Why Understanding What Helps Rheumatoid Arthritis Is Your First Step to Relief
What helps rheumatoid arthritis? If you're facing the daily challenges of joint pain, stiffness, and fatigue, this question is likely on your mind. The good news is that modern medicine offers multiple proven approaches to manage this autoimmune condition effectively.
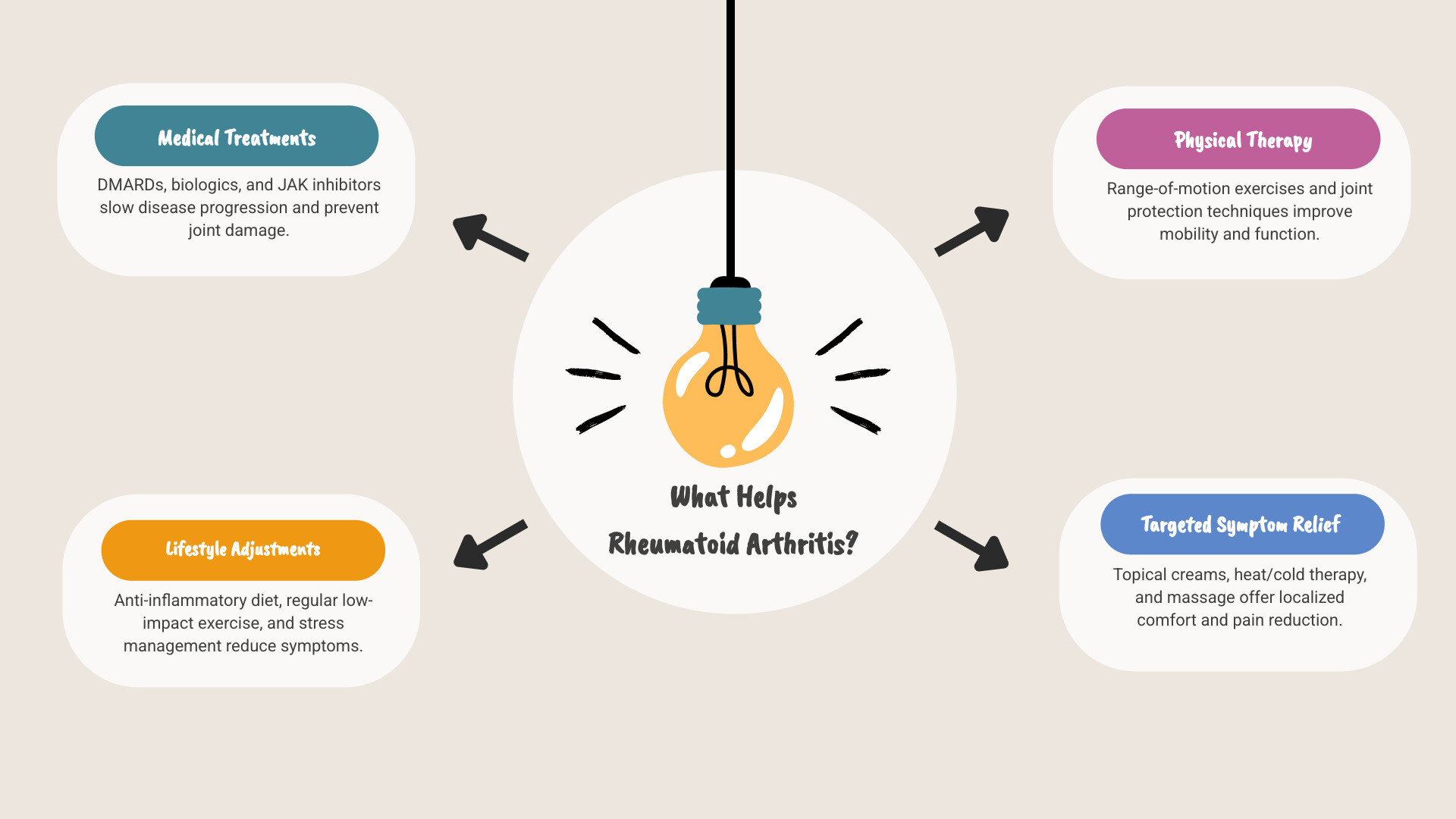
Quick Answer: What Helps Rheumatoid Arthritis
- Medications: DMARDs (like methotrexate), biologics, and JAK inhibitors to slow disease progression
- Lifestyle Changes: Anti-inflammatory diet, regular low-impact exercise, stress management
- Physical Therapy: Range-of-motion exercises and joint protection techniques
- Topical Relief: Pain-relieving creams and gels for targeted comfort
- Medical Procedures: Joint injections and surgery for severe cases
- Supportive Care: Heat/cold therapy, massage, and mind-body practices
My experience in developing pain relief solutions has shown that combining medical treatments with targeted topical relief often provides the most comprehensive approach to RA management. This guide will walk you through evidence-based strategies that can help you reclaim your mobility and quality of life.
Explore more about What helps rheumatoid arthritis?:
Understanding Rheumatoid Arthritis: More Than Just Joint Pain
To know what helps rheumatoid arthritis, we must first understand the condition. RA is not simple joint wear-and-tear; it's a complex autoimmune disease where the body's immune system mistakenly attacks its own tissues.
What is RA and What Are the Symptoms?
In rheumatoid arthritis (RA), the immune system attacks the synovium, the lining of the joints. This is different from osteoarthritis, which results from mechanical wear. The attack causes chronic inflammation that can lead to serious damage if untreated.
A key sign of RA is its symmetrical pattern—if one wrist hurts, the other likely will too. It often starts in smaller joints like the fingers and hands. Common symptoms include:
- Joint pain and swelling
- Morning stiffness that can last for hours
- Profound fatigue
- Low-grade fevers and loss of appetite
- Rheumatoid nodules (firm bumps under the skin)
The CDC provides comprehensive information on RA and its impact on daily life.
Causes, Risk Factors, and Potential Complications
The exact cause of RA is unknown, but it involves a combination of genetics, environment, and immune system issues. Certain genes (like HLA variations) increase susceptibility. Smoking is a major environmental risk factor that can also make the disease more severe. Other factors include:
- Sex: Women are about three times more likely to develop RA than men.
- Age: It most commonly appears between ages 30 and 60.
If left untreated, the chronic inflammation can cause irreversible joint damage, including cartilage and bone erosion leading to deformity. Complications can extend beyond the joints, affecting the eyes, lungs, and heart. The Mayo Clinic explains how RA can affect lung function, and it also increases the risk of cardiovascular disease. Early, effective treatment is crucial to prevent these serious issues.
How Doctors Diagnose Rheumatoid Arthritis
There is no single test for RA. Diagnosis involves piecing together evidence from several sources:
- Medical History and Physical Exam: Your doctor will ask about your symptoms, their pattern, and family history. They will check joints for swelling, tenderness, and warmth.
- Blood Tests: These look for inflammatory markers (ESR, CRP) and specific antibodies like rheumatoid factor (RF) and anti-CCP antibodies. The anti-CCP test is highly specific for RA, making it a key indicator in diagnosis.
- Imaging Tests: X-rays can track joint damage over time, while MRI and ultrasound can detect early inflammation.
A primary care doctor will likely refer you to a rheumatologist, a specialist in autoimmune diseases, for a definitive diagnosis and treatment plan. Early diagnosis and prompt treatment are the keys to preventing long-term damage.
Medical Treatments for RA: A Modern Approach to Remission
The goal of modern RA treatment has shifted from just managing pain to achieving remission or the lowest possible level of disease activity. This approach aims to minimize joint damage and dramatically improve function and quality of life.

Medications That Help Rheumatoid Arthritis
Medications are the foundation of most RA treatment plans, working to calm the overactive immune system.
Disease-Modifying Anti-Rheumatic Drugs (DMARDs): These are the cornerstone of treatment, as they slow disease progression and prevent joint damage. Methotrexate is the most common first-line DMARD. Other conventional DMARDs include leflunomide, hydroxychloroquine, and sulfasalazine. The National Rheumatoid Arthritis Society provides detailed information on DMARDs.
Biologics: These targeted drugs are used when conventional DMARDs aren't effective enough. Biologics target specific parts of the immune system, such as TNF inhibitors. Because they suppress the immune system, they can increase the risk of infections.
JAK inhibitors: These are newer oral medications that block immune signaling pathways. JAK inhibitors are typically used when other treatments have failed.
Corticosteroids: Drugs like prednisone offer rapid relief from pain and swelling during flare-ups but are generally used for short periods due to potential side effects.
NSAIDs: Over-the-counter options like ibuprofen can help with pain and inflammation but do not slow the disease's progression.
Early and aggressive treatment is crucial for improving long-term outcomes and achieving remission.
Other Medical Procedures: Injections and Surgery
When medications aren't enough, other procedures can provide relief.
Corticosteroid injections: A steroid injected directly into a painful joint can provide powerful, localized relief from inflammation. The American College of Rheumatology offers details on joint injections and aspirations.
-
Surgery: This is an option for advanced RA with significant joint damage. Surgical procedures include:
- Synovectomy: Removal of the inflamed joint lining (synovium).
- Tendon repair: To fix tendons damaged by inflammation.
- Joint fusion: Stabilizes a severely damaged joint to relieve pain, though it eliminates movement.
- Total joint replacement (arthroplasty): Damaged joints (like hips or knees) are replaced with artificial ones to restore function and reduce pain.
What Helps Rheumatoid Arthritis? Lifestyle and Home Management Strategies
Beyond medical treatments, what helps rheumatoid arthritis often involves daily lifestyle choices. These strategies give you more control over how RA affects your life.
The Role of Diet and Nutrition in Managing RA
An anti-inflammatory diet can be a powerful tool for managing RA. The focus is on eating foods that naturally fight inflammation.

The Mediterranean diet is often recommended. It emphasizes fish, colorful vegetables, nuts, beans, and olive oil. Key anti-inflammatory components include:
- Omega-3 fatty acids: Found in fatty fish like salmon, as well as walnuts and flaxseeds.
- Antioxidants: Abundant in brightly colored fruits and vegetables like berries and spinach.
- Fiber: Found in whole grains, legumes, and nuts, it can help lower inflammatory markers.
- Extra-virgin olive oil: Contains oleocanthal, a compound with anti-inflammatory properties.
It's also wise to limit processed foods, sugar, and saturated fats, which can promote inflammation. For guidance, see these tips for an anti-inflammatory diet from the Cleveland Clinic.
Exercise and Physical Therapy: Staying Active with RA
While it may seem counterintuitive, the right kind of movement can reduce pain and improve strength and flexibility.
Focus on gentle, consistent activities:
- Water exercise: The buoyancy of water supports your body and reduces impact on joints.
- Low-impact activities: Walking, cycling, and using an elliptical machine are great for cardiovascular health.
- Range-of-motion exercises: Help maintain joint flexibility and reduce stiffness.
- Strengthening exercises: Stronger muscles support and protect your joints.
- Tai Chi: This gentle practice improves strength, balance, and flexibility while reducing stress.
A physical therapist can design a personalized exercise program, while an occupational therapist can teach you joint-protection techniques for daily tasks. It's crucial to balance rest and activity. The CDC provides guidance on physical activity and arthritis.
Mind-Body Practices and Stress Reduction
Stress can trigger or worsen RA flares, so mind-body practices can help break this cycle.
- Mindfulness and meditation: These practices teach you to observe pain and stress without being overwhelmed by them.
- Deep breathing exercises: Can quickly calm your body's stress response.
- Pacing activities: Break tasks into smaller, manageable chunks with rest breaks to conserve energy.
- Quality sleep: Essential for managing pain and fatigue. Establish a consistent sleep routine.
- Heat and cold therapy: Use cold packs to reduce swelling during flares and heat (like warm baths or heating pads) to soothe stiff, aching joints.
Exploring Supportive and Topical Therapies for RA Relief
Beyond conventional medicine, many people find relief through supportive approaches. This section explores topical treatments and other therapies that can support your RA management plan.
Topical Relief and Supportive Therapies for Rheumatoid Arthritis
When you need relief right where it hurts, topical treatments can be a great addition to your plan. They deliver active ingredients directly to the affected area with fewer systemic side effects.

- Menthol-based products create a cooling sensation that can distract from pain.
- Aloe vera formulations are gentle and offer soothing properties for irritated skin around joints.
- Capsaicin creams work by depleting a chemical messenger that transmits pain signals.
- Topical NSAIDs contain active ingredients like diclofenac sodium, which penetrates the skin to target pain and inflammation at the source.
What helps rheumatoid arthritis? In our experience, Neuropasil nerve pain relief cream provides fast-acting, targeted comfort. Powered by natural ingredients like aloe, urea, and menthol, many customers find it valuable for managing the aches and pains of RA. Explore Neuropasil for targeted, soothing relief from joint discomfort.
Other supportive therapies include:
- Massage therapy: Can relax muscles and improve circulation. Find a therapist experienced with RA.
- Acupuncture: May help lower inflammation-linked chemicals and alleviate chronic pain.
- TENS units: These devices use a gentle electrical current to block pain signals.
Always consult your doctor before starting new therapies.
Supplements and Herbal Approaches: What Does the Science Say?
While some supplements show promise, it's crucial to approach them with caution and discuss them with your doctor. The National Center for Complementary and Integrative Health provides an in-depth look at complementary health approaches for RA.
- Fish oil supplements: Rich in omega-3s, they have strong scientific backing for reducing pain and stiffness in RA patients.
- Turmeric (Curcumin): A scientific review of curcumin for RA found that it significantly reduced disease activity, pain, and inflammatory markers.
- Probiotics and Ginger: These are also being studied for their potential anti-inflammatory benefits.
Natural doesn't mean risk-free. Your healthcare provider can help you avoid harmful interactions with your prescribed medications.
Living with RA: Outlook, Support, and Your Healthcare Team
Managing RA is a long-term journey, but the outlook today is brighter than ever. With modern advancements, many people with RA live full, active lives.
The Long-Term Outlook for People with RA
While there is no cure for rheumatoid arthritis, the condition can be managed effectively. The modern treatment goal is remission (little to no disease activity), which is a realistic possibility for many. Early diagnosis and aggressive treatment are critical to:
- Control symptoms like pain and stiffness.
- Prevent or slow permanent joint damage.
- Maintain mobility and function.
- Improve overall quality of life.
Living with RA means learning to manage occasional flares (periods of worsening symptoms). Regular communication with your doctor is essential to adjust treatments and manage the condition effectively over the long term.
Building Your Support System
Navigating RA is a marathon, not a sprint, and you don't have to do it alone. A strong support system is a key investment in your health.
Your Healthcare Team: This is your core support. It's led by your rheumatologist and includes your primary care doctor, physical therapist, and occupational therapist. Depending on your needs, it may also include other specialists.
Family and Friends: Open communication helps loved ones understand your challenges and provide practical and emotional support.
Support Groups: Connecting with others who have RA provides validation and practical insights from people who truly understand what you're going through.
Mental Health Support: Living with a chronic illness can be emotionally taxing. A therapist can provide valuable coping strategies for stress, anxiety, or depression.
Asking for help is a sign of strength. Building a team to support you is one of the smartest things you can do for your well-being.
Conclusion: Taking Control of Your Rheumatoid Arthritis Journey
Your journey with rheumatoid arthritis doesn't have to be one of constant struggle. The question "What helps rheumatoid arthritis?" has many answers, and the key is finding the right combination that works for you.
We've explored how modern medical treatments can slow the disease, how diet and exercise can reduce inflammation and pain, and how mind-body practices can help manage the emotional side of living with a chronic illness. The most encouraging truth is that remission is a realistic goal.
Working closely with your healthcare team and building a strong support system are crucial. You are not walking this path alone. For those moments when you need targeted relief right where it hurts, topical treatments like our Neuropasil cream can provide an extra layer of comfort, helping you keep moving forward.
What helps rheumatoid arthritis? The answer is individual, but hope and effective treatment options are very real. Take it one day at a time, celebrate small victories, and never underestimate your ability to adapt and thrive.
Explore Neuropasil for targeted, soothing relief from joint discomfort
References
- Rheumatoid Arthritis (RA), Centers for Disease Control and Prevention (CDC): https://www.cdc.gov/arthritis/rheumatoid-arthritis/
- Rheumatoid arthritis: Can it affect the lungs?, Mayo Clinic: https://www.mayoclinic.org/diseases-conditions/rheumatoid-arthritis/expert-answers/rheumatoid-arthritis/FAQ-20058245?p=1
- Rheumatoid Arthritis (RA) Diagnosis, Johns Hopkins Arthritis Center: https://www.hopkinsarthritis.org/arthritis-info/rheumatoid-arthritis/ra-diagnosis/
- DMARDs, National Rheumatoid Arthritis Society (NRAS): https://nras.org.uk/resource/dmards/
- Biologic Treatments for RA, National Rheumatoid Arthritis Society (NRAS): https://nras.org.uk/resource/biologics/
- JAK Inhibitors, National Rheumatoid Arthritis Society (NRAS): https://nras.org.uk/resource/jak-inhibitors/
- Joint Injections (Joint Aspirations), American College of Rheumatology: https://rheumatology.org/patients/joint-injections-joint-aspirations
- Surgery for rheumatoid arthritis, Versus Arthritis: https://www.versusarthritis.org/about-arthritis/conditions/rheumatoid-arthritis/treatments/surgery/
- An Anti-Inflammatory Diet for Rheumatoid Arthritis, Cleveland Clinic: https://health.clevelandclinic.org/rheumatoid-arthritis-diet-tips
- Physical Activity for Arthritis, Centers for Disease Control and Prevention (CDC): https://www.cdc.gov/arthritis/prevention/
- How Stress Impacts RA, Arthritis Foundation: https://www.arthritis.org/health-wellness/healthy-living/emotional-well-being/stress-management/how-stress-impacts-ra
- Heat and Cold Therapy for Arthritis Pain, Arthritis Foundation: https://www.arthritis.org/health-wellness/healthy-living/managing-pain/pain-relief-solutions/heat-and-cold-therapy-for-arthritis-pain
- Topical Pain Relief: What’s the Best for You?, Cleveland Clinic: https://health.clevelandclinic.org/topical-pain-relief
- Rheumatoid Arthritis: In Depth, National Center for Complementary and Integrative Health (NCCIH): https://www.nccih.nih.gov/health/rheumatoid-arthritis-in-depth
- Efficacy and safety of Curcumin/Curcuma longa extract for the treatment of rheumatoid arthritis, PubMed Central: https://pubmed.ncbi.nlm.nih.gov/34331695/















