Understanding Neuropathy: More Than Just Nerve Pain
Neuropathy, or nerve damage, affects an estimated 20-30 million Americans, making it a widespread neurological condition. Its causes are diverse, ranging from diabetes and alcohol abuse to infections and injuries. The pain, tingling, and numbness it causes can severely impact quality of life.
At its core, peripheral neuropathy is damage to the nerves outside your brain and spinal cord. These nerves form a communication network, relaying sensory information, controlling muscle movement, and regulating involuntary functions. When damaged, these nerves send incorrect signals, leading to symptoms like burning pain, numbness, or muscle weakness. Understanding the neuropathy causes is the first step toward effective management.
Common Neuropathy Causes at a Glance:
| Category | Specific Causes | Key Facts |
|---|---|---|
| Metabolic/Systemic | Diabetes, prediabetes, kidney disease, liver disease | Diabetes causes ~50% of all neuropathy cases |
| Lifestyle | Alcohol abuse, nutritional deficiencies (B12, B1, B6, E) | 66% of chronic alcohol users may develop neuropathy |
| Autoimmune | Lupus, rheumatoid arthritis, Guillain-Barré syndrome, Sjögren's | Immune system attacks peripheral nerves |
| Medications | Chemotherapy, certain antibiotics, heart medications | 30-40% of chemotherapy patients develop neuropathy |
| Infections | HIV/AIDS, Lyme disease, shingles, hepatitis C | Can cause temporary or permanent nerve damage |
| Physical | Trauma, compression (carpal tunnel), repetitive motion | Direct nerve injury or pressure |
| Genetic | Charcot-Marie-Tooth disease (CMT) | Inherited nerve disorders |
| Idiopathic | Unknown cause | About 23% of cases |
I'm Tony Enrico, and through my work with Neuropasil, I've helped thousands find relief from neuropathy. My personal experience with Type 1 diabetes and neuropathy drives my commitment to providing effective, natural, topical solutions that help people stay active.
Neuropathy vs. Neuralgia vs. Radiculopathy
It's easy to confuse nerve-related terms. Here’s a quick breakdown:
- Neuropathy: The general term for nerve damage or dysfunction.
- Neuralgia: A symptom of neuropathy, specifically referring to nerve pain (e.g., sharp, shooting, or burning pain).
- Radiculopathy: A distinct issue caused by a compressed or "pinched" nerve root at the spinal column, often from a herniated disc.
| Feature | Neuropathy | Neuralgia | Radiculopathy |
|---|---|---|---|
| What it is | Nerve damage or dysfunction | Nerve pain | Pinched nerve root in the spinal cord |
| Origin | Damage to peripheral nerves | Symptom of nerve irritation/damage | Compression of spinal nerve roots |
| Example Cause | Diabetes, alcohol abuse | Postherpetic neuralgia (shingles) | Herniated disc, spinal stenosis |
| Symptoms | Numbness, tingling, weakness, pain | Sharp, shooting, burning pain | Pain, numbness, weakness along nerve path |
The Main Neuropathy Causes: From A to Z
Understanding the root cause of your neuropathy is essential for effective treatment. Neuropathy causes are diverse, and identifying your specific trigger allows for targeted action.
Neuropathy is generally sorted into three categories:
- Acquired Neuropathies: The most common type, developing from external factors like systemic diseases (e.g., diabetes), lifestyle choices (e.g., alcohol abuse), infections, or physical trauma.
- Inherited Neuropathies: Genetic conditions passed down through families.
- Idiopathic Neuropathies: Cases where the cause is unknown, accounting for about 23% of diagnoses.
Most neuropathy is acquired, meaning it stems from identifiable causes that can often be managed or treated. Addressing the underlying issue can slow or halt nerve deterioration, and in some cases, allow nerves to heal.
1. Diabetes Mellitus
Diabetes is the single biggest contributor to neuropathy, responsible for approximately 50% of all cases. Chronically high blood sugar damages both the delicate nerve fibers and the small blood vessels that nourish them. This restricts the flow of oxygen and nutrients, causing nerves to malfunction and deteriorate.
Up to half of all people with diabetes will develop some form of neuropathy, and about 1 in 4 will experience nerve pain. The risk increases the longer you've had diabetes, especially with poor blood sugar control. Even prediabetes can initiate nerve damage.
The feet are often affected first, with symptoms like burning, tingling, or numbness. This numbness is dangerous, as injuries or infections may go unnoticed. For more on this, see our guide on Diabetic Foot Pain.
Fortunately, diabetic neuropathy is not inevitable. Tightly controlling blood sugar, maintaining a healthy weight, and staying active can dramatically slow or prevent nerve damage. Early intervention is key.
2. Alcohol Abuse
Following diabetes, chronic alcohol abuse is the second-leading cause of neuropathy. As many as 66% of individuals with chronic alcohol abuse may develop alcoholic polyneuropathy.
The damage occurs in two ways:
- Direct Toxicity: Alcohol is directly toxic to nerve tissue, poisoning the fibers over time.
- Nutritional Deficiencies: Heavy drinking impairs the body's ability to absorb and use essential nutrients, especially B vitamins (thiamine, B6, and B12), which are vital for nerve health.
This combination leads to widespread nerve damage (polyneuropathy), causing symptoms like burning feet, numb hands, and muscle weakness. The most effective treatment is complete abstinence from alcohol, paired with nutritional support to help stop the progression of nerve damage and allow for potential recovery.
3. Autoimmune Diseases
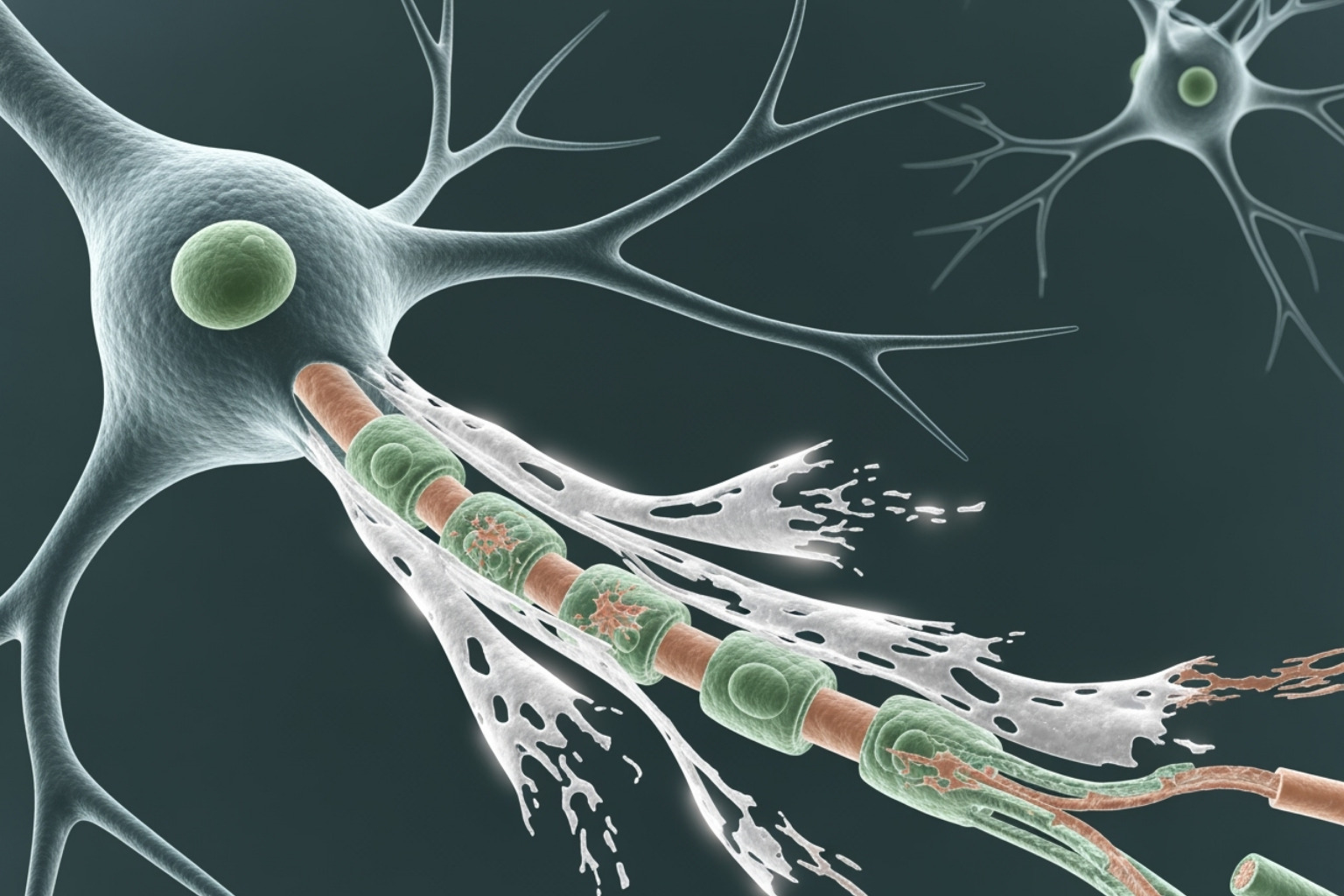
In autoimmune diseases, the immune system mistakenly attacks healthy tissues, including peripheral nerves. This assault can damage nerve fibers or the protective myelin sheath that insulates them, disrupting nerve signals.
Several autoimmune conditions are known to cause neuropathy:
- Lupus and Rheumatoid Arthritis: Can cause inflammation that compresses or damages nerves.
- Guillain-Barré Syndrome: An aggressive condition where the immune system rapidly attacks peripheral nerves, often after an infection.
- Sjögren’s Syndrome: Primarily targets moisture-producing glands but can also damage peripheral nerves.
- Celiac Disease: Gluten consumption triggers inflammation and can lead to poor nutrient absorption, both of which harm nerves.
- Other Culprits: Conditions like sarcoidosis and vasculitis (inflammation of blood vessels) can also reduce blood flow to nerves, causing damage.
Treating the underlying autoimmune condition is crucial to prevent further nerve damage, often requiring immunosuppressive medications.
4. Medications and Treatments
Unfortunately, some medical treatments can inadvertently damage nerves. This is a known side effect of several life-saving therapies.
Chemotherapy-induced peripheral neuropathy (CIPN) is the most common example, affecting an estimated 30-40% of patients. The powerful drugs that kill cancer cells can also harm healthy nerve tissue. While symptoms may resolve after treatment, some individuals experience persistent pain and numbness.
Other medications linked to neuropathy include:
- Certain antibiotics (e.g., metronidazole, nitrofurantoin), especially with prolonged use.
- Some heart medications (e.g., amiodarone).
- Anti-seizure drugs like phenytoin.
It is vital to discuss potential side effects with your doctor before starting a new treatment. If you experience symptoms, your provider may be able to adjust your dosage or find an alternative medication. Never stop taking prescribed drugs without medical guidance.
5. Infections and Viruses
Certain viruses and bacteria can directly attack peripheral nerves or trigger an immune response that harms them.
Key infectious neuropathy causes include:
- HIV/AIDS: Both the virus itself and some antiretroviral medications used to treat it can lead to nerve damage.
- Lyme Disease: Transmitted by ticks, the bacteria can cause inflammation that impacts nerve function if left untreated.
- Shingles (Herpes Zoster): A reactivation of the chickenpox virus that lies dormant in nerve tissue. It can lead to postherpetic neuralgia, a persistent and severe nerve pain. Modern vaccines can prevent over 95% of shingles cases.
- Hepatitis C and West Nile Virus: These viruses can cause body-wide inflammation that affects nerve tissue.
Protecting yourself from infections through vaccinations and prompt treatment is an important step in safeguarding your nerve health.
6. Nutritional and Vitamin Deficiencies
Your nerves require specific vitamins and nutrients to function properly. Deficiencies can lead to nerve deterioration and are often a preventable cause of neuropathy.
Vitamin B12 deficiency is a primary culprit, as B12 is critical for maintaining the protective myelin sheath around nerves. An untreated deficiency can cause irreversible nerve damage.
Other essential nutrients for nerve health include Vitamin B1 (thiamine), Vitamin B6 (pyridoxine), Vitamin E, and niacin. Deficiencies in these can also lead to neuropathy.
However, more is not always better. An excess of Vitamin B6, often from high-dose supplements, can be toxic to nerves and cause neuropathy itself. This highlights the need for a delicate balance.
Malnutrition from a poor diet or malabsorption conditions (like celiac disease) deprives nerves of the raw materials they need. A balanced diet is your first line of defense, and any suspected deficiencies should be evaluated by a healthcare professional before starting supplements.
7. Physical Injury and Trauma
Sometimes, neuropathy is caused by direct physical damage to a nerve. Nerves can be compressed, crushed, stretched, or severed, disrupting their ability to function.
- Nerve Compression: This is one of the most common injuries. A well-known example is carpal tunnel syndrome, where the median nerve in the wrist is squeezed, causing numbness and tingling in the hand. Another is ulnar neuropathy, affecting the nerve at the elbow (the "funny bone").
- Accidents and Sports Injuries: Falls, car accidents, or bone fractures can directly sever, stretch, or crush nerves.
- Repetitive Motion: Jobs or hobbies involving repetitive movements (e.g., typing, using vibrating tools) can put chronic stress on nerves, leading to entrapment neuropathies over time.
- Surgery: Nerves near a surgical site can occasionally be damaged during a procedure.
These injuries typically cause mononeuropathy (damage to a single nerve). If the source of pressure is removed or the injury heals, nerve function can often improve, though regeneration is a slow process.
Inherited and Idiopathic Neuropathy Causes
Beyond acquired conditions, some neuropathies are genetic, while others have no identifiable cause.
1. Hereditary Neuropathies
Some people inherit genetic mutations that predispose them to nerve damage. These hereditary neuropathies are passed down through families.
The most common is Charcot-Marie-Tooth disease (CMT), an inherited neurological disorder. CMT causes progressive muscle weakness and sensory loss, typically starting in the feet and legs and later affecting the hands and arms. It damages either the nerve fibers or their protective myelin sheath.
Symptoms often appear in childhood or adolescence, such as clumsiness or an unusual gait. While there is no cure for CMT, many people lead full lives with the help of physical therapy, occupational therapy, and supportive devices like braces. Genetic counseling can provide valuable information for families with a history of the disease.
2. Idiopathic Neuropathy
Sometimes, despite extensive testing, doctors cannot find a specific reason for nerve damage. This is called idiopathic neuropathy, and it accounts for roughly 23% of all neuropathy cases.
"Idiopathic" means the origin is unknown. It is a diagnosis of exclusion, made after all known neuropathy causes—like diabetes, alcohol abuse, and vitamin deficiencies—have been ruled out.
An idiopathic diagnosis can be frustrating, but it does not mean your symptoms aren't real or that nothing can be done. Treatment simply shifts focus from curing an underlying condition to effectively managing your symptoms. This includes pain relief strategies, physical therapy, and lifestyle modifications to maintain the best possible quality of life. Medical science is constantly evolving, and what is considered idiopathic today may have a known cause tomorrow.
Identifying the Problem: Symptoms, Types, and Diagnosis
Recognizing the signs of neuropathy and getting a proper diagnosis are crucial for effective treatment. The pattern of your symptoms provides important clues to the underlying cause.
Types of Neuropathy and Their Symptoms
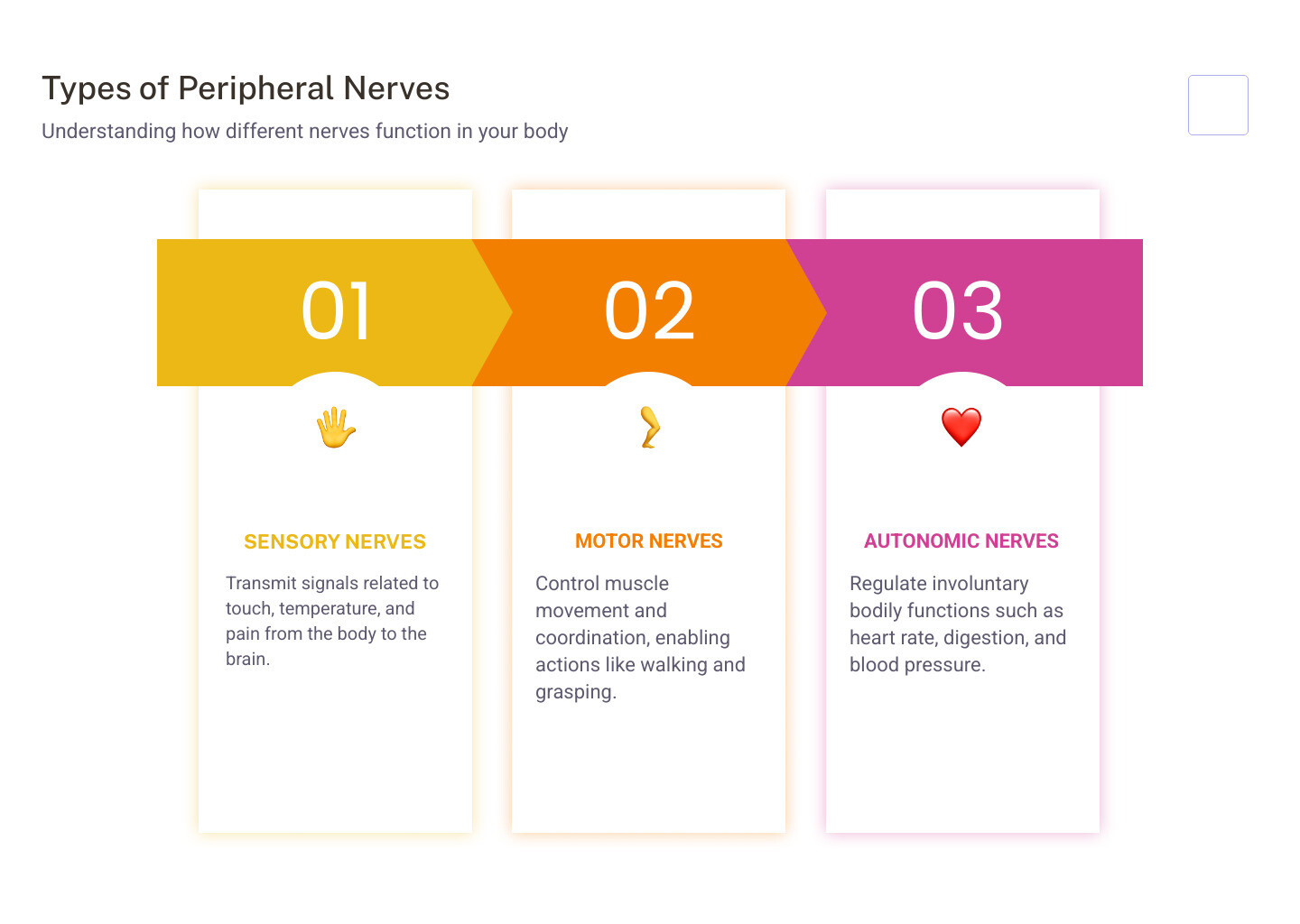
Neuropathy is classified based on which nerves are affected:
- Sensory Neuropathy: Affects nerves for touch, temperature, and pain. Symptoms include numbness, tingling, burning pain, extreme sensitivity to touch, and loss of balance or coordination.
- Motor Neuropathy: Impacts nerves controlling muscle movement. Symptoms include muscle weakness, lack of coordination, foot drop (difficulty lifting the front of the foot), and muscle atrophy (wasting).
- Autonomic Neuropathy: Affects nerves controlling involuntary functions. Symptoms can include dizziness upon standing, digestive issues (nausea, bloating, constipation), abnormal sweating, and bladder or sexual dysfunction.
Damage can affect a single nerve (mononeuropathy, e.g., carpal tunnel) or multiple nerves throughout the body (polyneuropathy, e.g., diabetic neuropathy), which often appears in a "stocking-glove" pattern starting in the hands and feet.
How Doctors Diagnose Neuropathy
Diagnosing neuropathy involves a multi-step process to identify the underlying cause:
- Medical History and Physical Exam: Your doctor will ask about your symptoms, lifestyle, and family history, and perform a neurological exam to check reflexes, muscle strength, and sensation.
- Blood Tests: These are crucial for identifying common causes like diabetes, vitamin deficiencies (especially B12), kidney or liver disease, and autoimmune markers.
-
Nerve Function Tests:
- Electromyography (EMG): Measures electrical activity in muscles to see if weakness is due to nerve or muscle issues.
- Nerve Conduction Velocity (NCV): Measures how quickly electrical signals travel through nerves, helping to identify damage to the nerve fiber or its protective myelin sheath.
- Additional Tests: In some cases, a nerve biopsy (examining a small nerve sample) or imaging scans like an MRI (to check for compressed nerves) may be necessary.
Managing Neuropathy: Treatment and Prevention
Once the neuropathy causes are identified, you can take action to halt progression, manage symptoms, and improve your quality of life.

Medical and Therapeutic Treatments
Effective treatment starts by addressing the root cause, such as controlling blood sugar in diabetes or stopping alcohol consumption.
- Pain Management: Prescription medications like anticonvulsants (gabapentin, pregabalin) and certain antidepressants are often effective for nerve pain.
- Topical Treatments: Creams and patches can provide targeted relief with fewer systemic side effects. Products with lidocaine or capsaicin are common. Our Neuropasil cream uses a combination of Aloe, Urea, and Menthol to soothe damaged nerves and relieve burning and tingling sensations.
- Physical and Occupational Therapy: Therapy can strengthen weakened muscles, improve balance to reduce fall risk, and teach adaptive strategies for daily tasks.
For more on diabetic neuropathy, see our guide on 7 Proven Diabetic Neuropathy Treatments for Fast Relief.
Lifestyle Changes and Prevention Strategies
Daily habits have a powerful impact on nerve health.
- Eat a Balanced Diet: A diet rich in fruits, vegetables, and whole grains provides the B vitamins, vitamin E, and other nutrients essential for nerve repair.
- Exercise Regularly: Physical activity improves circulation, helps manage weight, and strengthens muscles, which improves balance. Aim for 30-60 minutes of moderate activity three times a week, with your doctor's approval.
- Avoid Smoking and Limit Alcohol: Smoking constricts blood vessels, reducing blood flow to nerves. Limiting or eliminating alcohol is critical, especially if it's a cause of your neuropathy.
- Practice Meticulous Foot Care: If you have numbness in your feet, inspect them daily for injuries, wear protective shoes, and keep them clean and moisturized.
- Manage Chronic Conditions: Proactively manage conditions like diabetes and high blood pressure to prevent them from causing nerve damage.
- Avoid Toxins: Use proper protective equipment if your work exposes you to industrial chemicals or heavy metals.
Frequently Asked Questions about Neuropathy Causes
Here are answers to some of the most common questions about neuropathy causes.
Can neuropathy be reversed?
It depends on the cause and how early it's treated. If neuropathy is caused by a fixable issue like a vitamin B12 deficiency or a medication, symptoms can often improve or resolve. Peripheral nerves have a limited ability to regenerate, but the process is slow.
However, for advanced or trauma-induced neuropathy, complete reversal is less likely. In these cases, the focus shifts to managing symptoms and preventing further damage. Topical solutions like Neuropasil can provide significant daily comfort even when the underlying damage is permanent.
Is neuropathy always painful?
No. While burning, shooting, or stabbing pain is a common symptom, neuropathy can manifest in other ways. Many people experience numbness, tingling ("pins and needles"), or a complete loss of sensation. Others struggle primarily with muscle weakness, poor coordination, or balance problems due to a lack of feeling in their feet. Autonomic neuropathy can cause issues with digestion, blood pressure, or sweating without any pain.
What is the most common cause of neuropathy?
Diabetes is by far the leading cause, responsible for about half of all neuropathy cases. Consistently high blood sugar damages both the nerves and the small blood vessels that supply them with oxygen and nutrients. The risk increases the longer a person has diabetes and the poorer their blood sugar control. Managing blood sugar through diet, exercise, and medication is the most effective way to prevent or slow the progression of diabetic neuropathy.
Conclusion: Taking Control of Your Nerve Health
Understanding the neuropathy causes behind your symptoms is the first step toward taking control. Whether it's diabetes, alcohol abuse, an autoimmune condition, or another trigger, early diagnosis is critical for slowing progression and managing discomfort.
Medical treatments are essential, but so are daily lifestyle choices. A nutrient-rich diet, regular exercise, and avoiding smoking and excess alcohol create a strong foundation for nerve health.
At Neuropasil, our mission is to provide immediate, targeted relief from the symptoms that disrupt your life. Our topical creams, formulated with Aloe, Urea, and Menthol, are designed to soothe damaged nerves and ease burning, tingling, and numbness.
Don't let nerve pain limit you. By addressing root causes, making smart lifestyle choices, and using effective symptom management tools, you can significantly improve your quality of life.
Ready to find relief? Explore our Nerve Pain Relief Cream and visit our blog for more practical advice. Your nerve health matters, and relief is possible.
References
Throughout this comprehensive guide on neuropathy causes, we've drawn on research from leading medical institutions, health organizations, and clinical studies to ensure you receive accurate, reliable information. Understanding nerve damage and its origins requires a foundation built on credible medical knowledge, and we're committed to transparency about where our information comes from.
The statistics and medical insights shared here come from respected sources including the University of Michigan Health system, which provided valuable data on peripheral nerve disorders and the prevalence of various conditions. Their neurology health blog offered particularly helpful context about neuropathy's second-leading cause. We also referenced their resources on prediabetes and diabetes management, given diabetes's overwhelming role in neuropathy cases.
For information on specific conditions and their connection to nerve damage, we consulted Everyday Health's comprehensive guides on Type 2 Diabetes, Lupus, Rheumatoid Arthritis, Guillain-Barré Syndrome, Sjögren's Syndrome, Celiac Disease, Sarcoidosis, HIV/AIDS and its treatment options, infectious diseases, and Shingles. These resources helped us paint a complete picture of autoimmune and infectious neuropathy causes.
The Foundation for Peripheral Neuropathy provided invaluable insights into what peripheral neuropathy is and the various causes of this condition, including the sobering statistic that 66% of chronic alcohol users may develop alcoholic polyneuropathy. Cleveland Clinic's overview of peripheral neuropathy and Piedmont Healthcare's article on the most common causes rounded out our understanding of this complex condition.
For nutritional and medication-related causes, WebMD served as a trusted resource for information about Vitamin B12 and Carpal Tunnel Syndrome. MedlinePlus offered clear explanations of conditions like Ulnar Neuropathy.
The National Institute of Neurological Disorders and Stroke (NINDS) provided authoritative information on Charcot-Marie-Tooth Disease and their comprehensive Peripheral Neuropathy Fact Sheet, which includes details on shingles prevention and treatment options.
For diagnostic procedures, we referenced Medical News Today's explanation of Electromyogram (EMG) and nerve conduction velocity (NCV) tests. Information about peripheral neuropathy causes and prevalence also came from NHS UK resources.
We're grateful to these medical institutions and health organizations for making quality information accessible to everyone. Their research and clinical insights form the backbone of our commitment to helping you understand neuropathy causes and find effective relief. If you're dealing with nerve pain, always consult with your healthcare provider about your specific situation—these references can serve as a starting point for informed conversations with your medical team.













