Why Understanding Side Calf Pain Matters
Pain on side of calf is a common complaint that can stop you in your tracks—whether you're mid-run, climbing stairs, or just walking around your home. This discomfort isn't always straightforward. The side of your calf houses important muscles, tendons, nerves, and blood vessels, and pain in this area can stem from anything from a simple muscle strain to a more serious vascular or nerve issue.
Quick Answer: Common Causes & Relief for Pain on Side of Calf
- Muscular Issues: Peroneal tendonitis, gastrocnemius or soleus strain, muscle cramps (affecting an estimated 37% of people)
- Nerve Problems: Sciatica, peroneal nerve entrapment, diabetic neuropathy
- Serious Conditions: Deep vein thrombosis (DVT), peripheral artery disease (PAD), compartment syndrome, fibula stress fracture
- Immediate Relief: R.I.C.E. method (Rest, Ice, Compression, Elevation), gentle stretching, topical pain relief
- When to Seek Help: Sudden severe pain, swelling with redness and warmth, inability to bear weight, numbness or weakness
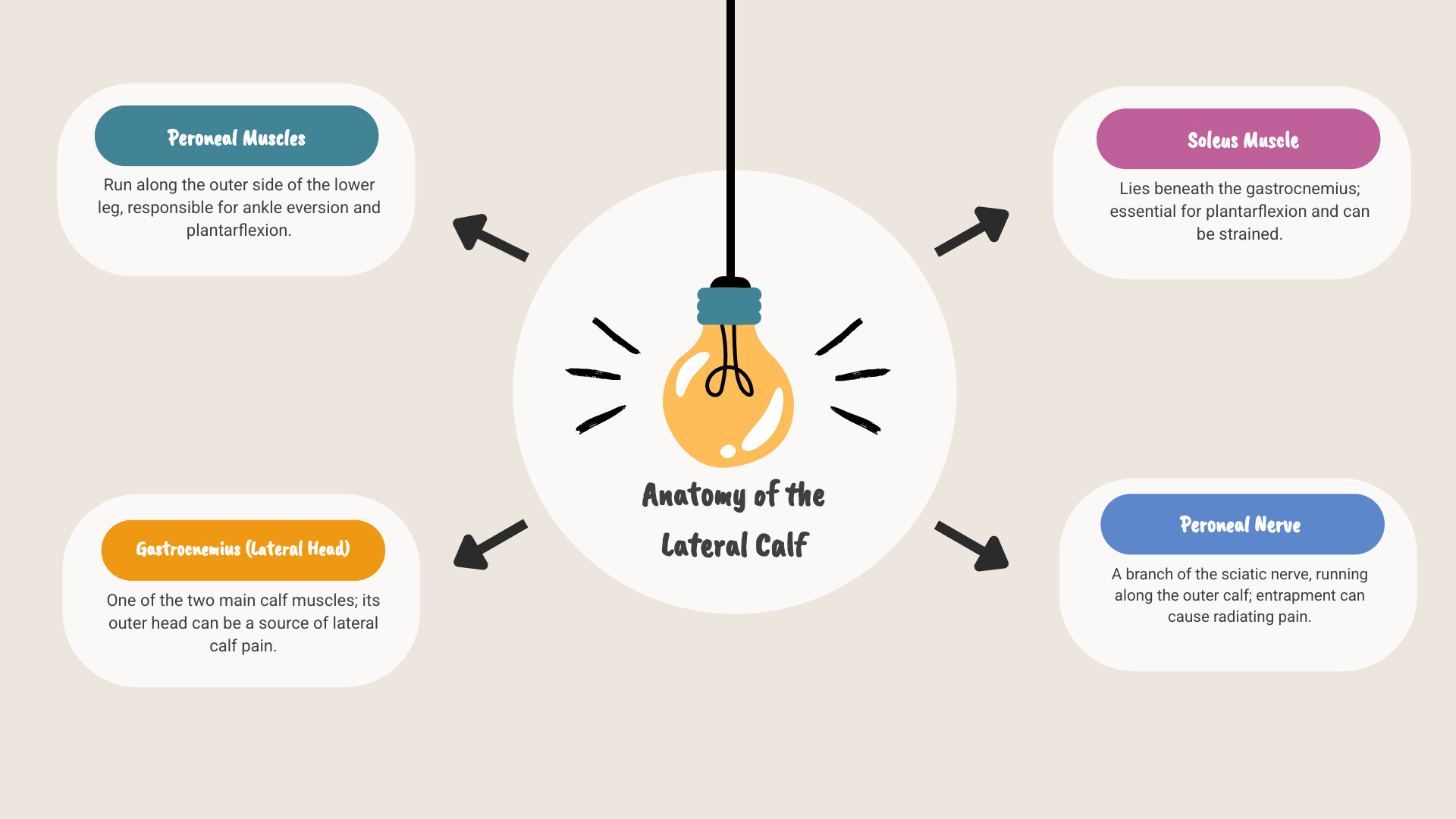
The calf is made up of several key structures. The gastrocnemius and soleus muscles form the bulk of your calf, while the peroneal muscles run along the outer side of your lower leg. When pain strikes the side of your calf—the lateral area—it often involves these peroneal muscles, the outer head of the gastrocnemius, or related tendons and nerves.
This guide will walk you through the most common and serious causes of side calf pain, how to recognize warning signs, and what steps you can take for relief and recovery.
I'm Tony Enrico, and through my work with Neuropasil, I've seen how debilitating pain on side of calf can be for athletes, workers, and anyone trying to stay active. My mission is to help people understand their pain and find natural, effective relief so they can keep moving forward.
What Causes Pain on the Side of the Calf?
When we experience pain on side of calf, it’s our body’s way of telling us something is amiss. This area of the lower leg is complex, involving muscles, tendons, bones, nerves, and blood vessels, all of which can be sources of discomfort. Let's explore the common culprits and some of the more serious conditions that might be causing your lateral calf pain.
Common Muscular and Tendon Issues
The most frequent causes of pain on side of calf often involve the muscles and tendons located in the lateral compartment of the lower leg. These issues typically arise from overuse, sudden movements, or direct trauma.
- Peroneal Tendonitis: The peroneal muscles (peroneus longus and brevis) run along the outside of your lower leg, connecting to the foot. Their tendons can become inflamed, leading to peroneal tendonitis, especially with repetitive ankle movements or inadequate support. This condition causes pain, swelling, and tenderness along the outside of the ankle and lower leg, often worse with activity.
- Gastrocnemius Strain (lateral head): The gastrocnemius is one of the two main calf muscles. Its lateral head, located on the outer side, can be strained or torn, particularly during explosive movements like jumping or sprinting. A strain can feel like a sudden sharp pain, tenderness, and sometimes swelling or bruising in the affected area. Many calf strains heal on their own within a few weeks, but others may need treatment and a longer recovery period. You can learn more about calf strains from Sports Medicine Australia.
- Soleus Muscle Strain: While the soleus muscle lies beneath the gastrocnemius, a strain in this deeper muscle can also manifest as pain on side of calf. Soleus strains are often associated with endurance activities like long-distance running, causing a deep ache or tightness that worsens with continued activity.
- Muscle Cramps: These sudden, involuntary, and often intense contractions of the calf muscles are incredibly common, affecting an estimated 37% of all people. While they can occur anywhere in the calf, they can certainly strike the side. Dehydration, electrolyte imbalances, muscle fatigue, or holding a position for too long are common triggers.
- Contusion (bruise): A direct blow or impact to the side of the calf can cause a contusion. This injury results in localized pain, tenderness, swelling, and often discoloration (bruising) as small blood vessels beneath the skin rupture.

Less Common but More Serious Causes
While most instances of pain on side of calf are due to musculoskeletal issues, it's crucial to be aware of less common but potentially more serious conditions. These require immediate medical attention.
- Deep Vein Thrombosis (DVT): DVT is a serious condition where a blood clot forms in a deep vein, often in the calf. Symptoms can include swelling, redness, warmth, and a tender, cramping pain in the affected leg. It's an emergency because the clot can break loose and travel to the lungs, causing a pulmonary embolism. If you suspect DVT, seek immediate medical care.
- Peripheral Artery Disease (PAD) / Arterial Claudication: PAD involves the narrowing of arteries that supply blood to the legs, often due to atherosclerosis. This can lead to a condition called arterial claudication, where you experience calf pain or cramping during physical activity (like walking) that eases with rest. This occurs because the muscles aren't receiving enough oxygen-rich blood. You can find more information about peripheral arterial disease from NCBI.
- Chronic Exertional Compartment Syndrome: This condition occurs when exercise causes pressure to build up within the muscle compartments of the lower leg. While it can affect various compartments, the lateral compartment can be involved, leading to pain on side of calf, tightness, numbness, or weakness during activity. The symptoms typically subside shortly after stopping the activity.
- Fibula Stress Fracture: The fibula is the smaller bone on the outer side of your lower leg. Repetitive stress, common in runners or those involved in high-impact sports, can lead to tiny cracks in the fibula, known as a stress fracture. This causes localized pain on the side of the calf that worsens with activity and improves with rest.
To help you distinguish between some of these conditions, here's a quick comparison:
| Symptom/Condition | Muscle Strain | Deep Vein Thrombosis (DVT) | Peripheral Artery Disease (PAD) |
|---|---|---|---|
| Onset | Often sudden | Can be sudden or gradual | Gradual |
| Pain Character | Sharp, localized, aching | Aching, cramping, tenderness | Cramping, fatigue, tightness |
| Relation to Activity | Worse with movement, specific actions | May worsen with standing/walking | Worse with activity, relieved by rest |
| Swelling | Possible, localized | Often significant, one-sided | Minimal or absent |
| Redness/Warmth | Possible | Often present | Pale or bluish skin, cool to touch |
| Other Symptoms | Bruising, weakness | Veins may be prominent | Hair loss, shiny skin, weak pulse |
| Urgency | Moderate | EMERGENCY | High |
Nerve-Related Side Calf Pain
Nerve issues can also be a significant source of pain on side of calf. When nerves are compressed, irritated, or damaged, they can send pain signals, along with other sensations, to the areas they supply.
- Sciatica: Sciatica occurs when the sciatic nerve, which originates in the lower back and extends down the leg, becomes compressed or irritated. While commonly associated with pain down the back of the leg, the nerve branches can refer pain to the lateral calf. Symptoms often include a burning sensation, tingling, numbness, or weakness, often radiating from the lower back down the leg.
- Peroneal Nerve Entrapment: The common peroneal nerve wraps around the outside of the knee and then branches into superficial and deep peroneal nerves. These nerves supply sensation to the outer calf and top of the foot, and control muscles that lift the foot. If this nerve gets compressed or entrapped, it can cause pain on side of calf, numbness, tingling, and sometimes "foot drop," where you have difficulty lifting the front part of your foot. You can learn more about common peroneal nerve dysfunction from Mount Sinai.
- Diabetic Neuropathy: For individuals with diabetes, high blood sugar levels can damage nerves throughout the body, including those in the legs. This condition, known as diabetic neuropathy, can cause numbness, tingling, burning, or sharp pain on side of calf, often starting in the feet and progressing upwards. Information on diabetic neuropathy highlights the importance of managing blood sugar to prevent such complications.
- Symptoms: When nerve pain is involved, you might experience not just pain, but also sensations like radiating pain, numbness, tingling, or even a feeling of pins and needles. This can often be confused with muscle pain, making proper diagnosis essential.
How to Find Relief: Diagnosis, Treatment, and Home Care
When pain on side of calf strikes, our first thought is often how to make it stop. However, because the causes can range from minor muscle soreness to serious medical emergencies, getting a proper diagnosis is the crucial first step.
Getting a Proper Diagnosis
A thorough medical evaluation is essential to determine the exact cause of your pain on side of calf. Our healthcare providers will typically follow a systematic approach:
- Physical Examination: Your doctor will observe your gait, check for swelling, tenderness, bruising, and assess your range of motion and muscle strength. They might perform specific tests to pinpoint the source of pain, such as checking for nerve impingement or tendon integrity. For a general idea of what to expect, you can review information on musculoskeletal exams from painHEALTH.
- Medical History: We'll ask you detailed questions about your symptoms, including when the pain started, its intensity, what makes it better or worse, any recent injuries, your activity levels, and any underlying health conditions (like diabetes or vascular issues).
-
Imaging Tests: Depending on the suspected cause, your doctor might order imaging.
- Ultrasound: Often used to visualize soft tissues like muscles and tendons, and can be very effective in identifying blood clots (DVT).
- MRI (Magnetic Resonance Imaging): Provides detailed images of soft tissues, bones, and nerves, useful for diagnosing muscle tears, stress fractures, compartment syndrome, or nerve compression.
- X-ray: Primarily used to check for bone fractures or abnormalities.
- Blood Tests: If DVT is suspected, a D-dimer blood test might be performed to check for fragments of blood clots. Other blood tests might assess for inflammation or other systemic conditions.
Immediate At-Home Care for Pain on the Side of the Calf
For many common causes of pain on side of calf, especially those due to minor strains or overuse, immediate at-home care can provide significant relief. We often recommend the R.I.C.E. method:
- Rest: Avoid activities that aggravate your pain. Give your calf muscles time to heal.
- Ice: Apply an ice pack or cold compress to the affected area for 15-20 minutes every 2-3 hours. This helps reduce inflammation and numb the pain. Remember not to apply ice directly to your skin; use a thin towel as a barrier. You can learn more about how to properly use ice for injuries from Cleveland Clinic.
- Compression: Gently wrap the calf with a compression bandage or wear a compression sleeve. This helps reduce swelling and provides support. Be careful not to wrap it too tightly, which could cut off circulation.
- Elevation: Whenever possible, lift your leg above heart level, especially when resting. This helps reduce swelling by promoting fluid drainage.

For mild pain, over-the-counter pain relievers, such as NSAIDs (non-steroidal anti-inflammatory drugs), can help manage discomfort and inflammation. Always use these as advised by your healthcare provider.
Advanced Relief and Supportive Therapies
Beyond initial home care, a comprehensive approach often includes targeted therapies.
- Gentle Stretching and Strengthening Exercises: Once the initial acute pain subsides, gentle stretching can help restore flexibility, and strengthening exercises can rebuild muscle resilience. A physical therapist can guide you through appropriate exercises to target the muscles on the side of your calf and surrounding areas, ensuring you don't exacerbate the injury.
- Supportive Care for Nerve and Muscle Pain: For ongoing discomfort, especially if there's a nerve component, supportive care is crucial. This can include managing underlying conditions, using ergonomic support, and ensuring proper posture.
- Topical Pain Relief Creams such as Neuropasil: For targeted, soothing relief from muscular aches and nerve discomfort, we often recommend a topical solution like Neuropasil. Our unique formula, powered by natural ingredients like Aloe, Urea, and Menthol, is designed to penetrate deeply and provide fast-acting relief for various types of pain, including the pain on side of calf from strains, muscle cramps, and nerve irritation. Many of our loyal customers testify to using Neuropasil for neuropathy, sciatica, fibromyalgia, plantar fasciitis, strains, sprains, aches and pains, joint discomfort, back and neck pain, cramps and aching feet. Athletes use Neuropasil to treat and recover from sore muscles. You can explore our best pain relief creams for muscle and nerve pain to find out more.
- Consult your healthcare provider for medical interventions for serious causes: If your pain on side of calf is due to a more serious condition like DVT, PAD, or a severe fracture, your doctor will recommend specific medical interventions. This could include medications (like blood thinners), physical therapy, or in some cases, surgical procedures.
Preventing Future Pain and When to See a Doctor
Taking proactive steps can significantly reduce your risk of developing pain on side of calf. Understanding your risk factors and knowing when to seek professional medical attention are key to maintaining your lower leg health.
Are You at Risk? Key Risk Factors for Developing Pain on the Side of the Calf
Certain factors can increase your susceptibility to pain on side of calf:
- Athletes/Runners: Repetitive stress, sudden increases in training intensity, inadequate warm-up, and improper biomechanics can lead to strains, tendonitis, or stress fractures.
- Age: As we age, muscles can lose elasticity, and bone density can decrease, increasing the risk of injuries like strains and stress fractures. Vascular conditions like PAD also become more common with age.
- Smoking: Smoking significantly impairs circulation, increasing the risk of peripheral artery disease (PAD) and hindering healing.
- Dehydration: Insufficient fluid intake can lead to electrolyte imbalances, a common cause of muscle cramps.
- Improper Footwear: Shoes that don't provide adequate support, are worn out, or don't fit properly can alter your gait and place undue stress on your calf muscles and tendons.
- Underlying Conditions (Diabetes, PAD): Conditions like diabetes can lead to nerve damage (neuropathy), while PAD directly affects blood flow to the legs, both contributing to calf pain.
How to Prevent Pain on the Side of the Calf
Prevention is always better than cure, especially when it comes to keeping your legs moving freely.
- Proper Warm-up/Cool-down: Before any physical activity, dedicate 5-10 minutes to light cardio and dynamic stretches. Afterward, cool down with static stretches to improve flexibility and reduce muscle soreness.
- Gradual Exercise Progression: Avoid sudden increases in the intensity, duration, or frequency of your workouts. Gradually build up your activity level to allow your muscles and tendons to adapt.
- Staying Hydrated: Drink plenty of water throughout the day, especially before, during, and after exercise. Consider electrolyte-rich beverages if you're sweating heavily during prolonged activity.
- Wearing Supportive Shoes: Invest in high-quality footwear that provides proper support and cushioning for your activity. Replace athletic shoes regularly as they wear out.
-
Essential Stretches for the Outer Calf and Peroneal Muscles: Incorporate these into your routine:
- Peroneal Stretch (Cross-Legged): Sit on the floor with your legs extended. Cross your affected leg over the other, placing your ankle on the opposite thigh. Gently pull your foot towards your body, feeling the stretch along the outer calf and ankle. Hold for 20-30 seconds.
- Standing Calf Stretch with External Rotation: Stand facing a wall, placing your hands on it. Step one foot back, keeping your heel on the ground. Turn your back foot slightly outward (external rotation). Lean forward, bending the front knee, until you feel a stretch along the outer calf of the back leg. Hold for 20-30 seconds.
- Ankle Eversion with Resistance Band: Sit with your legs extended. Loop a resistance band around the ball of your foot and anchor the other end. Slowly turn your foot outwards against the band's resistance. Perform 10-15 repetitions.
Red Flags: When to Call a Doctor Immediately
While many instances of pain on side of calf can be managed at home, certain symptoms warrant immediate medical attention. We encourage you to be vigilant and not hesitate to seek professional help if you experience any of the following:
- Signs of DVT: Sudden, unexplained swelling, redness, warmth, or tenderness in one calf. This could indicate a blood clot and is a medical emergency.
- Inability to Bear Weight: If you cannot put any weight on your leg after an injury.
- Severe, Sudden Pain: Especially if it occurred without a clear cause or is excruciating.
- Leg Feels Cool or Looks Pale: This can be a sign of a severe circulatory problem requiring urgent care.
- Numbness or Weakness: If you experience sudden or progressive numbness, tingling, or weakness in your leg or foot, it could indicate nerve damage.
- Pain at Rest: Pain that persists even when you are resting, especially if it's severe or accompanied by other concerning symptoms, should be evaluated. This can be a sign of PAD, DVT, or other serious issues. For more information on when to see a doctor for leg pain, consult myDr.com.au.
Frequently Asked Questions about Side Calf Pain
Can sciatica cause pain on the side of the calf?
Yes, absolutely! The sciatic nerve is a large nerve that runs from your lower back down through your buttocks and legs. While often associated with pain down the back of the leg, branches of the sciatic nerve can certainly refer pain, tingling, or numbness to the lateral (side) aspect of the calf. This happens when the nerve is compressed or irritated, often due to issues in the lower spine like a herniated disc or spinal stenosis.
How long does a side calf strain take to heal?
The healing time for a side calf strain largely depends on its severity, which is typically graded from 1 to 3:
- Mild (Grade 1): A minor pull with minimal pain and no loss of strength. Recovery usually takes 2 to 3 weeks.
- Moderate (Grade 2): A partial tear with noticeable pain, swelling, and some loss of strength. This typically requires 4 to 6 weeks for recovery.
- Severe (Grade 3): A complete rupture of the muscle, resulting in severe pain, significant swelling, and inability to use the muscle. This can take 3 months or more to heal and may require surgical intervention.
Is it OK to walk with side calf pain?
It really depends on the cause and severity of your pain on side of calf.
- If the pain is mild and due to muscle stiffness or minor soreness, gentle walking might actually help to improve blood flow and reduce stiffness. However, if the pain increases, stop immediately.
- For acute injuries like a muscle strain or if you suspect a more serious condition like DVT or a stress fracture, walking can worsen the problem and delay healing. In these cases, we advise you to avoid walking and seek medical advice. Never try to "push through" significant pain.
Conclusion
Understanding pain on side of calf is the first step toward finding relief and preventing future discomfort. As we've explored, the causes are incredibly diverse, ranging from common muscular strains and cramps to more serious conditions involving nerves, bones, or blood vessels. Recognizing the specific symptoms and knowing when to seek professional medical help versus applying self-care strategies is paramount for your health and well-being.
Whether your pain is a result of an intense workout, a sudden movement, or an underlying condition, our goal at Neuropasil is to empower you with knowledge and effective solutions. For targeted, soothing relief from muscular aches and nerve discomfort, consider a topical solution like Neuropasil. Our unique blend of natural ingredients, including Aloe, Urea, and Menthol, is designed to provide fast-acting comfort, helping you get back to your active life. Learn more about our natural ingredients and how they can support your journey to pain relief.
References
- Sports Medicine Australia. (n.d.). Gastrocnemius (Calf) Strain. Retrieved from https://sma.org.au/resources/injury-fact-sheets/gastrocnemius-calf-strain/
- Diabetes Australia. (2020). Peripheral Neuropathy. Retrieved from https://www.diabetesaustralia.com.au/blog/peripheral-neuropathy-2/
- painHEALTH. (n.d.). Örebro Musculoskeletal Pain Screening Questionnaire. Retrieved from https://painhealth.csse.uwa.edu.au/pain-self-checks/orebro-musculoskeletal-pain-screening-questionnaire/
- Cleveland Clinic. (2021). How Long You Should Ice an Injury. Retrieved from https://health.clevelandclinic.org/how-long-to-ice-an-injury
- myDr. (2021). Leg ache - causes and symptoms. Retrieved from https://mydr.com.au/skin-hair/leg-ache/
- Zemaitis, M. R., et al. (2023). Peripheral Arterial Disease. In StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK430745/
- Mount Sinai. (n.d.). Common peroneal nerve dysfunction. Retrieved from https://www.mountsinai.org/health-library/diseases-conditions/common-peroneal-nerve-dysfunction
- Monderer, R. S., et al. (2017). A randomized, double-blind, placebo-controlled, single-center study of the safety and efficacy of the orally administered TRPA1/V1 agonist, ALGRX-4975, for the treatment of muscle cramps in adult patients. PLoS One. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5435142/













