When That Chest Ache Isn't Your Heart
Chest muscle ache is pain in the muscles, cartilage, or bones of your chest wall. While any chest pain is concerning, it's a common issue, with over half of the 6.5 million annual ER visits for chest pain in the U.S. having non-cardiac causes.
Quick Answer: What You Need to Know
- Most common causes: Muscle strain from exercise or lifting, costochondritis (inflammation of rib cartilage), persistent coughing, or poor posture
- Key difference from heart pain: Chest muscle ache is localized, worsens with movement or touch, and doesn't radiate to your arm or jaw
- When to worry: Seek emergency care if pain feels crushing, spreads to your arms/jaw, or comes with shortness of breath, sweating, or nausea
- Relief options: Rest, gentle stretching, heat/cold therapy, and topical pain relief creams
Understanding the difference between muscular chest pain and cardiac chest pain can save you unnecessary worry—and knowing when to seek help could save your life.
Chest muscle aches typically feel sharp or tender when you press on the area, worsen with deep breaths or twisting, and stay in one spot. In contrast, heart-related pain often feels like pressure or squeezing, may spread across your chest or down your arm, and doesn't change with movement.
The good news? Chest muscle ache usually improves with simple at-home care within a few days to weeks. The key is understanding its cause and how to address it effectively.
I'm Tony Enrico. Through my work with Neuropasil, I've helped thousands find relief from muscle and nerve pain. I've seen how combining knowledge with effective, natural relief can restore comfort and confidence for people from all walks of life experiencing chest muscle ache and other musculoskeletal issues.
Chest muscle ache terminology:
Identifying the Causes of Your Chest Muscle Ache
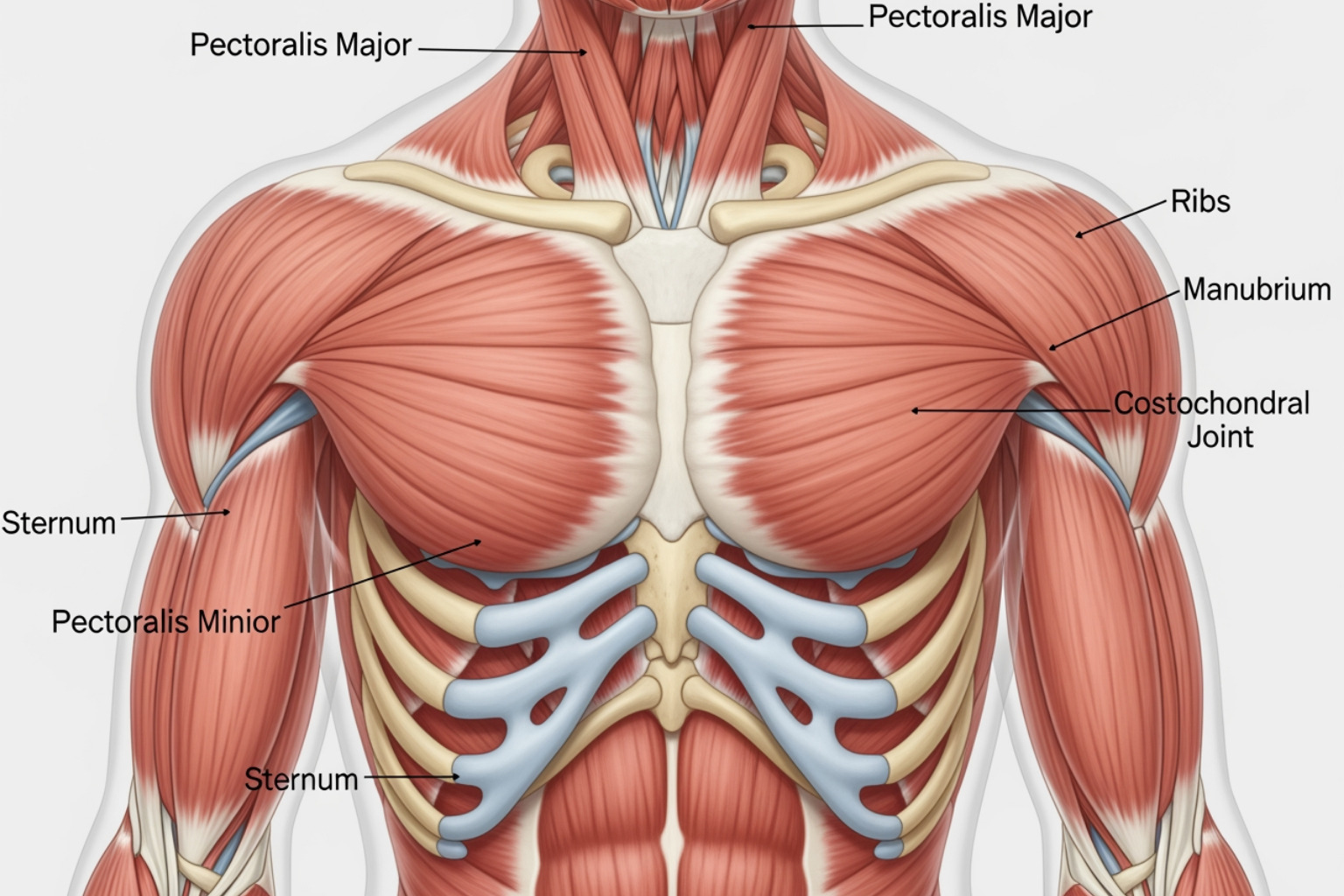
Most chest muscle ache comes from the muscles, bones, and cartilage of your chest wall—not your heart. Understanding the cause of your discomfort is the first step toward feeling better.
The most common culprit is muscle strain. This occurs when you overexert your chest muscles by lifting heavy objects, exercising too intensely, or even from a persistent cough. The microscopic tears in muscle fibers result in soreness, stiffness, and sharp pain.
Another frequent cause is costochondritis, an inflammation of the cartilage connecting your ribs to your breastbone. The pain is often sharp, located on the left side of the chest, and worsens with deep breaths, coughing, or pressure. A related but less common condition, Tietze syndrome, is similar but also involves visible swelling.
Daily habits also play a role. Poor posture, like hunching over a desk, strains chest wall muscles and joints over time. Anxiety and stress cause muscle tension throughout the body, including the chest. The rapid breathing during a panic attack can exhaust chest muscles, leading to physical pain. Learn more about how stress affects your body in our guide on Muscle Tension.
Sometimes the cause is as simple as intense coughing from a cold or overexertion from an unfamiliar activity, like a weekend of spring cleaning. Your chest muscles work harder than you think during these activities.
What is Costochondritis?
Costochondritis is inflammation of the cartilage at the costosternal joints, where your ribs meet your breastbone (sternum). This cartilage allows your rib cage to expand when you breathe, so inflammation can make every breath painful.
While the exact cause is often unknown, common triggers include physical strain from heavy lifting or repetitive movements, severe respiratory infections with persistent coughing, direct chest trauma, and certain types of arthritis. The pain is typically sharp or aching in the front of the chest, often on the left side. It worsens with deep breaths, coughing, or pressure on the area and can sometimes radiate to the arms and shoulders. It is most common in women over 40.
Diagnosis involves a physical exam where a doctor checks for tenderness along the rib-breastbone junctions. To rule out cardiac issues, they may order an X-ray, EKG, or blood work. Reassuringly, costochondritis usually resolves on its own in a few weeks to months. For more details, the NHS provides detailed information on Costochondritis.
How is a chest muscle ache different from other pains?
Knowing how chest muscle ache differs from heart-related pain can give you peace of mind or help you recognize an emergency.
Chest muscle ache has telltale characteristics. The pain is localized—you can usually point to exactly where it hurts. When you press on that spot, the pain gets worse. This tenderness to touch is a key sign that the pain is musculoskeletal.
The pain also worsens with movement. Twisting your torso, reaching overhead, or taking a deep breath intensifies the discomfort. The sensation itself tends to be sharp or aching, not the crushing pressure associated with heart problems.
Musculoskeletal pain usually improves with rest, while heart pain does not change whether you're moving or still.
If you're dealing with chest discomfort after exercise, it might simply be normal Muscle Soreness. But always take new or concerning chest pain seriously. When in doubt, get it checked out. Your peace of mind is worth it, and if it is something serious, early treatment makes all the difference.
Is It a Heart Attack or a Harmless Ache?
Feeling chest pain is understandably concerning, and you should never dismiss it. While over half of ER visits for chest pain are for non-cardiac causes, it's critical not to self-diagnose.
The difference between a chest muscle ache and cardiac pain comes down to several key characteristics.
Musculoskeletal chest pain is usually localized to a specific spot. The sensation is sharp, stabbing, or a dull ache that intensifies when you press on the area. It gets worse when you move, breathe deeply, or cough, but it stays in one place.
Heart-related pain behaves differently. It often feels like a crushing or squeezing sensation that's hard to pinpoint. This pain frequently radiates to the left arm, jaw, neck, or back. It doesn't change when you press on your chest or shift position, and it often comes with other symptoms like shortness of breath, cold sweats, nausea, or dizziness.
The duration also tells a story. A chest muscle ache can last from seconds to weeks, while cardiac pain typically persists for minutes and requires immediate attention. Muscular pain often improves with rest, while cardiac pain may only respond to specialized medications.
Red Flag Symptoms: When to Seek Emergency Care
Let me be direct here—if you experience any of the following symptoms, call 911 immediately. Don't second-guess yourself. Don't wait to see if it gets better. Don't have a friend or family member drive you to the hospital. Call for an ambulance. In a cardiac emergency, every single minute matters.
Watch for crushing chest pressure or a squeezing sensation that feels like an elephant sitting on your chest. If pain spreads to your arm—especially your left arm—jaw, neck, or back, that's a red flag. Shortness of breath that makes it difficult to catch your breath needs immediate attention. Dizziness or feeling like you might pass out, combined with chest discomfort, is serious. Cold sweats that soak through your shirt, nausea or vomiting, or a fast, irregular pulse alongside chest pain—all of these warrant emergency care.
Even if the pain doesn't perfectly match what you think a heart attack should feel like, trust your instincts. I've spoken with countless people who dismissed their symptoms because "it didn't feel quite right" or "I didn't want to overreact." The emergency room doctors would much rather see you and send you home reassured than have you wait too long.
For non-emergency guidance, UK residents can get help from 111 online, and you can read more about distinguishing different types of chest pain at Michigan Medicine's resource on when chest pain isn't a heart attack.
Understanding your chest muscle ache symptoms
Once a medical professional has ruled out an emergency, you can identify the specific characteristics of your chest muscle ache. Musculoskeletal chest pain follows a pattern: it intensifies with a deep breath, twisting your torso, or reaching. Pressing on your sternum or between your ribs reproduces the pain, a key sign it's not cardiac-related. You might feel general soreness after physical activity or hard coughing, which strains the chest wall. The pain is also localized; you can pinpoint the exact spot that hurts, which is a reassuring sign it's coming from the chest wall structures. Understanding these patterns helps you manage recovery and gives you peace of mind. For more context, our article on Muscle Pain offers additional insights.
Your Guide to At-Home Relief and Management
After a healthcare professional confirms your chest muscle ache is musculoskeletal, you can take several steps at home to find comfort and speed up recovery.
The first principle is simple: rest. This means giving your chest muscles a break from whatever aggravated them. If you strained yourself lifting, skip the weightlifting for a few days. If your chest aches from a cough, support your chest with a pillow when you need to cough.
Activity modification is your friend. You're not abandoning exercise forever; you're just being smart about what your body needs. Think of it as a strategic pause. Avoid strenuous exercise involving your chest muscles until the pain significantly improves.
Once the initial sharp pain settles, gentle stretching becomes incredibly valuable. These stretches help open up your chest, improve flexibility, and reduce tightness. A doorway stretch is one of the most effective: place your forearms on either side of a doorframe and gently lean forward until you feel a comfortable stretch across your chest. Hold for 15-30 seconds and repeat a few times a day.

How to manage chest muscle ache pain at home
Combining several natural approaches creates the most effective comfort routine for chest muscle ache.
Heat and cold therapy form the foundation. In the first 24-48 hours, apply a cold pack wrapped in a towel for 10-20 minutes every few hours to reduce inflammation. After two days, or for chronic achiness, switch to warmth. A heating pad, warm compress, or warm bath can relax tight muscles and increase blood flow to promote healing.
Over-the-counter pain relievers like ibuprofen or naproxen can help manage pain and inflammation. Acetaminophen is another option for pain relief. Always follow dosage instructions and check with your doctor if you have underlying health conditions.
Deep breathing exercises are important for preventing stiffness. Support your chest with a pillow and take slow, gentle deep breaths several times a day.
If poor posture is a factor, address your workspace. Ensure your monitor is at eye level and your shoulders are relaxed. Set a reminder to stand and stretch hourly.
For comprehensive strategies, our guide on the Best Ways to Relieve Muscle Aches with Physical Activity and Healthy Living offers practical advice.
The Role of Topical Treatments
When your chest muscle ache is localized, topical treatments can provide remarkably effective relief. Unlike oral medications that travel through your entire system, natural topical analgesics deliver soothing ingredients directly where you need them most.
Plant-based pain relief creams have come a long way. At Neuropasil, we've formulated our creams for targeted relief, combining ingredients like menthol, aloe, and urea to create fast-acting comfort without a greasy residue. Menthol creates a cooling sensation that helps interrupt pain signals while providing analgesic benefits.
What makes topical treatments particularly appealing for chest muscle pain is their localized relief. You're applying the cream directly to the sore area—whether along your ribs, near your sternum, or across your pectoral muscles—for concentrated relief right where it matters. There are no systemic side effects, and you can reapply as needed.
When choosing a topical treatment, look for products that work quickly and absorb without leaving your clothes sticky. The best formulations penetrate the skin to reach the underlying muscle tissue where the pain originates.
To understand how these topical solutions work, explore our article Beyond the Pill: How Topical Anti-Inflammatories Soothe Your Aches. And if you're curious about what distinguishes effective muscle rubs, The Ultimate Guide to Good Muscle Rubs provides detailed insights.
Frequently Asked Questions about Chest Wall Pain
Here are answers to the most common questions about chest muscle ache to help put your mind at ease.
How long does a pulled chest muscle take to heal?
The healing time depends on the severity of the strain. I've seen people recover in a few days, while others need several weeks.
For mild strains, where muscle fibers are slightly overstretched, recovery can take a few days to two weeks. These respond well to rest, ice, heat, and gentle stretching.
Moderate strains involve more significant tearing and can take several weeks to a couple of months to heal. These require more patience. It's common to push too hard too soon and cause a setback.
Severe strains are rare but can involve a complete muscle tear, potentially requiring medical intervention and months of rehabilitation.
The key to faster healing is giving your body what it needs. Rest is crucial initially, followed by a gradual return to activity as pain allows. Our guide on Recover Like a Pro: Strategies for Faster Muscle Healing offers practical strategies.
Can costochondritis lead to long-term problems?
Here's some good news: for most people, costochondritis is temporary and causes no lasting damage. Most cases resolve on their own within a few weeks to a few months.
However, some people experience chronic costochondritis, where the pain lingers or recurs. Even in these cases, the condition itself isn't damaging your body. The main issue is managing the ongoing discomfort, which can impact your quality of life.
If you're dealing with persistent chest muscle ache from costochondritis, follow up with your doctor to rule out other issues and explore additional pain management options, such as physical therapy. Stay proactive about your comfort.
What is the difference between costochondritis and Tietze syndrome?
People often use these terms interchangeably, but there's a clear, visible distinction.
Costochondritis involves inflammation of the cartilage where your ribs connect to your breastbone. You'll feel pain and tenderness, but you won't see any swelling. It's more common in women over 40 and can affect multiple rib joints.
Tietze syndrome, on the other hand, includes the same symptoms plus noticeable swelling at the affected joint. You can see or feel a raised area. Tietze syndrome is less common, typically affects just one joint, and tends to appear in younger people. It affects men and women equally.
Think of Tietze syndrome as costochondritis's more dramatic cousin. Both conditions involve cartilage inflammation and are treated similarly, with a focus on reducing inflammation, managing pain, and allowing time to heal. The at-home care strategies we've discussed can help ease discomfort for both.
Conclusion: Taking Control of Your Chest Health
While any chest muscle ache is concerning, many cases are musculoskeletal, not cardiac. Differentiating between them is a powerful tool for your peace of mind.
Remember the key takeaways: a chest muscle ache is often localized, worsens with movement or touch, and feels sharp or aching. Heart-related pain typically feels crushing or squeezing, may radiate, and is often associated with other severe symptoms like shortness of breath or sweating. When in doubt, always prioritize seeking immediate medical attention by calling 911.
For non-emergency chest muscle aches, effective home treatments like rest, hot/cold therapy, gentle stretching, and over-the-counter pain relievers can provide significant relief. For targeted, soothing relief from muscle soreness and localized pain, consider a natural topical cream like Neuropasil. Our unique blend of Aloe, Urea, and Menthol is designed to deliver fast, effective comfort directly to the source of your discomfort.
Taking proactive steps to understand your symptoms and manage your pain empowers you to regain control of your comfort and well-being. Don't let a chest muscle ache hold you back from living your fullest life.
Discover our natural pain relief solutions and find the comfort you deserve.
References
The information in this article is backed by credible medical and health resources to ensure accuracy and reliability. Understanding chest muscle ache requires drawing on established medical knowledge, and we've consulted the following trusted sources:
We referenced the comprehensive 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain, a detailed report from the American College of Cardiology and American Heart Association Joint Committee on Clinical Practice Guidelines. This authoritative document provides the clinical framework for distinguishing cardiac from non-cardiac chest pain. You can access the full guideline through the American Heart Association journal.
For specific information on costochondritis, we turned to the NHS's dedicated resource on the condition, which offers patient-friendly explanations of symptoms, causes, and treatment approaches. Their guidance is available at NHS Costochondritis. We also consulted NHS inform for additional perspectives on chest and rib problems.
The Cleveland Clinic's overview of musculoskeletal chest pain provided valuable insights into the non-cardiac causes of chest discomfort, helping us explain how to differentiate between muscle-related aches and other types of pain. Their resource can be found at Cleveland Clinic Musculoskeletal Chest Pain.
MedlinePlus, a trusted service of the U.S. National Library of Medicine, offered comprehensive information on both general chest pain and costochondritis specifically. Their evidence-based articles are accessible at MedlinePlus Chest Pain and MedlinePlus Costochondritis.
The University of Michigan Health article on noncardiac chest pain helped us understand when chest pain isn't a heart attack, providing clarity on the causes and symptoms that distinguish musculoskeletal issues from cardiac emergencies. Read their insights at Michigan Medicine.
These references represent the medical consensus on chest wall pain and ensure that the information we've shared with you is both accurate and actionable. When it comes to your health, especially something as potentially serious as chest pain, we believe in providing information you can trust.















