Understanding the Hidden Burden of Fibromyalgia
Fibromyalgia is a chronic condition affecting around 4 million people in the U.S., characterized by widespread pain, severe fatigue, and cognitive issues known as "fibro fog." It's a central nervous system disorder that amplifies pain signals, meaning your brain and spinal cord process pain differently, leading to heightened sensitivity throughout the body. The pain is real, not imaginary, stemming from altered neural pathways.
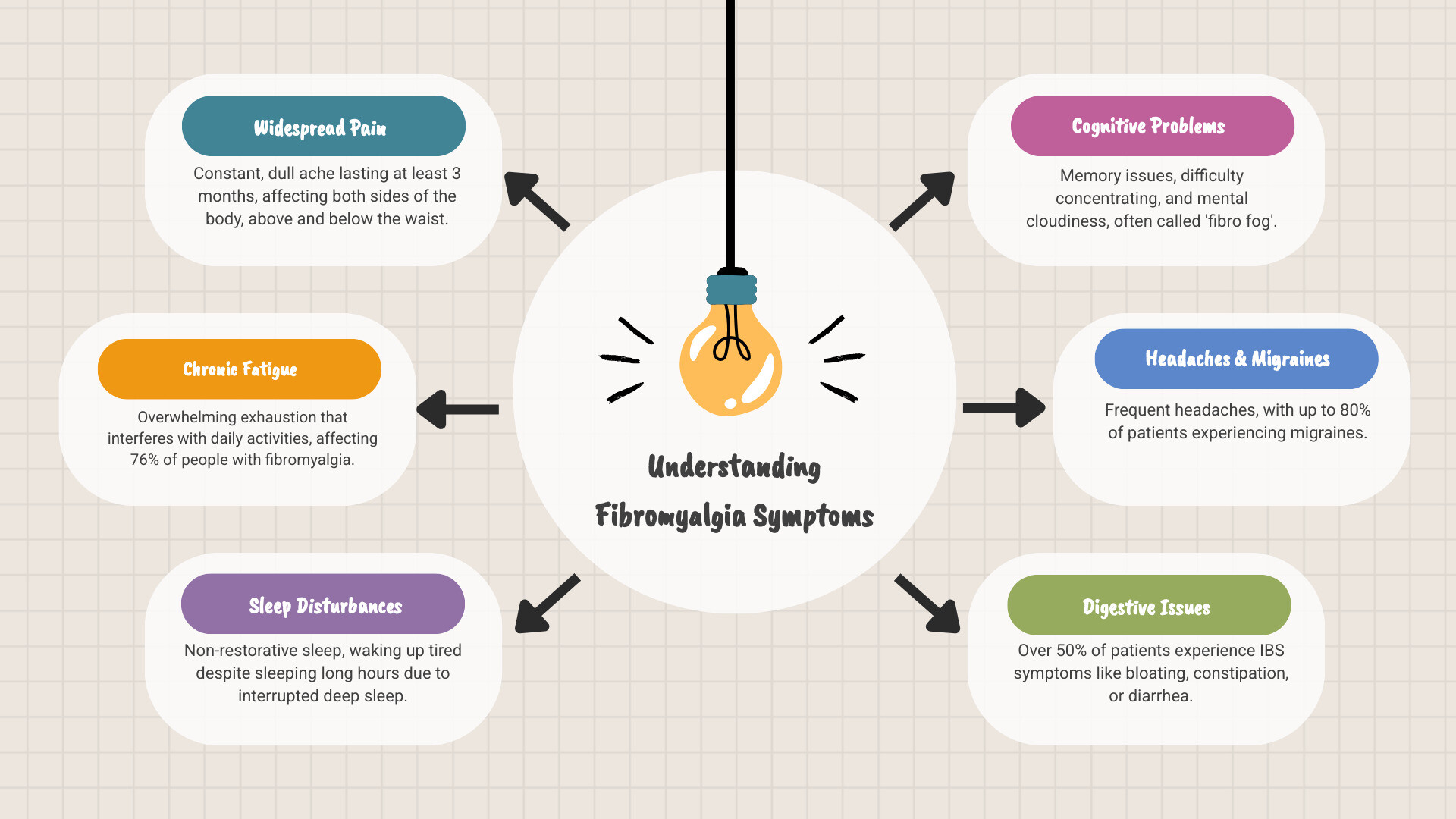
Key symptoms of fibromyalgia include:
- Widespread Pain: A constant dull ache on both sides of the body, lasting at least three months.
- Chronic Fatigue: Overwhelming exhaustion affecting daily life.
- Sleep Disturbances: Waking up tired despite long hours of sleep.
- Cognitive Problems ("Fibro Fog"): Issues with memory and concentration.
- Other Common Symptoms: Headaches, digestive issues like IBS, and sensory sensitivities to light, noise, and temperature.
What makes fibromyalgia challenging is its complexity and invisibility. It's diagnosed based on symptoms, not lab tests, and its intensity can fluctuate in periods called "flare-ups." I'm Tony Enrico, and at Neuropasil, we help people manage the overwhelming symptoms of fibromyalgia. Understanding them is the first step toward finding relief.
Understanding Fibromyalgia and Its Core Symptoms
If you're experiencing unexplained widespread pain and crushing fatigue, you may be dealing with fibromyalgia. This complex, chronic condition affects millions, and understanding it is the first step toward relief.
What is Fibromyalgia?
Fibromyalgia is a chronic disorder causing widespread musculoskeletal pain and tenderness. It is not an autoimmune or inflammatory disease like arthritis, so it doesn't damage joints or muscles. Instead, it involves central sensitization, where the brain and spinal cord become overly sensitive to pain signals. Think of it as the volume knob on your pain receptors being turned way up. This is a real, physical change in how your nervous system works, making normal sensations feel painful.
According to the CDC, this altered pain processing is what distinguishes fibromyalgia from other chronic pain conditions. It's far more than just "aching muscles."
The Primary Symptoms of Fibromyalgia: Pain, Fatigue, and Sleep Issues
The symptoms of fibromyalgia revolve around a challenging cycle of three main issues.
Widespread pain is the hallmark symptom. It's a constant dull ache lasting at least three months, occurring on both sides of the body and above and below the waist. The pain can feel deep, burning, or throbbing and often migrates. This heightened sensitivity can also cause hyperalgesia (where painful things hurt more) and allodynia (where non-painful stimuli, like clothing, become painful).
Chronic fatigue is the second pillar, affecting about 76% of people with the condition. This isn't ordinary tiredness; it's a profound exhaustion that makes simple tasks feel monumental and can interfere with work and social life.
Non-restorative sleep is the third major symptom. Despite sleeping for long hours, you wake up feeling as if you haven't rested at all. Research shows that deep sleep stages are frequently interrupted, preventing the body from repairing itself.
This creates a vicious cycle: poor sleep worsens pain and fatigue, which in turn makes it harder to sleep. Managing fibromyalgia effectively means finding ways to break this cycle.
The Widespread and Unique Nature of Fibromyalgia Pain
Explaining fibromyalgia pain can be difficult because it's constantly shifting and hard to pinpoint. The symptoms of fibromyalgia create a type of pain that is both widespread and unpredictable.
How Fibromyalgia Pain Feels
People describe their pain in various ways: a deep, muscular aching, a burning sensation, or stabbing and shooting pains. A key feature is that the pain migrates, moving from shoulders to hips to legs from one day to the next. Morning stiffness is also common, making it hard to get moving.
Your body's pain sensitivity is also amplified. This manifests in two ways:
- Hyperalgesia: Things that should hurt a little, like bumping into a table, hurt a lot more.
- Allodynia: Things that shouldn't hurt at all, like a light touch or the weight of clothing, become painful.
These heightened sensitivities require constant adjustments to steer daily life, from avoiding hugs to wearing only the softest fabrics.
Fibromyalgia Pain vs. Other Types of Pain
Understanding how fibromyalgia pain differs from other types is key to finding effective treatments.
Unlike arthritis pain, which is caused by joint inflammation, fibromyalgia pain originates in the central nervous system. There is no visible swelling or redness, even though the pain can be intense.
Unlike acute tissue damage from an injury, which is localized and heals over time, fibromyalgia pain is widespread and chronic, lasting for months or years. It doesn't stem from tissue damage but from how your nervous system processes pain signals.
Because the origin is different, fibromyalgia is classified as a soft tissue pain condition, not an inflammatory one. Traditional anti-inflammatory medications often don't work because they don't address the root cause in the nervous system. This is why exploring different approaches, from lifestyle changes to topical relief, is essential. For more ideas, our guide can help: Beyond Meds: Natural Ways to Ease Fibromyalgia Symptoms.
Beyond the Pain: Cognitive and Emotional Symptoms of Fibromyalgia
Fibromyalgia extends beyond physical discomfort, affecting how you think and feel. These cognitive and emotional symptoms of fibromyalgia can be as debilitating as the pain itself.
What is 'Fibro Fog'?
"Fibro fog" is the term for the cognitive dysfunction that accompanies fibromyalgia. It's a persistent mental cloudiness that makes thinking clearly feel like wading through syrup. Key features include:
- Memory problems: Forgetting names, appointments, or losing your train of thought.
- Difficulty concentrating: Struggling to read, work, or follow conversations.
- Slowed speech and word-finding issues: Knowing what you want to say but being unable to find the right words.
This mental cloudiness can impact work performance, relationships, and simple daily tasks, requiring intense effort to overcome.
The Emotional and Mental Health Impact
Living with an invisible, chronic illness takes a significant emotional toll. Anxiety and depression are common, with over 43% of people with fibromyalgia requiring medication for these conditions. The constant battle with pain and fatigue, coupled with the unpredictability of symptoms, naturally leads to anxiety.
Stress creates a vicious cycle: it can trigger symptom flare-ups, while the condition itself is a major source of stress. This keeps the body's stress response system on high alert.
The frustration of having an invisible illness is immense. It can lead to feelings of isolation when others don't understand your struggle. Managing these emotional aspects is just as crucial as treating the physical symptoms. If you're struggling, know that support is available. Learn about managing chronic illness and find resources to help you cope.
Systemic Impact: How Fibromyalgia Affects the Whole Body
Fibromyalgia doesn't confine itself to one area; its symptoms of fibromyalgia can affect nearly every system in the body, creating challenges far beyond pain and fatigue.
Headaches, GI Issues, and Sensory Overload
Many people with fibromyalgia also struggle with other debilitating conditions:
- Headaches: Between 45% and 80% of patients experience frequent migraine or tension-type headaches, often originating from trigger points in the neck and shoulders.
- Digestive Issues: Over 50% have a functional gastrointestinal disorder, most commonly Irritable Bowel Syndrome (IBS). This can cause abdominal pain, bloating, and unpredictable constipation or diarrhea.
- Sensory Overload: The nervous system often amplifies all sensory input. Bright lights, everyday noises, and strong odors can become overwhelming or painful. Many also struggle with temperature regulation, feeling too hot or cold.
Living with these sensitivities requires constant management of your environment, which can be exhausting.
Understanding the Less Common Symptoms of Fibromyalgia
Fibromyalgia can also manifest in other surprising ways, which vary greatly from person to person. These less common symptoms of fibromyalgia are just as real and can include:
- Restless Legs Syndrome: An irresistible urge to move your legs, especially at night.
- Numbness and Tingling (Paresthesia): Sensations of pins and needles in the hands, feet, arms, or legs.
- Bladder Issues: Increased urinary frequency, urgency, or pain.
- Jaw Pain (TMJ): Chronic pain and dysfunction in the jaw joint.
- Dizziness and Balance Problems: Feelings of lightheadedness or unsteadiness.
- Skin Sensitivities: Unexplained burning, itching, rashes, or hives.
For localized nerve pain that can accompany these symptoms, topical relief can be a valuable tool. To learn more, Explore a comprehensive guide to nerve pain relief creams.
Triggers, Diagnosis, and Living with Fibromyalgia
Living with fibromyalgia involves navigating unpredictable symptoms. Understanding what triggers flare-ups and how the condition is diagnosed can empower you to manage your health more effectively.
What Triggers or Worsens Fibromyalgia Symptoms?
Periods of increased pain and fatigue are called "flare-ups." While sometimes random, they are often linked to specific triggers. Common triggers for the symptoms of fibromyalgia include:
- Physical or emotional trauma: A car accident, surgery, infection, or significant psychological stress can precede the onset of symptoms.
- Stress: Emotional strain from work or relationships can amplify pain signals.
- Weather changes: Many people report worse symptoms in cold, damp conditions.
- Hormonal fluctuations: Menstrual cycles, pregnancy, and menopause can influence symptom severity.
- Overexertion: Doing too much one day can lead to a severe flare-up the next.
- Poor sleep: This is both a symptom and a trigger, creating a vicious cycle.
Keeping a symptom journal can help you identify your personal triggers.
How Fibromyalgia is Diagnosed
There is no single test for fibromyalgia, so diagnosis can be a lengthy process. It's a "diagnosis of exclusion," meaning doctors must first rule out other conditions with similar symptoms, like rheumatoid arthritis or lupus.
Diagnosis follows criteria from the American College of Rheumatology. A doctor will use the Widespread Pain Index (WPI) to map where you've had pain and the Symptom Severity (SS) Scale to assess fatigue, sleep issues, and cognitive problems. To be diagnosed, your symptoms of fibromyalgia must have been present for at least three months.
Blood tests are used not to find fibromyalgia, but to exclude other conditions. When tests are normal but symptoms persist, fibromyalgia is the likely diagnosis. If you're struggling to get answers, don't give up. You can also explore research studies for new options: Find a Clinical Trial for Fibromyalgia.
Frequently Asked Questions about Fibromyalgia Symptoms
How are fibromyalgia symptoms diagnosed?
Fibromyalgia diagnosis is clinical, based on your medical history and a physical exam. There is no single lab test. Instead, doctors use criteria from the American College of Rheumatology, including the Widespread Pain Index (WPI) and the Symptom Severity (SS) scale. Your widespread pain and other symptoms of fibromyalgia must be present for at least three months. The process also involves a "diagnosis of exclusion," where tests are run to rule out other conditions like lupus or rheumatoid arthritis.
Do fibromyalgia symptoms ever go away?
Fibromyalgia is a chronic condition with no current cure, but its symptoms are not constant. Most people experience fluctuations, with periods of increased severity ("flare-ups") and periods where symptoms are milder ("remission"). The goal of management is to increase the duration of remission and reduce the impact of flares. With effective strategies, many people significantly improve their quality of life.
What is the difference between fibromyalgia pain and regular muscle soreness?
Regular muscle soreness (DOMS) is localized, temporary, and caused by physical exertion. It resolves in a few days as muscles repair. Fibromyalgia pain is entirely different. It is widespread, chronic, and caused by amplified pain signals in the central nervous system, not muscle damage. This is why it's accompanied by other symptoms like profound fatigue and "fibro fog," and why even a light touch can be painful (allodynia). The underlying cause is far more complex, requiring a comprehensive management approach.
Managing Symptoms and Moving Forward
The symptoms of fibromyalgia create a complex reality of widespread pain, fatigue, mental cloudiness, and other systemic issues. Because the condition is so personal, a one-size-fits-all solution is rarely effective. However, understanding your unique symptoms and triggers is a powerful first step toward taking an active role in your care.
The path forward involves building a personalized management plan with healthcare professionals. This may include lifestyle adjustments, stress management, gentle movement, and exploring different treatment options.
At Neuropasil, we understand chronic pain. Our natural, fast-acting topical creams are designed to provide targeted, soothing relief. While not a cure for fibromyalgia, many in our community use Neuropasil to ease the muscle aches and nerve discomfort that accompany the condition, helping to make each day more manageable. There is hope for living a life with less pain and more comfort.
For more information on how topical relief can fit into your plan, explore a comprehensive guide to nerve pain relief creams.
References
- Centers for Disease Control and Prevention. (2020). Basics of Fibromyalgia. https://www.cdc.gov/arthritis/basics/fibromyalgia.htm
- Cleveland Clinic. Fibromyalgia. https://my.clevelandclinic.org/health/diseases/4844-fibromyalgia
- Erdrich, S., et al. (2020). A systematic review of the association between fibromyalgia and functional gastrointestinal disorders. Therapeutic Advances in Gastroenterology. https://journals.sagepub.com/doi/full/10.1177/1756284820977402
- FMAware. Fibromyalgia Symptoms. https://www.fmaware.org/fibromyalgia-symptoms/
- FMNetNews. Common Symptoms. https://fmnetnews.com/fibro-basics/symptoms/common
- Healthline. Signs of Fibromyalgia. https://www.healthline.com/health/fibromyalgia/signs-of-fibromyalgia
- Mayo Clinic. Fibromyalgia. https://www.mayoclinic.org/diseases-conditions/fibromyalgia/symptoms-causes/syc-20354780
- MedlinePlus. Fibromyalgia. https://medlineplus.gov/ency/article/000427.htm
- Mount Sinai. Fibromyalgia. https://www.mountsinai.org/health-library/diseases-conditions/fibromyalgia
- NHS. Fibromyalgia: Symptoms. https://www.nhs.uk/conditions/fibromyalgia/symptoms/
- Penn, I-W., et al. (2019). Bidirectional association between migraine and fibromyalgia: Retrospective cohort analyses of two populations. BMJ Open. https://bmjopen.bmj.com/content/9/4/e026581
- Vincent, A., et al. (2013). Beyond pain in fibromyalgia: insights into the symptom of fatigue. Arthritis Research & Therapy. https://arthritis-research.biomedcentral.com/articles/10.1186/ar4395
- Walitt, B., et al. (2015). The Prevalence and Characteristics of Fibromyalgia in the 2012 National Health Interview Survey. PLOS ONE. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0138024
- WebMD. Fibromyalgia Symptoms and Types. https://www.webmd.com/fibromyalgia/guide-chapter-fibromyalgia-symptoms-types
- Wolfe, F., et al. (2010). The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care & Research. https://www.rheumatology.org/portals/0/files/2010preliminarydiagnostic_criteria.pdf
- Yang T-Y, et al. (2017). Risk for irritable bowel syndrome in fibromyalgia patients: A national database study. Medicine (Baltimore). https://journals.lww.com/md-journal/Fulltext/2017/04070/NoticeofRepublication_RiskforIrritableBowel.51.aspx















