Why Understanding Peripheral Neuropathy Causes Matters
What causes peripheral neuropathy is a question that affects millions of people worldwide. The answer isn't simple—peripheral neuropathy can stem from dozens of different sources, ranging from common diseases like diabetes to lifestyle factors like alcohol use, vitamin deficiencies, infections, medications, injuries, and even inherited conditions.
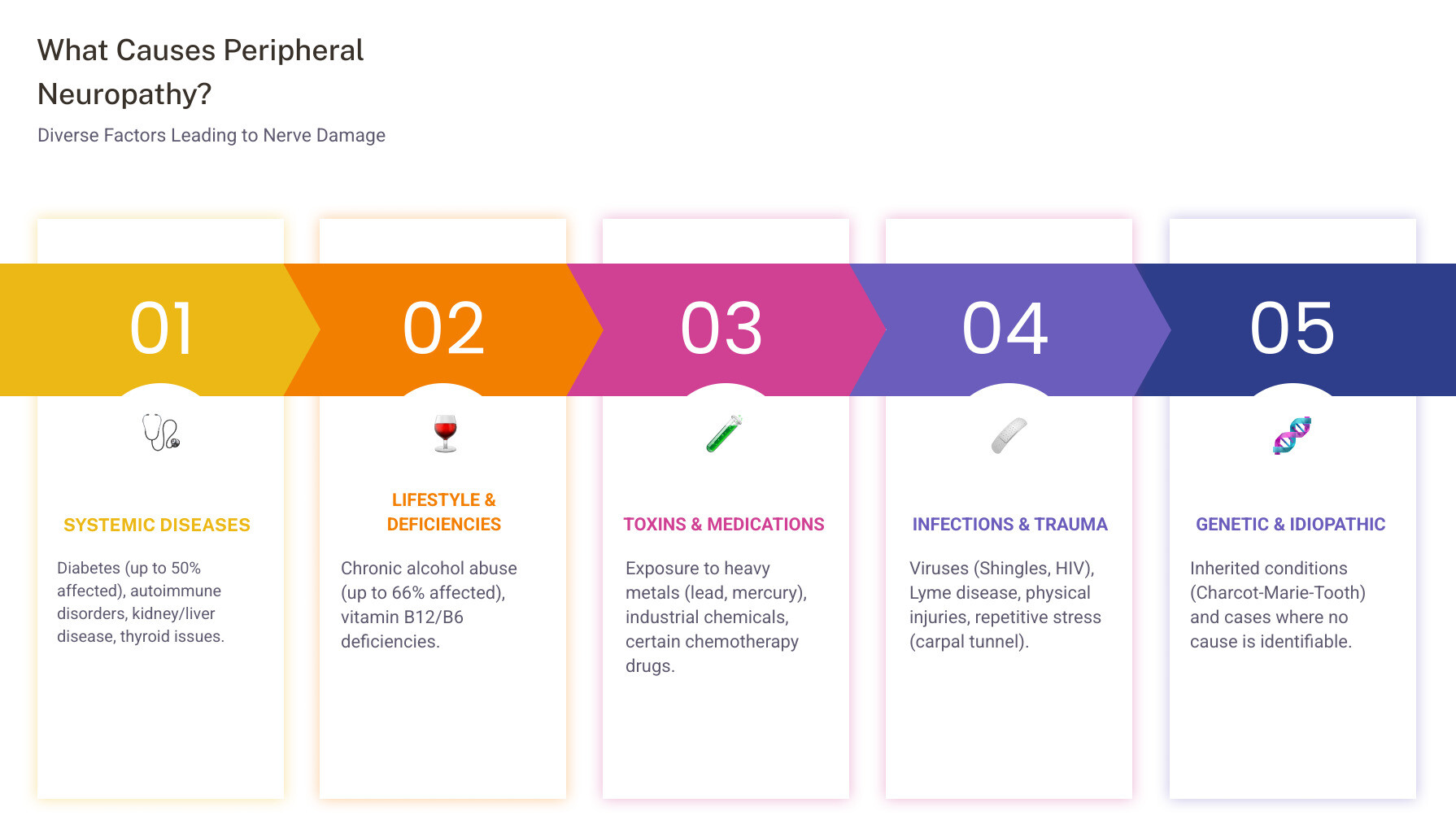
Quick Answer: Common Causes of Peripheral Neuropathy
- Diabetes (the leading cause, affecting up to 50% of people with diabetes)
- Chronic alcohol abuse (affecting up to 66% of heavy drinkers)
- Vitamin deficiencies (especially B12, B6, and vitamin E)
- Autoimmune diseases (lupus, rheumatoid arthritis, Sjögren's syndrome)
- Infections (shingles, Lyme disease, HIV, hepatitis C)
- Medications (chemotherapy drugs, certain antibiotics)
- Physical trauma (injuries, repetitive stress like carpal tunnel syndrome)
- Toxin exposure (lead, mercury, arsenic, industrial chemicals)
- Inherited conditions (Charcot-Marie-Tooth disease)
- Idiopathic (no identifiable cause in some cases)
Peripheral neuropathy happens when the nerves outside your brain and spinal cord—your peripheral nervous system—become damaged or diseased. Think of your nervous system like the wiring in a house. When those wires get frayed or broken, the signals between your brain and the rest of your body get disrupted. The result? Numbness, tingling, burning pain, muscle weakness, and a host of other symptoms that can significantly impact your daily life.
The numbers tell an important story. About 2.4% of people globally have some form of peripheral neuropathy, and that number jumps to between 5% and 7% among people aged 45 and older. These aren't just statistics—they represent millions of people searching for answers and relief.
I'm Tony Enrico, and at Neuropasil, we've dedicated ourselves to understanding what causes peripheral neuropathy so we can provide real relief to those suffering from nerve pain. Through years of research and working directly with people experiencing nerve discomfort, we've seen how identifying the underlying cause is the first step toward effective management and relief.
Basic what causes peripheral neuropathy terms:
What Causes Peripheral Neuropathy? The Main Culprits
This section explores the diverse factors leading to nerve damage, from common diseases to lifestyle choices. Understanding these root causes is crucial for effective treatment and management. When we talk about what causes peripheral neuropathy, we're delving into a complex web of medical conditions, environmental exposures, and genetic predispositions that can all contribute to nerve damage.
Systemic Diseases: The Most Common Cause of Peripheral Neuropathy
Systemic diseases are conditions that affect multiple organs or the entire body, and they are frequently at the heart of peripheral neuropathy. The most common culprit we encounter, particularly in the United States, is diabetes.
Diabetes
In the U.S., diabetes is the most common cause of peripheral neuropathy, eventually affecting about half of all people with this condition. Whether it's Type 1 or Type 2 diabetes, prolonged high blood sugar levels are incredibly damaging to the delicate peripheral nerves. This damage occurs because liftd glucose and fats like triglycerides in the blood impair the small blood vessels that supply nerves with essential oxygen and nutrients. Over time, this chronic deprivation leads to inflammation and degeneration of the nerve fibers.
The risk of developing diabetic neuropathy increases with the duration of diabetes and how well blood sugar levels are controlled. Up to one-half of people with diabetes have peripheral neuropathy, and many will experience pain from this nerve damage. Risk factors for polyneuropathy in diabetics include poorly controlled blood sugar, smoking, regular heavy alcohol consumption, and being over 40. Managing diabetes effectively is often the first and most critical step in preventing or slowing the progression of diabetic neuropathy. You can find more detailed information on diabetic neuropathy from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) here.
Autoimmune Diseases
Our immune system, designed to protect us, can sometimes turn against our own tissues, including our nerves. This is the case with autoimmune diseases, which are significant contributors to peripheral neuropathy.
- Lupus: A chronic inflammatory disease that can affect various body parts, including the nervous system.
- Rheumatoid Arthritis: Primarily affecting joints, this inflammatory condition can also lead to nerve damage.
- Sjögren's Syndrome: This autoimmune disorder primarily targets moisture-producing glands but can also cause nerve damage. It's estimated that one to four million people in America suffer from Sjögren’s syndrome, and a significant portion may experience neuropathy.
- Guillain-Barré Syndrome (GBS): A rare disorder where the immune system attacks the peripheral nerves, often triggered by an infection.
- Chronic Inflammatory Demyelinating Polyneuropathy (CIDP): A long-term neurological disorder characterized by progressive weakness and impaired sensory function due to damage to the myelin sheath of peripheral nerves.
- Vasculitis: Inflammation of blood vessels can restrict blood flow to nerves, causing damage.
Other Chronic Health Conditions
Beyond diabetes and autoimmune disorders, several other chronic conditions can answer the question of what causes peripheral neuropathy:
- Chronic Kidney Disease: As kidney function declines, toxins can build up in the blood, damaging nerves. This can lead to uremic neuropathy, affecting 50%-100% of people experiencing kidney disease.
- Chronic Liver Disease: Similar to kidney disease, impaired liver function can lead to an accumulation of neurotoxic substances.
- Underactive Thyroid (Hypothyroidism): An underactive thyroid can lead to fluid retention and swelling, which can put pressure on nerves.
- Monoclonal Gammopathy of Undetermined Significance (MGUS): This condition involves the production of abnormal proteins that can sometimes damage nerves.
- Cancers: Certain cancers, such as lymphoma and multiple myeloma, can directly cause neuropathy by infiltrating nerves or through paraneoplastic syndromes, where the immune system reacts to the cancer and inadvertently attacks nerves.
- Amyloidosis: A rare disease where abnormal proteins called amyloid build up in organs and tissues, including nerves.
Lifestyle Factors, Toxins, and Deficiencies
Sometimes, the choices we make or the environments we live in can directly impact our nerve health.
Alcohol Abuse
Chronic alcohol abuse is one of the most frequent causes of neuropathy. Alcohol can have a direct toxic effect on nerve tissue, and it often leads to nutritional deficiencies, particularly B vitamins, which are crucial for nerve health. It is estimated that as many as 66% of individuals with chronic alcohol abuse may suffer from alcoholic polyneuropathy. The good news is that reducing or stopping alcohol intake can sometimes lead to an improvement in symptoms.
Nutritional Deficiencies
Our nerves need a steady supply of vitamins and minerals to function correctly. Deficiencies in certain nutrients can lead to nerve damage:
- Vitamin B12 Deficiency: Essential for nerve maintenance and the production of myelin (the protective sheath around nerves). Low B12 levels can be caused by poor diet, malabsorption issues, or even certain medications like metformin. Your doctor may perform tests to check for low vitamin B12 levels.
- Vitamin B6 Imbalance: This one's tricky. Both too little AND too much Vitamin B6 can cause neuropathy. While B6 is vital for nerve function, excessive intake (often from supplements) can become neurotoxic.
- Vitamin E and Niacin Deficiencies: These are also important for nerve health, and their absence can contribute to neuropathy.
Exposure to Toxins
Environmental or occupational exposure to certain toxins can directly damage peripheral nerves.
- Heavy Metals: Lead, mercury, and arsenic are notorious for their neurotoxic effects.
- Industrial Chemicals: Solvents, pesticides, and other chemicals found in certain workplaces can be harmful. For example, acrylamide, hexacarbons, and ethylene oxide are known culprits.
Medications, Infections, and Physical Trauma
Sometimes, the very treatments designed to help us, or external forces, can inadvertently cause nerve damage.
Medications
Certain medications can have peripheral neuropathy as a side effect. It's always worth discussing with your healthcare provider if you suspect a medication is contributing to your nerve symptoms.
- Chemotherapy Drugs: Many chemotherapy agents used to treat cancer are known to cause neuropathy. This is often referred to as chemotherapy-induced peripheral neuropathy (CIPN).
- Antibiotics: Some antibiotics, like metronidazole and nitrofurantoin, can lead to nerve damage.
- Other Drugs: Phenytoin (an anti-seizure medication), amiodarone (for heart rhythm issues), and thalidomide (used for certain cancers and inflammatory conditions) are also associated with neuropathy. Even some depression medications can sometimes be implicated.
Infections
Various infections can directly attack or trigger an immune response that damages peripheral nerves.
- Shingles (Herpes Zoster): The varicella-zoster virus, which causes chickenpox, can reactivate later in life as shingles, leading to painful postherpetic neuralgia.
- Lyme Disease: Caused by bacteria transmitted by ticks, Lyme disease can manifest with neurological symptoms, including neuropathy.
- HIV/AIDS: The virus itself, as well as some medications used to treat HIV, can cause peripheral neuropathy.
- Hepatitis B and C: These viral infections can sometimes lead to nerve damage.
- Other Infections: Leprosy, diphtheria, and West Nile virus are also known causes.
Physical Trauma
Direct physical damage to nerves is a straightforward answer to what causes peripheral neuropathy.
- Traumatic Injuries: Accidents, falls, sports injuries, or even surgical complications can directly sever, crush, or compress nerves.
- Repetitive Stress: Repeated pressure or movements can lead to nerve damage over time. A classic example is carpal tunnel syndrome, where the median nerve in the wrist is compressed.
Inherited Disorders and Idiopathic Neuropathy
For some, nerve damage is part of their genetic makeup, while for others, the cause remains a mystery.
Inherited Conditions
Genetic factors can play a significant role. If you have a family history of neuropathy, it's worth exploring inherited conditions.
- Charcot-Marie-Tooth Disease (CMT): This is one of the most common inherited neurological disorders, affecting the peripheral nerves and leading to muscle weakness and sensory loss, primarily in the feet and lower legs, but also in the hands and forearms. To date, mutations in more than 100 genes have been identified as a cause of CMT.
Idiopathic Neuropathy
Sometimes, despite extensive medical evaluation, the cause of peripheral neuropathy cannot be identified. This is referred to as "idiopathic neuropathy." While frustrating, managing the symptoms and preventing further nerve damage still remains the focus.
We understand that navigating these complex causes can be overwhelming. For more insights and information on managing your nerve health, you can explore our blog for more on neuropathy topics.
Recognizing the Signs: Symptoms and Complications
Peripheral neuropathy doesn't always announce itself with a bang. Often, the symptoms begin subtly and progress over time. Understanding these signs is crucial for early detection and intervention.
The symptoms of peripheral neuropathy can vary widely depending on which types of nerves are affected—sensory, motor, or autonomic.
- Gradual onset of symptoms: Many people first notice a gradual onset of numbness, prickling, or tingling in their feet or hands, which can then spread upwards into their legs and arms. This is often described as a "pins and needles" sensation.
- Burning or sharp, jabbing pain: This kind of pain can be intense and persistent, often worsening at night.
- Extreme sensitivity to touch (allodynia): Imagine the weight of a bedsheet causing excruciating pain. This extreme sensitivity to normally non-painful stimuli is called allodynia and is a hallmark of neuropathic pain.
- Muscle weakness: As motor nerves are affected, you might experience weakness in your limbs, difficulty walking, or even muscle twitching and loss of muscle tone.
- Lack of coordination and balance issues: Damage to sensory nerves that help us understand our body's position in space can lead to problems with coordination and an increased risk of falls.

How Peripheral Neuropathy Affects the Body
Peripheral neuropathy impacts the body by disrupting the intricate communication network of the peripheral nervous system. This disruption can manifest in three main ways, depending on which types of nerves are primarily damaged:
-
Sensory Nerve Symptoms: These nerves transmit information about touch, temperature, and pain from your skin to your brain. When damaged, you might experience:
- Numbness or reduced ability to feel pain or temperature changes.
- Tingling, burning, or "pins and needles" sensations.
- Sharp, jabbing, throbbing, or electric-like pain.
- Extreme sensitivity to touch (allodynia).
- Loss of position sense, making it hard to know where your limbs are without looking.
-
Motor Nerve Symptoms: These nerves control muscle movement. Damage can lead to:
- Muscle weakness, cramps, or twitching.
- Loss of muscle tone and muscle atrophy (wasting).
- Difficulty with coordination and balance.
- Problems walking or performing fine motor tasks.
-
Autonomic Nerve Symptoms: These nerves control involuntary functions like heart rate, blood pressure, digestion, and sweating. Damage can result in:
- Heat intolerance due to reduced sweating.
- Abnormal sweating (either too much or too little).
- Digestive problems, such as nausea, vomiting, constipation, or diarrhea.
- Dizziness or lightheadedness when standing up (orthostatic hypotension) due to drops in blood pressure.
- Bladder dysfunction and sexual problems.
Complications
The consequences of ongoing peripheral neuropathy can be severe and significantly impact quality of life:
- Foot Ulcers and Infections: Loss of sensation, particularly in the feet, means you might not feel cuts, blisters, or sores. These unnoticed injuries can become infected, and if left untreated, can lead to severe infections, tissue death (gangrene), and potentially limb amputation, especially in people with diabetes.
- Falls and Fractures: Impaired balance, muscle weakness, and loss of sensation dramatically increase the risk of falls, leading to fractures and other injuries.
- Chronic Pain and Mental Health Impact: Living with persistent nerve pain can be incredibly challenging. The chronic nature of the pain can lead to grief, anxiety, and depression. It's a vicious cycle where pain exacerbates mental health issues, and vice versa.
Diagnosis and Managing Neuropathy Symptoms
If you're experiencing symptoms consistent with peripheral neuropathy, seeking a diagnosis is the first crucial step. The process usually involves a comprehensive approach by your healthcare provider.
Medical History and Physical Exam: Your doctor will ask detailed questions about your symptoms, medical conditions, medications, lifestyle, and family history. A thorough physical exam will assess your reflexes, muscle strength, sensation, and balance.
Neurological Tests: These tests are designed to evaluate nerve function.
Blood Tests: These are often performed to identify underlying conditions that could be causing neuropathy. They may check for:
- Diabetes (blood glucose, HbA1c)
- Vitamin deficiencies (especially B12)
- Thyroid issues
- Kidney or liver dysfunction
- Markers for autoimmune diseases or infections
Nerve Conduction Studies (NCS) and Electromyography (EMG): These are specialized tests that measure the electrical activity of your nerves and muscles.
- NCS: Electrodes are placed on your skin to stimulate nerves with a mild electrical impulse. The speed and strength of the nerve signals are recorded, helping to identify nerve damage and differentiate between demyelinating (myelin sheath damage) and axonal (axon damage) neuropathy.
- EMG: A thin needle electrode is inserted into a muscle to record its electrical activity, both at rest and during contraction. This helps assess muscle health and identify if nerve damage is affecting muscle function.
Nerve Biopsy: In some cases, a small sample of nerve tissue may be removed and examined under a microscope. This can provide detailed information about the type and extent of nerve damage.
What causes peripheral neuropathy to flare up and how can it be managed?
Neuropathy symptoms can sometimes worsen or "flare up" due to various triggers. Managing these triggers and the underlying cause is key to finding relief.
Treating the Underlying Cause: This is the most effective long-term strategy.
- Blood Sugar Control: For diabetic neuropathy, tightly controlling blood glucose levels is paramount. This can prevent further damage and, in early stages, sometimes even reverse some nerve damage.
- Alcohol Cessation: If alcohol abuse is the cause, stopping alcohol consumption is critical.
- Correcting Deficiencies: Addressing vitamin deficiencies through diet or supplements (e.g., B12 injections for severe deficiency) can help nerves recover.
- Managing Autoimmune Conditions: Immunosuppressive therapies may be used for autoimmune-related neuropathies.
- Medication Review: Your doctor may adjust or change medications that are causing neuropathy as a side effect.
Supportive Approaches for Nerve Pain Relief: Even when the underlying cause is managed, nerve pain can persist. Here, supportive therapies come into play.
- Physical Therapy: Custom exercises can improve muscle strength, coordination, and balance, reducing fall risk and improving mobility. Nerve gliding exercises can also be beneficial.
- Lifestyle Changes: A holistic approach to health can significantly impact neuropathy symptoms.
Here's a list of lifestyle changes to support nerve health:
- Strict Blood Glucose Control: If you have diabetes, keep your blood sugar levels consistently within target ranges.
- Limit Alcohol Consumption: Reduce or eliminate alcohol intake to prevent further nerve damage.
- Correct Vitamin Deficiencies: Ensure adequate intake of B vitamins (B1, B6, B12), vitamin E, and niacin. Consult your doctor before taking high doses of supplements, especially B6.
- Healthy, Balanced Diet: Focus on fruits, vegetables, whole grains, and lean proteins. Foods rich in omega-3 fatty acids and antioxidants are also beneficial.
- Regular Exercise: Engage in at least 30 minutes of moderate exercise most days of the week. Focus on balance exercises like Pilates, yoga, or Tai Chi if coordination is an issue. Exercise improves blood flow and nutrient delivery to nerves.
- Appropriate Footwear: Wear comfortable, well-fitting shoes with a wide toe box and good support. Avoid shoes with high midsole cushioning if you have impaired sensation, as they can be a trip hazard.
- Quit Smoking: Smoking constricts blood vessels, reducing blood flow to nerves.
- Maintain a Healthy Weight: Excess weight can put additional pressure on nerves.
Finding Topical Relief for Nerve Pain
While addressing the root cause and adopting healthy lifestyle changes are crucial, managing the daily discomfort of nerve pain is often a priority. This is where topical solutions can offer targeted relief.
Topical creams and patches deliver active ingredients directly to the affected area, providing localized relief with fewer systemic side effects compared to oral medications. For many of our customers in New York City and across the United States, finding comfort is key.
At Neuropasil, we've developed a nerve pain relief cream designed to provide soothing comfort. Our cream uses ingredients like menthol, which works by creating a cooling sensation that distracts from pain signals and provides temporary relief. When you apply a cream like ours, the active ingredients penetrate the skin to calm the nerve endings directly. This can be particularly helpful for the burning, tingling, and sharp pains often associated with neuropathy. We believe in providing relief that works with your body, not against it.
Our unique blend includes soothing ingredients like Aloe and Urea, which not only help with pain relief but also support skin health, a critical aspect for individuals with neuropathy who may experience dry or sensitive skin. Many loyal customers testify to using Neuropasil for neuropathy, sciatica, fibromyalgia, plantar fasciitis, strains, sprains, aches and pains, joint discomfort, back and neck pain, cramps and aching feet. Athletes also use Neuropasil to treat and recover from sore muscles.
You can learn about our natural ingredients and shop Neuropasil Nerve Pain Relief Cream for targeted relief.
Frequently Asked Questions about Peripheral Neuropathy
We often hear many questions about peripheral neuropathy, and we're happy to provide clear answers to help you better understand this condition.
How quickly can peripheral neuropathy develop?
The speed at which peripheral neuropathy develops varies significantly depending on what causes peripheral neuropathy.
- Instantaneous: Traumatic injuries, such as a severe accident or nerve compression, can cause neuropathy to develop immediately or within hours.
- Rapid Onset: Some toxic exposures (e.g., acute poisoning) or inflammation-based neuropathies (like Guillain-Barré Syndrome) can develop rapidly over days or weeks.
- Gradual Onset: Most other conditions, such as diabetic neuropathy, nutritional deficiencies, or medication-induced neuropathy, tend to develop slowly over months, years, or even decades. The symptoms might be subtle at first and gradually worsen.
Can peripheral neuropathy be reversed or cured?
The possibility of reversal or cure for peripheral neuropathy depends largely on its underlying cause and the extent of nerve damage.
- Reversible Causes: If the neuropathy is due to a treatable cause, such as a vitamin deficiency, medication side effect (where the medication can be stopped or adjusted), or well-controlled diabetes in its early stages, nerve function can sometimes improve or even recover. For instance, managing blood glucose levels in the early stages of diabetic neuropathy can sometimes halt its progression and even reverse some damage.
- Treating the Cause: The primary goal is always to identify and treat the underlying condition. If the nerve damage is severe or chronic, full reversal may not be possible.
- Symptom Management: In many cases, treatment focuses on managing symptoms, preventing further progression, and improving quality of life, even if a full cure isn't achievable.
Is peripheral neuropathy always painful?
No, peripheral neuropathy is not always painful. While pain (burning, sharp, shooting, or aching) is a very common and often debilitating symptom, it's not universally experienced by everyone with the condition. The specific symptoms depend on which types of peripheral nerves are affected:
- Sensory Nerve Damage: Can cause numbness, tingling, or a loss of sensation, rather than pain. You might not feel temperature changes, light touch, or even injuries.
- Motor Nerve Damage: Primarily leads to muscle weakness, cramps, or paralysis, which may not be inherently painful.
- Autonomic Nerve Damage: Affects involuntary bodily functions and can cause symptoms like dizziness, digestive issues, or abnormal sweating, typically without pain.
It's common for individuals to experience a combination of these symptoms, and the severity can range from mild to severe. If you're experiencing any unusual sensations or changes in your body, it's always best to consult a healthcare professional for an accurate diagnosis.
References
- About 2.4% of people globally have a form of peripheral neuropathy. Among people 45 and older, that percentage rises to between 5% and 7%. Source: Neuropathy - StatPearls - NCBI Bookshelf
- Up to one-half of people with diabetes have peripheral neuropathy. Source: Peripheral Neuropathy | NIDDK
- It is estimated that as many as 66% of individuals with chronic alcohol abuse may suffer from alcoholic polyneuropathy. Source: Common causes of peripheral neuropathy | The Foundation for Peripheral Neuropathy
- Uremic neuropathy can affect 60% to 100% of people with chronic kidney disease. Source: Uremic Polyneuropathy - Kidney International
- An estimated one to four million people in America have Sjögren’s syndrome, a potential cause of neuropathy. Source: Sjögren's Foundation FAQs
- Mutations in more than 100 genes have been identified as a cause of Charcot-Marie-Tooth disease. Source: Inherited Neuropathies | The Foundation for Peripheral Neuropathy
- Information on chronic pain and depression: Source: Depression | National Institute of Mental Health (NIMH)
- More on Vitamin B12's role in nerve health: Source: Vitamin B12 Fact Sheet for Consumers | NIH Office of Dietary Supplements
- Peripheral neuropathy: Symptoms and causes: Source: Peripheral neuropathy - Symptoms and causes - Mayo Clinic













