of what is plantar fasciitis, you'll want to do everything possible to keep it from coming back. Think of prevention as an investment in your future comfort – a little effort now can save you months of heel pain later.
The secret to long-term success lies in understanding that your feet need consistent care, not just when they hurt. By making some simple lifestyle adjustments and being proactive about foot health, you can significantly reduce your chances of dealing with this painful condition again.
The Role of Footwear and Weight
Your shoes are either your feet's best friend or their worst nightmare. There's really no middle ground here! Supportive shoes with good arch support are absolutely essential. Look for shoes that cradle your heel with a firm heel counter and provide ample cushioning throughout the sole.
Here's something many people don't realize: athletic shoes lose their support long before they look worn out. Those trusty running shoes that have carried you through countless miles? They might be secretly sabotaging your feet. Replace your athletic shoes every 6-9 months or after 250-500 miles of use – your plantar fascia will thank you.
Avoid walking barefoot on hard surfaces like concrete, tile, or hardwood floors. We know it feels liberating to kick off your shoes, but those hard surfaces put tremendous stress on your plantar fascia. Instead, slip into supportive house shoes or slippers when you're at home.
Maintaining a healthy weight plays a huge role in preventing plantar fasciitis. Every extra pound puts additional stress on your feet – it's simple physics. Even losing just 10 pounds can make a dramatic difference in how your feet feel at the end of the day.

Stretches and Exercises for Prevention
Think of stretching as your daily insurance policy against heel pain. Consistency is your secret weapon – doing these exercises regularly is far more effective than doing them intensively for a few days and then forgetting about them.
Calf stretches are fundamental because tight calf muscles put extra strain on your plantar fascia. Stand facing a wall, place your hands against it, and step one foot back. Keep that back leg straight with your heel on the ground, then lean forward until you feel a good stretch. Hold for 30 seconds and repeat 2-3 times for each leg.
Towel stretches are perfect for morning routines. While sitting with your legs extended, loop a towel around the ball of your foot and gently pull it toward you. Keep your knee straight and feel the stretch through your calf and arch. This is especially helpful first thing in the morning.
The plantar fascia stretch can be a game-changer for preventing that awful "first-step pain." Before getting out of bed or after sitting for a while, cross your affected foot over your other knee. Grab your toes and gently pull them back toward your shin. You'll feel the stretch right in your arch – hold for 10-15 seconds and repeat 10 times.
Strengthening exercises like toe curls and marble pickups might seem simple, but they're incredibly effective. Place a towel on the floor and scrunch it toward you with your toes, or try picking up marbles with your toes and placing them in a cup. These exercises strengthen the small muscles in your feet that support your arch.
Recovery and Outlook
Recovery from plantar fasciitis is rarely a straight line. Some days will feel better than others, and that's completely normal. Most people see significant improvement within several months, though it can take up to a year for complete resolution. The key word here is patience – your body needs time to heal properly.
More than 90% of people improve with simple, conservative treatments like the ones we've discussed. That's an incredibly encouraging statistic! Surgery is rarely needed – only about 5% of cases require surgical intervention, and usually only after trying everything else for months.
Here's what we can't stress enough: consistency with your treatment plan is absolutely crucial. Doing your stretches sporadically or wearing supportive shoes only sometimes won't give you the results you're looking for. Make these habits part of your daily routine, just like brushing your teeth.
Ignoring plantar fasciitis or hoping it will just go away on its own can lead to chronic problems that are much harder to treat. Even worse, when your heel hurts, you naturally change how you walk. This compensation can create a domino effect of problems in your knees, hips, and back. Your body is beautifully interconnected, but that also means problems in one area can ripple throughout your entire system.
The good news? With proper care and attention, you can get back to all the activities you love without that stabbing heel pain greeting you every morning.
Frequently Asked Questions about Heel Pain
When you're dealing with heel pain, questions start piling up fast. We completely understand - it's frustrating when every step hurts, and you just want answers! Let's tackle the most common questions we hear about what is plantar fasciitis and clear up some confusion.
Are plantar fasciitis and heel spurs the same thing?
This mix-up happens all the time, and honestly, it's no wonder people get confused! The short answer is no - they're definitely not the same thing, though they can be related.
Plantar fasciitis is what happens when that thick band of tissue on the bottom of your foot (the plantar fascia) gets irritated and develops tiny tears. It's a soft tissue problem that causes the stabbing pain you feel.
Heel spurs, on the other hand, are actual bony growths that stick out from your heel bone. Think of them as your body's way of responding to chronic stress - like how your hands develop calluses from repetitive work. These spurs often develop as a result of long-standing plantar fasciitis, not the other way around.
Here's the kicker: many people walk around with heel spurs and never feel a thing. Meanwhile, plenty of folks suffering from plantar fasciitis don't have spurs at all. The spur itself rarely causes pain - it's usually just an innocent bystander that shows up on X-rays.
Can plantar fasciitis go away on its own?
Your body is pretty amazing at healing itself, but waiting around for plantar fasciitis to disappear on its own is like hoping your car will fix itself - it might happen, but why take that chance?
Studies show that about 75% of cases may resolve within a year without treatment. That sounds promising until you realize it means you could be hobbling around in pain for 12 months or more! And that's assuming you're in the lucky majority.
Treatment makes a huge difference in how quickly you feel better. Instead of suffering for months, many people start feeling relief within just a few weeks of starting proper care. Plus, ignoring the pain often leads to other problems - you'll start walking differently to avoid the hurt, which can mess up your knees, hips, and back.
Why put yourself through all that when help is available? Early treatment not only gets you back on your feet faster but also prevents the condition from becoming a chronic nightmare.
What is the single best treatment for plantar fasciitis?
We wish we could point to one magic bullet that works for everyone, but plantar fasciitis is a bit more complicated than that. It's like asking what's the best ingredient for cooking - it really depends on what you're making!
That said, if we had to pick the most consistently effective treatment, it would be stretching. Research shows that regular stretching of the plantar fascia and calf muscles can improve heel pain by over 50% in just eight weeks. It's simple, free, and you can do it anywhere.
But here's the thing - a combination approach works best. The most successful treatment plans typically include stretching as the foundation, along with supportive footwear to cushion your steps, rest to let things heal, and pain relief when you need it.
Some people find great relief from topical creams that soothe muscle discomfort and reduce pain. At Neuropasil, we've seen how the right pain relief cream can make a real difference in managing the daily discomfort while your foot heals.
The "best" treatment is really the one you'll stick with consistently. Work with your healthcare provider to find the right mix of therapies that fits your lifestyle and addresses what's causing your specific pain.
Conclusion
After diving deep into what is plantar fasciitis, we hope you're feeling more confident about tackling this frustrating condition. You now know it's not just "heel pain" – it's a degenerative condition affecting that crucial band of tissue supporting your foot's arch. You understand why those first morning steps feel like stepping on glass, and you've learned about the risk factors that might have put you on this painful path.
Most importantly, you're armed with knowledge about effective treatments. The research is clear: more than 90% of people improve with simple, conservative treatments. Whether it's consistent stretching (which studies show can reduce pain by over 50%), wearing supportive shoes, or using topical pain relief creams like those we offer at Neuropasil, you have options that really work.
Early intervention makes all the difference. Don't wait and hope it goes away on its own – the sooner you start treatment, the faster you'll be back to pain-free walking. Consistency is your best friend here. Those daily stretches might seem tedious, but they're your ticket to freedom from heel pain.
We've also seen how lifestyle factors like maintaining a healthy weight and choosing proper footwear can prevent future episodes. Think of these as investments in your long-term foot health – small changes that pay huge dividends.
You're not powerless against plantar fasciitis. With the right approach and a bit of patience, you can overcome this condition and get back to enjoying life without wincing at every step. Your feet carry you through life's trips – they deserve the care and attention we've outlined.
For more health insights and tips on managing pain, visit our blog. Here's to happier, healthier feet!














