Understanding Heel Pain When Walking: What Your Body Is Telling You
Heel pain when walking is a common foot complaint that can turn every step into a challenge. Affecting roughly 1 in 10 people in their lifetime, it's a widespread issue with clear causes and effective solutions.
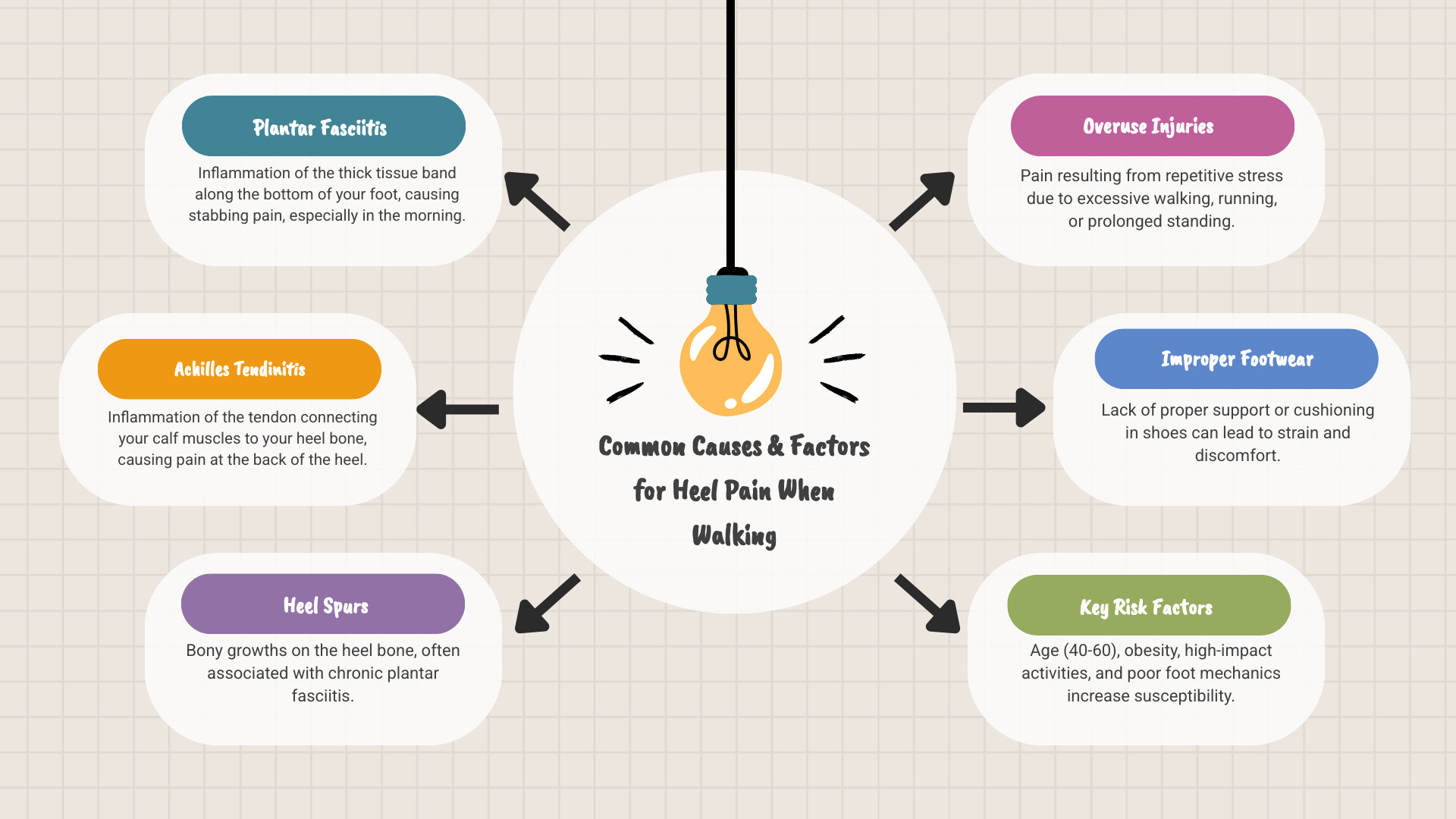
Most Common Causes:
- Plantar fasciitis: Inflammation of the tissue on your foot's bottom.
- Achilles tendinitis: Inflammation of the tendon connecting your calf to your heel.
- Heel spurs: Bony growths on the heel bone.
- Overuse injuries: From repetitive walking, running, or standing.
- Improper footwear: Shoes lacking proper support or cushioning.
Quick Relief Options:
- Rest and reduce activities that worsen pain.
- Apply ice for 10-15 minutes twice daily.
- Wear supportive shoes with good arch support.
- Use topical pain relief creams for targeted comfort.
- Perform gentle calf and foot stretches.
When to See a Doctor: If pain persists beyond 2-3 weeks, is severe, or prevents you from walking normally.
The good news is that over 90% of cases improve with conservative treatment. The heel is your foot's largest bone, cushioned by a fatty pad and supported by the plantar fascia. When this system is overworked or injured, pain develops, often feeling sharpest during those first morning steps.
Common culprits include obesity, ill-fitting shoes, running on hard surfaces, and age, with most cases occurring in people between 40 and 60. I'm Tony Enrico, and through my work with Neuropasil, I've helped many individuals find relief. Our advanced nerve pain relief cream uses natural ingredients for fast-acting comfort, helping you return to pain-free movement. Let's explore what's causing your heel pain and how to address it.
Why Does My Heel Hurt? Unpacking the Common Causes
When heel pain when walking strikes, it helps to understand what's happening inside your foot. The heel bone (calcaneus) is your body's primary shock absorber, cushioned by a fat pad. The plantar fascia, a tough tissue band, supports your arch, while the Achilles tendon connects your calf muscles to the heel for push-off power. When any part of this system is overworked or injured, pain occurs.
The two most common culprits have distinct symptoms:
| Condition | Primary Location of Pain | Characteristic Pain Pattern | Other Symptoms |
|---|---|---|---|
| Plantar Fasciitis | Bottom of the heel, near the arch | Sharp, stabbing pain, especially with first steps in the morning or after rest; lessens with movement but may return after prolonged activity | Stiffness, tenderness, may feel like a stone bruise |
| Achilles Tendinitis | Back of the heel, above the heel bone | Aching or burning pain, often worse with activity (especially running or jumping); stiffness in the morning | Tenderness, swelling, limited ankle flexibility |
Understanding Plantar Fasciitis and Heel Spurs
If you feel a sharp, stabbing pain in your heel with your first steps in the morning, you've likely met plantar fasciitis. Affecting about 2 million Americans annually, it's the most common cause of heel pain. It occurs when the plantar fascia becomes inflamed from repetitive stress, leading to tiny tears in the tissue. Activities like long-distance running or standing on hard surfaces all day are common triggers.
Many people confuse this with heel spurs, which are bony growths that can form on the heel bone due to long-term tension. However, the spur itself is rarely the source of pain. The real issue is the inflamed plantar fascia. Most people with heel spurs have no pain at all.
For a deeper understanding, see more info about Plantar Fasciitis or the Plantar Fasciitis overview from Mayo Clinic.
Other Conditions That Cause Heel Pain
While plantar fasciitis is common, other conditions can also cause heel pain when walking:
- Achilles Tendinitis: Inflammation of the large tendon at the back of the ankle, causing pain during or after exercise.
- Bursitis: Inflammation of the small, fluid-filled sacs (bursae) that cushion the heel, resulting in pain, swelling, and redness.
- Stress Fractures: Tiny cracks in the heel bone from repetitive force, with pain that worsens with activity and improves with rest.
- Tarsal Tunnel Syndrome: Compression of the tibial nerve in the ankle, causing burning, tingling, or numbness in the heel.
- Sever's Disease: A common cause of heel pain in active children (ages 8-14), caused by stress on the heel's growth plate.
- Arthritis: Various forms, including osteoarthritis and rheumatoid arthritis, can affect foot joints and lead to heel pain.
- Nerve Entrapment: Compression or irritation of nerves in the foot, creating pain, tingling, or numbness.
- Heel Contusion (Stone Bruise): A bruise on the fatty pad of the heel from landing forcefully or stepping on a hard object.
Understanding the cause is the first step toward relief. For more information, explore more info on general heel pain.
Are You at Risk? Identifying Factors and Getting a Diagnosis
If you're dealing with heel pain when walking, you might wonder, "Why me?" Certain risk factors can make you more vulnerable. Knowing these can help with prevention, while understanding the diagnostic process can ease anxiety about seeking help.
Key Risk Factors for Developing Heel Pain
Several factors can increase stress on your heels:
- Age: Those between 40 and 60 are most susceptible as tissues lose elasticity.
- Activity Level: High-impact activities like running or dancing, especially on hard surfaces, put repetitive stress on the heel.
- Foot Mechanics: Both flat feet and high arches can alter weight distribution and strain the plantar fascia.
- Excess Weight: Being overweight increases the load on your heels with every step.
- Occupation: Jobs that require long hours of standing, such as nursing or factory work, contribute to chronic heel stress.
- Improper Footwear: Worn-out shoes, footwear with poor arch support, or walking barefoot on hard surfaces can all lead to pain.
How Doctors Diagnose Heel Pain
If heel pain when walking lasts more than a few weeks, it's time to see a doctor. The diagnosis is usually straightforward.
- Medical History: Your doctor will ask about your pain, activity levels, and footwear to gather clues about the cause.
- Physical Examination: The doctor will examine your foot for tenderness, swelling, or redness. Pressing on specific areas of the heel can help pinpoint the problem, such as plantar fasciitis. They will also observe your gait to identify any biomechanical issues.
- Imaging Tests: X-rays are often used to rule out stress fractures, bone spurs, or arthritis. While X-rays can show heel spurs, remember they are rarely the actual source of pain. Advanced imaging like an MRI or ultrasound is typically only used if the diagnosis is unclear or initial treatments fail.
An accurate diagnosis is key, as treatment varies depending on the cause. If home care doesn't help within a few weeks, it's important to understand when to see a doctor for heel pain.
Finding Relief: Effective Approaches for Heel Pain When Walking
If you have heel pain when walking, take heart: this condition is highly treatable. Over 90% of people with plantar fasciitis find relief within 10 months using simple, conservative methods. The focus is on non-invasive care that addresses both symptoms and underlying causes to create lasting relief.
Think of healing as a partnership with your body. You provide the right conditions, and your body does the work. For more tips, you can find helpful information on Managing Plantar Fasciitis and Bone Spurs.
Supportive Strategies and Therapies
Managing heel pain when walking effectively involves combining several strategies:
- Gentle Stretching: Regularly stretching your calf muscles and plantar fascia reduces tension and improves flexibility.
- Topical Pain Relief: Creams like Neuropasil offer targeted, fast-acting comfort. Our formula with natural ingredients like Aloe, Urea, and Menthol provides soothing relief directly to the affected area, helping you stay active.
- Supportive Insoles: Over-the-counter or custom orthotics provide arch support and cushioning, distributing pressure more evenly across your foot.
- Rest and Activity Modification: Temporarily reducing high-impact activities gives your foot a chance to heal. Swap running for low-impact exercises like swimming or cycling.
- Medical Advice: If pain persists after a few weeks, consult a healthcare professional. They may recommend physical therapy or other treatments. Surgery is rarely needed.
How Footwear Impacts Heel Pain When Walking
Your shoes are a therapeutic tool. For anyone with heel pain when walking, the right footwear is non-negotiable.
- Prioritize Arch Support: Good arch support is crucial for distributing pressure and preventing strain on the plantar fascia.
- Choose Cushioned Soles: Look for shoes with thick, shock-absorbent soles to protect your heel from impact.
- Look for Deep Heel Cups: This feature helps stabilize the heel and provides extra cushioning.
- Avoid Walking Barefoot: On hard surfaces like concrete or hardwood, walking barefoot offers no support and increases stress on your heel.
- Replace Worn-Out Shoes: The support in shoes breaks down over time. Replace athletic shoes every 6-9 months or after 250-500 miles of use to prevent recurring pain.
For a detailed guide on choosing the right shoes, see our Guide to Plantar Fasciitis Shoes.
Your At-Home Toolkit for Heel Pain Management

When heel pain when walking flares up, you can take control with effective at-home strategies. A powerful first step is the R.I.C.E. method: Rest, Ice, Compression, and Elevation. This approach helps manage acute pain and swelling.
Beneficial Exercises and Stretches for Heel Pain
Regular, gentle stretching is one of the most effective ways to relieve heel pain when walking. By improving flexibility in your calf and plantar fascia, you release the tension that pulls on your heel.
- Calf Stretches: Stand facing a wall and step one foot back, keeping the heel on the ground. Lean forward until you feel a stretch in your calf. Hold for 30 seconds and switch sides.
- Towel Stretch: While seated, loop a towel around the ball of your foot and gently pull it toward you, keeping your knee straight. Hold for 30 seconds.
- Rolling Exercises: Roll your foot over a frozen water bottle or tennis ball for 5-10 minutes. This massages the plantar fascia and reduces inflammation.
- Toe Curls: Place a small towel on the floor and use your toes to scrunch it toward you. This strengthens the small muscles that support your arch.
Consistency is more important than intensity. For more movements, visit our guide on Exercises for Plantar Fasciitis.
Simple Home Remedies to Ease Heel Pain When Walking
Beyond stretching, several home remedies can provide relief.
- Ice Therapy: Apply an ice pack wrapped in a towel to your heel for 10-15 minutes, twice daily, to reduce swelling and numb pain.
- Anti-Inflammatory Medication: Over-the-counter anti-inflammatory medications (NSAIDs) can help manage pain and inflammation. Use them as directed and consult a doctor for long-term use.
- Taping: Strapping your foot with athletic tape can provide temporary arch support and reduce stress on the plantar fascia.
- Gentle Foot Massage: Massaging the arch and heel improves circulation and relaxes tight tissues.
- Topical Pain Relief Creams: Products like Neuropasil offer a significant advantage by delivering relief directly to the source of pain. Our cream, with soothing ingredients like Aloe, Urea, and Menthol, works locally for fast-acting comfort without systemic side effects. It's an ideal addition to your daily routine, especially on active days.
For more on choosing topical solutions, explore our guide on Foot Pain Relief Creams.
Navigating Your Recovery and Seeking Help
The path to overcoming heel pain when walking requires time and dedication, but the outlook is positive. Over 90% of patients improve significantly within 10 months using conservative, nonsurgical methods. However, it's crucial to know when home care isn't enough and professional help is needed.
Recovery timelines vary, but consistency is the key to success. Sporadic efforts rarely yield lasting results.
When to See a Doctor
While self-care is powerful, certain signs indicate it's time to see a healthcare provider:
- Pain persists for more than 2-3 weeks despite home treatment.
- Pain is severe and prevents you from bearing weight or walking normally.
- You experience numbness, tingling, or burning sensations, which could signal nerve involvement.
- There are signs of infection, such as redness, warmth, significant swelling, or fever.
- You have diabetes, as any foot pain warrants a doctor's evaluation to prevent complications. Learn more about diabetic foot pain.
The Outlook for Heel Pain
The prognosis for most cases of heel pain when walking is excellent. The difference between a smooth recovery and a prolonged struggle often comes down to consistency. Daily stretching, wearing supportive shoes, and using topical relief like Neuropasil are commitments to your healing.
Early and consistent management is also crucial for preventing chronic pain. Ignoring discomfort can alter your gait, leading to compensatory issues in your knees, hips, and back. By addressing the problem head-on, you avoid this cascade effect.
Lifestyle changes act as an insurance policy against future episodes. Maintaining a healthy weight, choosing appropriate footwear, and incorporating regular stretching will keep your feet resilient. With the right approach, heel pain when walking can be a temporary setback, not a permanent limitation.
Conclusion
You now have a clearer understanding of heel pain when walking, from its causes like plantar fasciitis and Achilles tendinitis to its risk factors and diagnosis. The most important takeaway is that relief is achievable—more than 90% of people improve with consistent, conservative care.
The path forward is built on a few key practices. Proper footwear with good arch support and cushioning is foundational. Regular, gentle stretching of your calves and plantar fascia reduces tension and prevents flare-ups. When pain strikes, having effective tools is essential. Modifying activities, applying ice, and using topical pain relief creams like Neuropasil provide targeted, fast-acting comfort.
Our natural formula with Aloe, Urea, and Menthol delivers soothing relief right where it hurts, helping you regain confidence in every step. Your feet carry you through life, and they deserve your care. By taking these practical steps, you are empowering yourself to move freely and live fully. For more information on effective solutions, we invite you to explore The Complete Guide to Effective Foot Pain Creams.
Here's to pain-free movement and stepping forward with confidence.
References
Throughout this comprehensive guide on heel pain when walking, we've drawn on information from leading medical institutions and health organizations to ensure accuracy and reliability. Understanding heel pain requires evidence-based knowledge, and we're grateful to these trusted sources for their contributions to patient education.
The American Academy of Orthopaedic Surgeons (AAOS) provides detailed information on Plantar Fasciitis and Bone Spurs, helping us understand the mechanics of heel pain at http://orthoinfo.aaos.org/topic.cfm?topic=a00159. Similarly, the American Podiatric Medical Association (APMA) offers valuable insights on Heel Pain at http://www.apma.org/learn/FootHealth.cfm?ItemNumber=985, contributing to our understanding of foot health fundamentals.
The Cleveland Clinic has been an invaluable resource, with their comprehensive guides on both Heel Pain: Causes, Diagnosis & Treatment at https://my.clevelandclinic.org/health/symptoms/heel-pain and their specific article on Plantar Fasciitis at https://my.clevelandclinic.org/health/diseases/14709-plantar-fasciitis. These resources helped us provide accurate information on diagnosis and treatment approaches.
Mayo Clinic's authoritative piece on Plantar fasciitis - Symptoms and causes at https://www.mayoclinic.org/diseases-conditions/plantar-fasciitis/symptoms-causes/syc-20354846 provided essential context for understanding this common condition. Healthline's article on Heel Pain: Causes, Treatments, and Prevention at https://www.healthline.com/health/heel-pain offered practical insights into managing discomfort.
For our UK readers, the NHS guide on Heel pain at https://www.nhs.uk/conditions/foot-pain/heel-pain/ and The Royal College of Podiatry's information on Heel Pain at https://rcpod.org.uk/common-foot-problems/heel-pain provided additional perspectives on self-care approaches.
The Victoria State Government health resources at https://www.health.vic.gov.au/ contributed to our understanding of foot anatomy and common causes of heel pain. eMedicineHealth's article How to Alleviate Heel Pain When Walking: Expert Tips at https://www.emedicinehealth.com/howcanirelievethepaininmyheel/article_em.htm and The Podiatry Group's expert insights at https://www.thepodiatrygroup.com/2025/03/14/how-to-alleviate-heel-pain-when-walking-expert-tips/ offered practical guidance for managing symptoms.
We're committed to providing you with accurate, trustworthy information backed by medical expertise, so you can make informed decisions about managing your heel pain when walking and returning to the activities you love.














