Your Guide to Understanding and Relieving Lower Back Pain
If you're looking for relief from pain lower back, you're not alone. This common ailment is a leading cause of disability worldwide and a top reason for missed work and doctor visits in the U.S.
Here's a quick look at the impact of lower back pain:
- Extremely Common: Affects nearly everyone at some point.
- Global Impact: The leading cause of disability worldwide.
- Work-Related: A top reason for missing work.
- Frequent Doctor Visits: Second most common reason for doctor visits in the U.S.
This guide will help you understand the types of lower back pain, its causes, and how to find relief. You'll also learn how to prevent future issues and when to seek medical help.
I'm Tony Enrico, a pain management expert dedicated to helping people find relief from conditions like pain lower back. My goal is to provide solutions for fast, long-lasting comfort.
Pain lower back terms made easy:
- Muscle soreness
- back muscles strain
- muscle spasm relief
Understanding Your Lower Back Pain: Symptoms and Types
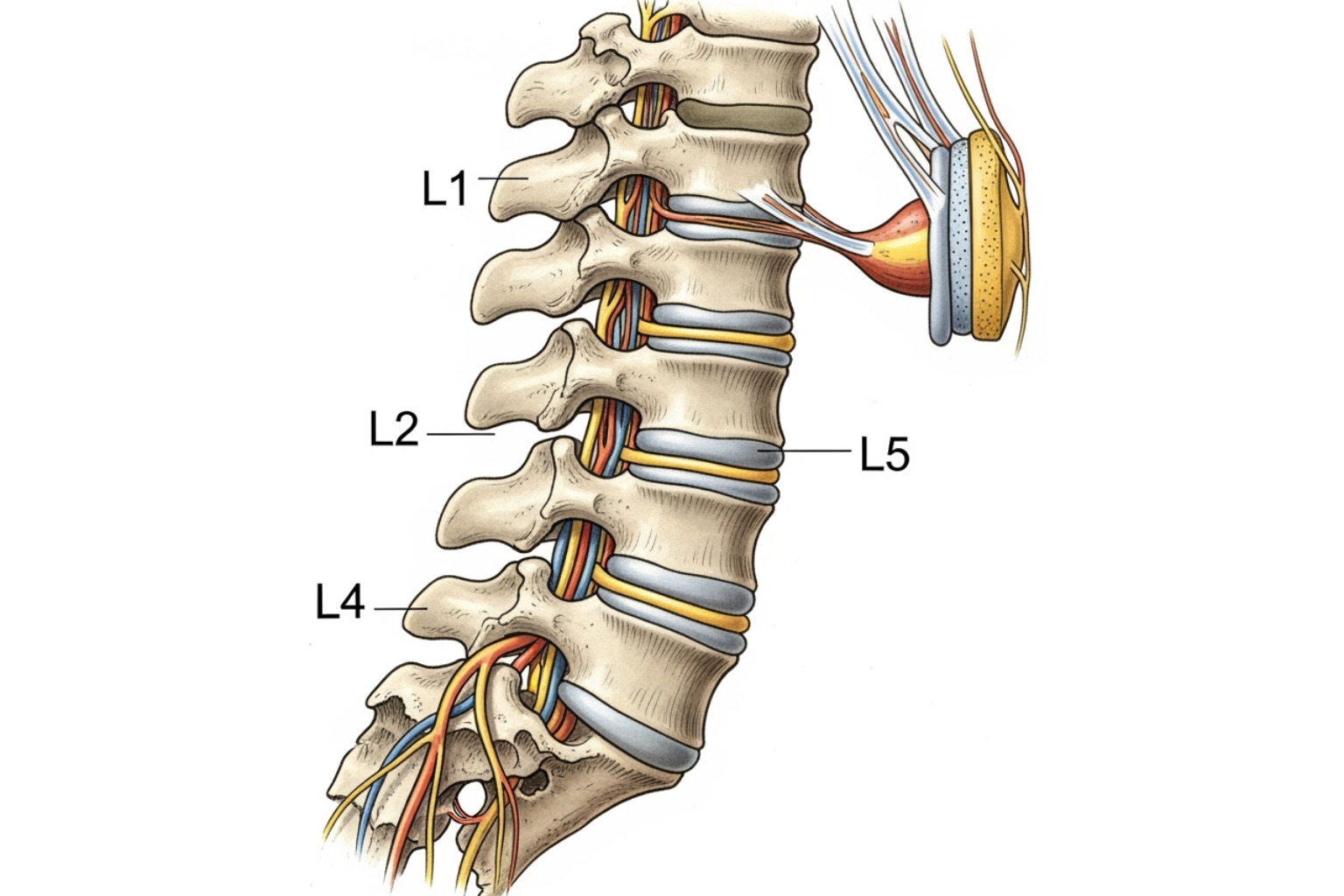
Your lower back, or lumbar region, supports your upper body and allows for movement, but this makes it vulnerable to pain lower back. The pain can range from a dull, constant ache to a sharp, sudden sensation. Understanding your symptoms is the first step toward finding the right path to recovery.
Typical Symptoms of Pain Lower Back
Lower back pain symptoms vary, but some common patterns can help you identify the issue.
- Dull, Aching Pain: A persistent, throbbing pain that often worsens after prolonged standing or sitting.
- Sharp, Stabbing Sensations: Often signals an acute injury or irritated nerve, triggered by movements like bending, twisting, or lifting.
- Pain Worsens with Movement: Walking or bending can stress the back, while reclining often provides relief by taking pressure off the spine.
- Radiating Pain Down the Leg: Pain that shoots into your buttock, thigh, or foot is a hallmark of sciatica, caused by irritation of the sciatic nerve. For more details, see our guide on Sciatica Symptoms.
- Numbness or Tingling: A "pins-and-needles" feeling in the leg or foot often indicates nerve compression.
- Stiffness and Decreased Movement: Difficulty bending or twisting, often due to muscles tightening to protect an injured area.
- Muscle Spasms: Sudden, painful muscle contractions that can severely limit movement. For more on muscle-related issues, read our article on Muscle Pain.
Acute vs. Chronic Lower Back Pain
Understanding whether your pain lower back is acute or chronic is key to managing it effectively.
Acute lower back pain comes on suddenly, often after an injury or lifting something improperly. It typically resolves within a few days to a few weeks (less than 12 weeks) with conservative care.
Chronic lower back pain persists for 12 weeks or longer. It may develop gradually and is often caused by more complex issues like arthritis, degenerative disc disease, or spinal stenosis. Managing chronic pain requires a long-term approach combining treatments and lifestyle adjustments.
| Feature | Acute Lower Back Pain | Chronic Lower Back Pain |
|---|---|---|
| Duration | Lasts a few days to a few weeks (less than 12 weeks) | Persists for 12 weeks or longer |
| Onset | Often sudden, typically linked to a specific event | Develops more slowly, can be gradual and insidious |
| Typical Causes | Muscle strains, ligament sprains, minor injuries from overuse or improper lifting | Degenerative disc disease, arthritis, spinal stenosis, nerve compression, prolonged poor posture, underlying medical conditions |
| Prognosis | Most cases resolve on their own with conservative care | Requires ongoing management, diagnosis can be complex, may involve multidisciplinary approach |
When to See a Doctor: Red Flag Symptoms
While most pain lower back can be managed at home, certain "red flag" symptoms require immediate medical attention.
- Pain After an Injury or Fall: Get checked for a fracture or other serious injury, especially if you're over 50.
- Bowel or Bladder Control Issues: This is a medical emergency that could indicate cauda equina syndrome, a serious condition requiring urgent intervention.
- Severe or Progressive Leg Weakness or Numbness: Suggests significant nerve compression that needs prompt evaluation.
- Fever with Back Pain: Could point to a spinal infection.
- Unexplained Weight Loss: May signal an underlying systemic condition.
- Pain is Worse at Night or During Rest: Pain that wakes you from sleep is unusual and should be investigated.
- Pain Doesn't Improve After a Week: If self-care isn't working or the pain is worsening, consult a doctor.
- History of Certain Conditions: If you have a history of cancer, osteoporosis, or IV drug use, or are over 50 with new back pain, see a doctor.
Uncovering the Common Causes of Your Pain Lower Back
Understanding why you have pain lower back is a key step toward relief. The lower back is a complex structure of vertebrae, discs, nerves, muscles, and ligaments. When any of these parts are compromised, pain can result.
Mechanical and Acute Injuries
Sudden pain lower back is often due to mechanical issues or acute injuries related to daily activities.
- Muscle Strains and Ligament Sprains: These occur when muscle fibers or ligaments are overstretched or torn, often from an awkward movement, heavy lifting, or overexertion. For more details, explore our insights on Muscle Pain.
- Improper Lifting Techniques: Lifting with your back instead of your legs, or twisting while lifting, puts immense stress on your spine.
- Overuse from Sports or Work: Repetitive motions or prolonged postures can lead to nagging overuse injuries.
Structural Spine Issues
Sometimes, pain lower back stems from persistent structural problems within the spine.
- Herniated or Bulging Discs: The soft inner part of a spinal disc pushes out, potentially compressing nearby nerves and causing pain, numbness, or sciatica. For authoritative information, see this guide on Herniated Discs from Johns Hopkins Medicine.
- Sciatica: This is pain that radiates along the path of the sciatic nerve, from the lower back down the leg.
- Spinal Stenosis: A narrowing of the spinal canal that can squeeze nerves, causing pain or weakness in the legs, especially when standing or walking.
- Scoliosis: An abnormal sideways curve of the spine that can cause uneven stress and pain over time.
- Degenerative Disc Disease: Age-related wear and tear on spinal discs, making them thinner and less effective as shock absorbers.
- Spondylolisthesis: A condition where one vertebra slips forward over the one below it, causing instability and potential nerve compression.
Underlying Conditions and Lifestyle Factors
Various medical conditions and lifestyle choices can contribute to pain lower back.
- Inflammatory Conditions: Arthritis, such as osteoarthritis or ankylosing spondylitis, can cause inflammation and pain in the back's joints. Learn more about Managing Arthritis Pain.
- Osteoporosis: This condition weakens bones, making them susceptible to painful vertebral compression fractures.
- Fibromyalgia: A chronic condition known for widespread pain that can include the lower back.
- Poor Posture: Slouching or hunching puts continuous strain on the lumbar spine.
- Obesity: Excess weight, especially around the abdomen, increases the load on your lower back.
- Sedentary Lifestyle: Weak core muscles from inactivity fail to properly support the spine, increasing injury risk.
- Smoking: Nicotine restricts blood flow to spinal discs, impairing their ability to heal and increasing inflammation.
- Other Conditions: Issues like kidney stones, infections, pregnancy, and menstrual cramps can cause referred pain that feels like back pain.
Effective Relief and Treatment Options
Finding the right relief for pain lower back often requires a personalized approach. A proper diagnosis is the crucial first step before starting any treatment.
At-Home Care and Remedies
For most acute pain lower back, simple self-care strategies can be highly effective.
- Limited Rest: Avoid prolonged bed rest. More than a day or two can slow recovery. Gentle movement is better for healing.
- Ice and Heat Therapy: Use ice for the first 48-72 hours to reduce inflammation. After that, switch to heat to relax tight muscles and improve blood flow.
- Over-the-Counter (OTC) Pain Relievers: Medications like ibuprofen (Advil), naproxen (Aleve), or acetaminophen (Tylenol) can manage mild to moderate pain. Always follow package directions.
- Topical Creams and Gels: Products with ingredients like menthol provide targeted relief. Our Neuropasil cream is formulated to deliver fast-acting, soothing comfort for muscle and nerve-related back pain.
- Gentle Movement and Stretching: Light walking and simple stretches, such as knee-to-chest tilts, can reduce stiffness. Stop if any movement sharpens your pain. Find more tips in our guide on What Helps Sore Muscles.
Medical and Professional Treatments
If home care isn't enough, professional help is a smart next step for persistent pain lower back.
- Physical Therapy: A physical therapist can design a custom program to strengthen your core, improve flexibility, and teach you proper body mechanics.
- Prescription Medications: For more severe pain, doctors may prescribe stronger NSAIDs, muscle relaxants, or specific nerve pain medications.
- Epidural Steroid Injections: For persistent nerve-related pain, corticosteroids injected near the spinal nerves can reduce inflammation and provide significant relief.
- Surgery: This is a last resort, considered only for severe conditions like herniated discs or spinal stenosis when conservative treatments have failed. For a full overview of options, see this Comprehensive overview from the NIH.
Complementary and Alternative Therapies
These therapies can work well alongside conventional treatments for pain lower back.
- Massage Therapy: Can release tight muscles, reduce pain signals, and improve circulation to injured tissues.
- Chiropractic Adjustments: Focus on spinal alignment to improve joint function and reduce pain, and is recognized as a complementary health approach for acute back pain.
- Acupuncture: This traditional practice may help release the body's natural pain-relieving chemicals and is a common complementary therapy for chronic back pain.
- Yoga and Tai Chi: These mind-body practices combine physical postures, breathing, and mindfulness to improve flexibility, strength, and stress management.
Prevention and Long-Term Management
While you can't always prevent pain lower back, you can significantly reduce your risk by building a more resilient spine through smart daily habits and targeted exercises.
Key Lifestyle Adjustments
Your daily habits have a major impact on your back health.
- Maintain a Healthy Weight: Reducing excess weight, especially around your midsection, lessens the strain on your spine.
- Quit Smoking: Quitting improves blood flow and nutrient delivery to your spinal discs, which aids healing and reduces inflammation.
- Manage Stress: Chronic stress leads to muscle tension. Practices like meditation, deep breathing, or yoga can reduce both physical tension and pain.
- Create an Ergonomic Workspace: Ensure your chair supports your lower back, your feet rest flat on the floor, and your computer screen is at eye level.
- Wear Supportive Footwear: Avoid high heels and unsupportive shoes. Choose footwear with good arch support and cushioning to maintain proper alignment.
Exercises for a Stronger Back
A strong core is your best defense against pain lower back. Your core includes the muscles in your abdomen, back, and glutes that stabilize your spine.
- Core Strengthening: Exercises like planks and the bird-dog are excellent for building a stable core.
- Flexibility and Stretching: Gentle stretches are crucial. The knee-to-chest stretch releases the lower back, the cat-cow stretch improves spinal mobility, and hamstring stretches prevent tightness that can pull on your pelvis.
- Low-Impact Aerobic Exercise: Activities like walking, swimming, or cycling improve circulation and reduce stiffness without jarring your spine. Aim for 30 minutes on most days. Proper management of After Workout Soreness is also key to staying consistent.
Preventative Measures for Pain Lower Back
Adopt these protective habits to reduce your risk of a back injury.
- Proper Lifting Technique: Always bend at your knees, not your waist. Keep the object close to your body, engage your core, and use your leg muscles to lift. Never twist while holding a heavy object.
- Maintain Good Posture: Stand and sit tall, with your shoulders back and core engaged, to minimize chronic strain on your spine.
- Take Frequent Breaks from Sitting: Stand up, stretch, and walk around every 30-60 minutes to relieve pressure on your spinal discs.
- Sleep in a Supportive Position: If you sleep on your side, place a pillow between your knees. If you sleep on your back, a pillow under your knees helps maintain proper spinal alignment.
Frequently Asked Questions about Lower Back Pain
It's natural to have questions about pain lower back. Here are clear, concise answers to some of the most common ones.
How long does acute lower back pain typically last?
Most acute pain lower back resolves within a few days to a few weeks, with many people feeling significantly better in under six weeks. As defined by medical guidelines, pain that lasts for more than 12 weeks is considered chronic and may require a more comprehensive, long-term management plan. Recovery time depends on the cause of the pain and your adherence to treatment.
Is walking good for lower back pain?
Yes, walking is generally an excellent low-impact exercise for pain lower back. It helps increase blood flow, reduce stiffness, and gently strengthen the muscles that support your spine. The key is to start with short, gentle walks on flat surfaces and gradually increase your distance as you feel better. Always listen to your body and ease up if the pain worsens.
Can stress and anxiety cause lower back pain?
Yes, there is a strong link between mental stress and pain lower back. When you're stressed or anxious, your body's natural response is to tense your muscles. Chronic tension in the back can lead directly to pain and stiffness. Furthermore, stress can amplify your brain's perception of pain. Learning to manage stress through relaxation techniques like meditation, deep breathing, or yoga can help alleviate both your anxiety and your back pain.
Conclusion: Taking Control of Your Back Health
We've explored the symptoms, causes, and a wide range of treatments for pain lower back. The most important takeaway is that while this pain is common and can feel debilitating, it is almost always manageable. Most cases improve significantly with conservative care at home or with professional guidance.
Prevention is your best tool for long-term back health. By making conscious lifestyle choices and knowing when to see a doctor for red flag symptoms, you can protect your spine. Always seek medical advice when you need it.
Embracing a spine-healthy lifestyle includes:
- Maintaining a healthy weight
- Staying active with core exercises and stretching
- Practicing good posture
- Using proper lifting techniques
For those moments when pain lower back flares up, our Neuropasil topical cream can be a valuable ally. It's designed to provide targeted, soothing relief for muscle and nerve-related discomfort, helping you get back to your life with less pain and more comfort.
Ready to experience that soothing relief for yourself?
Find fast-acting relief for your back pain.
References/Sources
This guide on pain lower back is based on research from trusted medical institutions and scientific studies. We believe in transparency and have listed our key sources below.
Major Medical Institutions and Research:
The National Institutes of Health (NIH) offers a comprehensive Low Back Pain Fact Sheet covering causes, treatments, and prevention from the National Institute of Neurological Disorders and Stroke.
Johns Hopkins Medicine provides a detailed guide on Lumbar Disc Disease (Herniated Disc), explaining its role in back pain.
The Cleveland Clinic offers patient-friendly information on Lower Back Pain, including symptoms, causes, and when to seek care.
Research on Treatment Approaches:
Studies from the National Center for Biotechnology Information (NCBI) library explore various aspects of back pain management:
- Research on massage therapy effectiveness for subacute low-back pain.
- Studies on the relationship between forward head posture and back pain.
- Investigation into pain, nicotine, and smoking.
- Research on cryotherapy effects for pain relief.
Complementary and Alternative Therapies:
The National Center for Complementary and Integrative Health offers evidence-based information on chiropractic care and other complementary health approaches.
Harvard Health Publishing provides accessible articles on the importance of stretching and the health benefits of tai chi.
Clinical Guidelines and Statistics:
The Centers for Disease Control and Prevention (CDC) tracks back pain prevalence among U.S. adults.
Clinical practice guidelines from the American College of Physicians on noninvasive treatments for low back pain inform current best practices.
We've also referenced information from the NIH Osteoporosis and Related Bone Diseases National Resource Center on smoking and bone health, and the National Institute of Arthritis and Musculoskeletal and Skin Diseases on general back pain topics.
Always consult with your healthcare provider for personalized medical advice.














