Understanding Post-Op Nerve Pain: The Unexpected Challenge After Surgery
Post-op nerve pain affects a surprising number of people after surgery. Here's what you need to know:
Key Facts About Post-Surgical Nerve Pain:
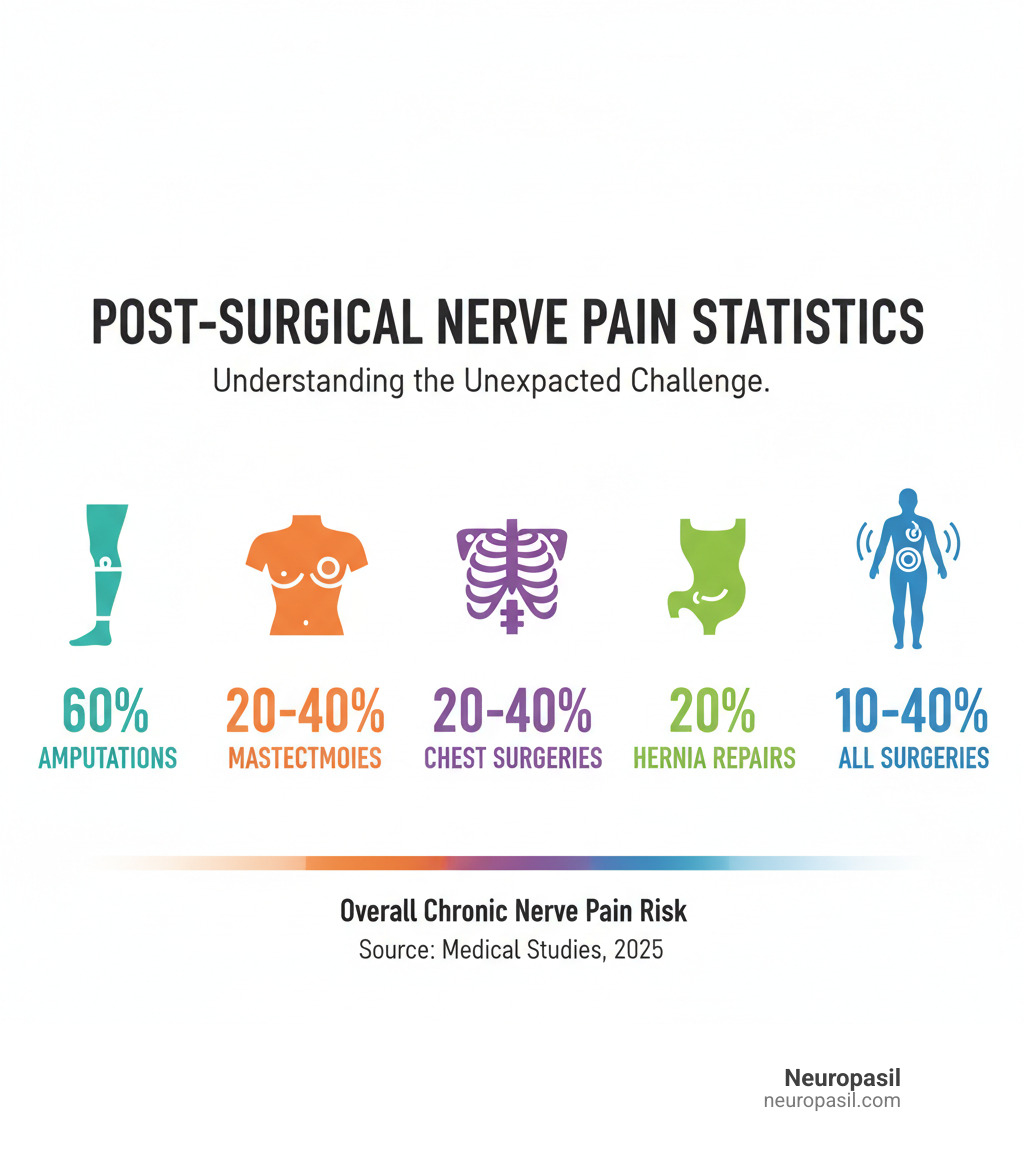
- Affects 10-40% of patients after common surgeries
- Can develop immediately or months later
- Ranges from mild tingling to severe, chronic pain
- Most common after: mastectomy (20-40%), thoracotomy (20-40%), hernia repair (20%), and amputation (60%)
- Symptoms include: burning, shooting pain, numbness, and hypersensitivity
After surgery, you expect to feel better, but sometimes a new, strange pain appears. This burning, tingling, or electric shock sensation is likely nerve pain, and it's a common issue.
Post-op nerve pain happens when surgical procedures damage or irritate nerves. Unlike typical surgical pain that gets better with time, nerve pain can persist for months or even years. Understanding the cause is the first step toward finding relief.
Most operations require cutting through skin nerves. While this usually causes temporary discomfort, it can sometimes trigger changes in your nervous system that turn acute pain into a chronic condition.
Recognizing nerve pain early and taking action is key. With the right approach, many people find significant relief and get back to their active lives.
Understanding Post-Surgical Nerve Pain (SNPP)
You trusted your surgeon, but now you're dealing with a new kind of discomfort. Post-op nerve pain isn't typical soreness; it's a different and often surprising challenge.
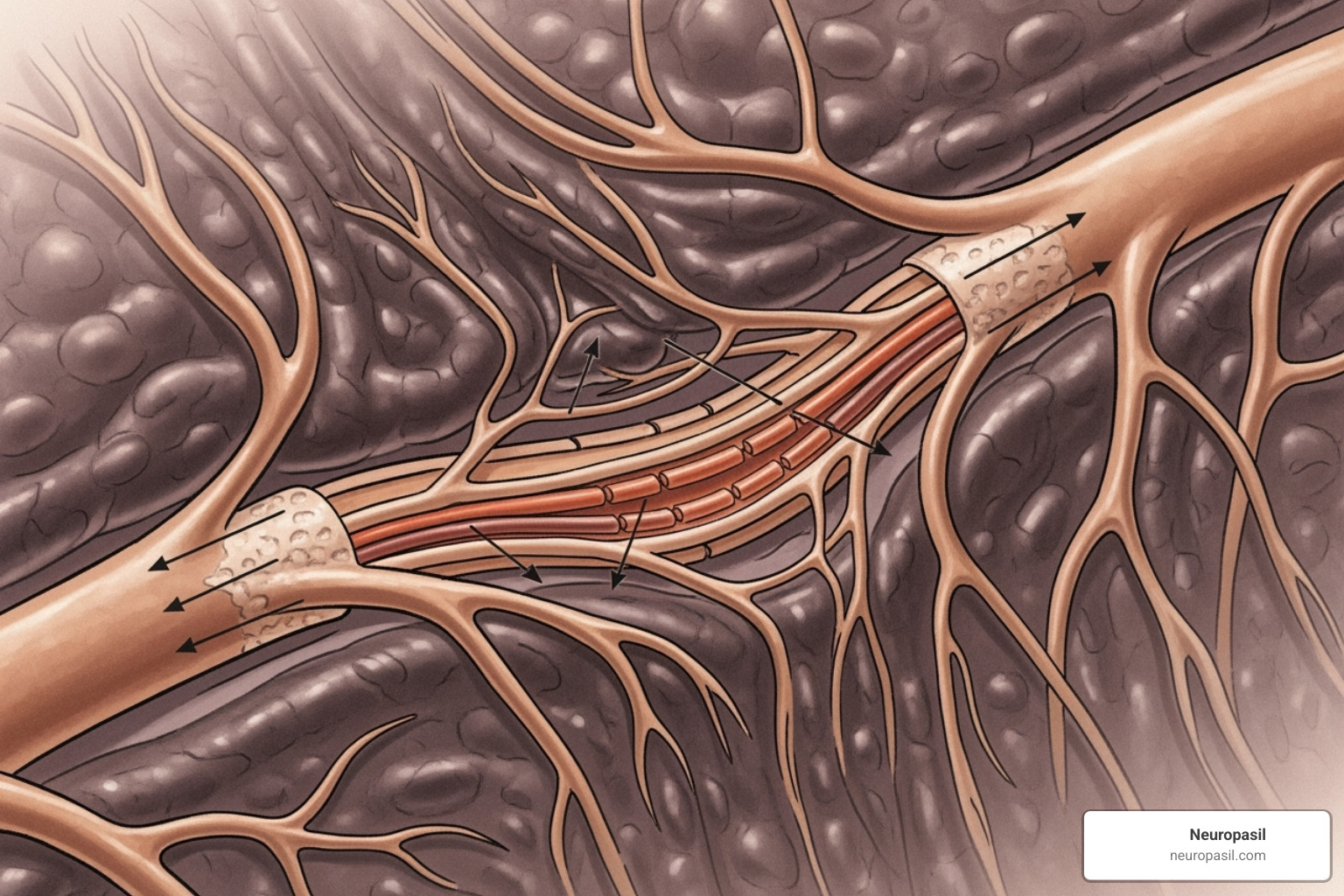
During surgery, surgeons cut through tissue, including the delicate network of nerves. Your nervous system is like an electrical grid, with the brain and spinal cord (the central nervous system) as the control center and peripheral nerves branching out like power lines. Surgery can disrupt these pathways, even with the most skilled surgeon.
What makes post-op nerve pain challenging is that the nervous system can "learn" to be in pain, creating a difficult cycle. The journey from a surgical cut to chronic nerve pain involves complex changes, which you can learn more about in scientific research on the perioperative process of SNPP.
What is SNPP and What Causes It?
Surgically-Induced Neuropathic Pain (SNPP) is chronic pain from nerve damage or dysfunction after surgery. It's not typical healing pain; it comes directly from injured nerves.
The causes often combine. Direct nerve injury can happen if nerves are cut (transection), torn (laceration), stretched, or compressed by instruments, stitches, or swelling.
Scar tissue formation is another factor. While natural, excessive scar tissue can wrap around and squeeze nerves, causing ongoing irritation.
Inflammation also plays a key role. Surgery triggers an immune response, causing swelling and chemical changes that can irritate nearby nerves. If this inflammation persists, it keeps nerves in a state of agitation.
Common Signs and Symptoms of Post-op Nerve Pain
How do you know if your pain is normal or something more? Post-op nerve pain has telltale signs.
A burning sensation is a common clue, often described as the skin being on fire. Tingling or "pins and needles" is another red flag, like a limb constantly falling asleep.
Oddly, numbness can accompany pain, with some spots feeling dead to the touch while others are hypersensitive. Sharp, shooting, or electric shock-like pain can be sudden and intense, often radiating along the nerve's path.
Two frustrating symptoms are allodynia and hyperalgesia. With allodynia, a light touch (like clothing) causes pain. With hyperalgesia, a normally painful stimulus becomes excruciating. These symptoms are usually near the surgery site but can also cause weakness or balance issues.
How Acute Nerve Injury Becomes Chronic Pain
When nerves are injured, your body's alarm system activates. This acute pain is protective. But sometimes, the alarm gets stuck on, becoming more sensitive even after the tissue has healed.
Two processes drive this change to chronic post-op nerve pain.
Peripheral sensitization occurs at the injury site. Damaged nerves become trigger-happy, firing pain signals with little provocation, like a car alarm that goes off too easily. Inflammation makes these nerves even more excitable.
Central sensitization is more complex. Constant pain signals cause the spinal cord and brain to change how they process information. Neurons become hypersensitive, amplifying minor signals into major pain messages. This can lead to "brain reorganization," where the brain rewires itself around the pain. It's a maladaptive response where your nervous system learns to be in pain.
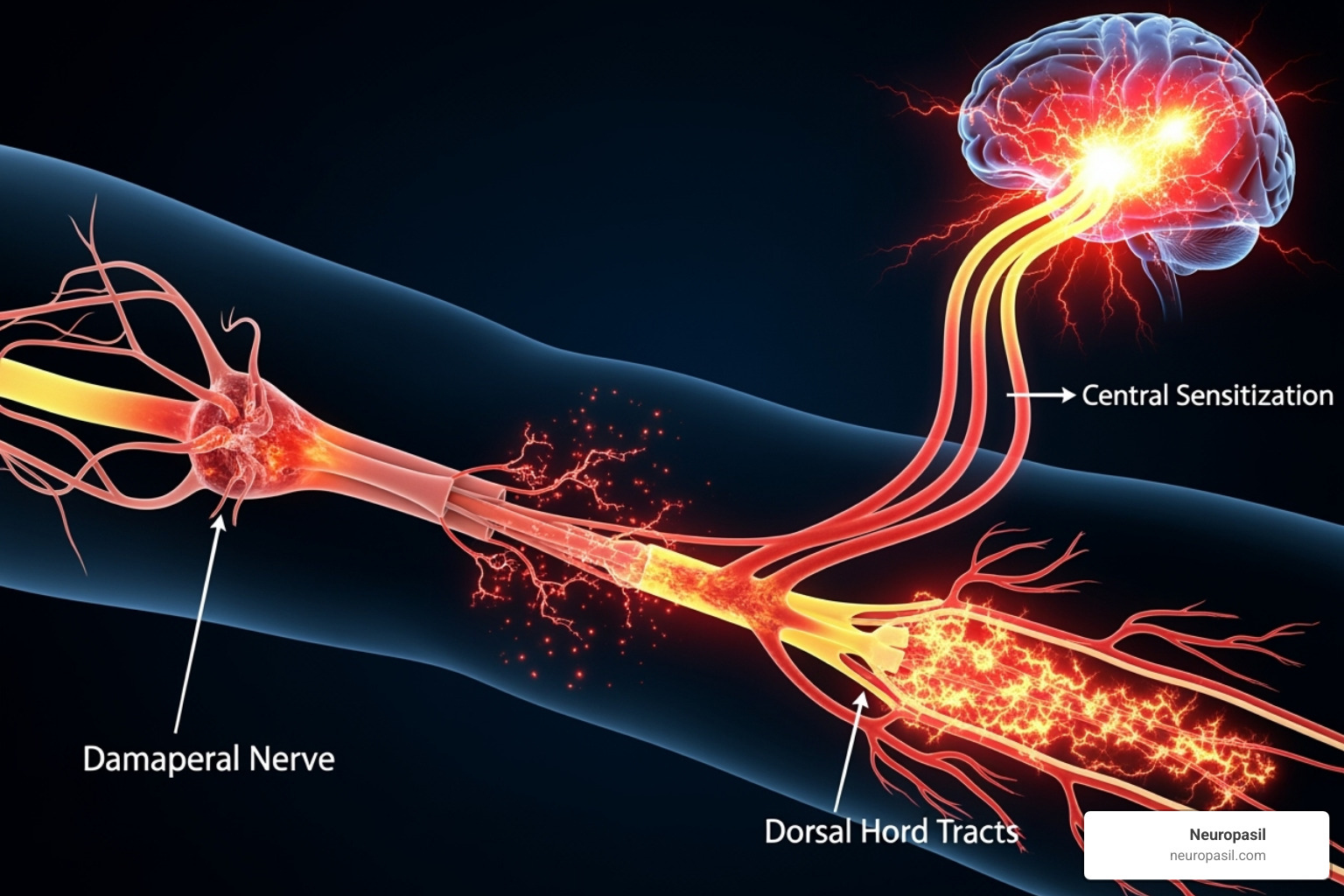
These nervous system changes can become self-perpetuating. Even after the surgical site has healed, your nervous system continues to generate pain signals. This is why early intervention is so important—to interrupt this process before these changes become permanent.
Are You at Risk? Diagnosis and Key Factors
Understanding your risk for post-op nerve pain can help you and your doctor be prepared. While you can't control everything, early detection is key.

Factors That Increase Your Risk
Some people are more likely to develop post-op nerve pain. Knowing these risk factors helps in monitoring for warning signs.
- Type of surgery: Operations near major nerve pathways carry higher risks. Limb amputation has the highest risk (around 60%), followed by mastectomy and chest surgeries (20-40%) and hernia repairs (about 20%). Even minor incisions can affect small skin nerves.
- Pain history: If you had chronic pain before surgery, your nervous system might already be more sensitive.
- Genetics: Some people are genetically more prone to developing chronic pain after an injury.
- Psychological factors: High levels of stress, anxiety, or a tendency to catastrophize about pain can increase your risk. Your mental state is closely linked to your pain experience.
- Severity of acute pain: Intense, poorly controlled pain immediately after surgery can be a warning sign for chronic issues.
How Doctors Diagnose Nerve Pain After Surgery
Diagnosing post-op nerve pain requires a thorough evaluation, as symptoms can mimic other issues.
- Patient history: Your story is the starting point. Describing when the pain started, what it feels like (burning, shooting, tingling), and what makes it better or worse provides crucial clues.
- Physical exam: Your doctor will examine the area, testing for sensation (light touch, temperature), muscle strength, and reflexes to map out affected areas.
- Specialized sensory testing: Using different textures or temperatures can reveal how your nerves are responding, identifying areas that are numb, hypersensitive, or reacting incorrectly.
- Pain questionnaires: These diagnostic tools help measure the specific qualities of nerve pain and track your progress over time.
- Advanced imaging: MR neurography, a special MRI, can directly visualize nerves to find damage or compression. High-frequency ultrasound is also useful for examining nerves closer to the skin.
- Electrical tests: EMG and nerve conduction studies measure how well electrical signals travel through your nerves, showing if there's damage.
Getting an accurate diagnosis is the first step toward creating an effective treatment plan for your post-op nerve pain.
A Comprehensive Guide to Managing Post-op Nerve Pain
Dealing with post-op nerve pain can feel overwhelming, but many options are available. Effective management involves a multimodal approach, combining different strategies for the best chance at relief and an improved quality of life. Research supports this comprehensive strategy, as detailed in this scientific research on pain management.
Let's explore the tools available to manage your post-op nerve pain.
The Role of Physical and Occupational Therapy
Physical and occupational therapy are powerful tools for regaining control over your body. They do more than just prescribe exercises.
- Desensitization techniques help retrain your nervous system if you have allodynia (pain from light touch). A therapist guides you through gentle exposure to different textures, helping your brain re-classify these sensations as harmless.
- Range of motion exercises keep joints flexible and prevent stiffness that can develop from protecting a painful area.
- Strengthening exercises rebuild muscles that may have weakened from disuse, providing better support to the affected area.
- Occupational therapists help you adapt daily activities to perform them with less pain, sometimes suggesting assistive devices.
- Graded motor imagery is a technique that uses your brain's plasticity to aid healing. It progresses from imagining movement to mirror therapy, helping your brain reorganize its perception of the painful area.
Topical Approaches for Post-op Nerve Pain
Topical treatments deliver relief directly to the painful area, often with fewer side effects than oral medications.
- Topical numbing agents, available as gels or patches, can block pain signals at the source.
- Anti-inflammatory gels can reduce inflammation around irritated nerves, providing significant relief, especially in the early stages.
- Other specialized creams work by affecting the chemical messengers that transmit pain signals from the nerves.
- Compounded creams can be custom-formulated by a pharmacy to combine several ingredients to meet your specific needs.
Neuropasil offers topical solutions designed to address nerve discomfort. Discuss with your healthcare provider if our products might be a good fit for your pain management strategy. These formulations can provide comfort and work well alongside other treatments.
Simple comfort measures like keeping skin moisturized and wearing soft fabrics can also make a real difference, especially when dealing with hypersensitivity.
Mind-Body and Lifestyle Approaches
Your mind and body are deeply connected, especially with post-op nerve pain. Stress and lifestyle can influence your pain experience.
- Cognitive Behavioral Therapy (CBT) helps you change how you respond to pain by identifying unhelpful thoughts and developing better coping strategies.
- Meditation and deep breathing exercises can calm your nervous system and reduce pain perception. Techniques like diaphragmatic breathing activate your body's natural relaxation response.
- An anti-inflammatory diet rich in fruits, vegetables, and healthy fats can help reduce systemic inflammation that contributes to nerve irritation.
- Gentle exercise like walking or swimming improves circulation and releases natural pain relievers (endorphins). Always start slowly and consult your doctor or physical therapist.
- Good sleep hygiene is crucial, as poor sleep can worsen pain. A consistent schedule and a relaxing bedtime routine can help break the cycle of pain and sleeplessness.
- Stress reduction is essential. Finding ways to manage stress through yoga, hobbies, or relaxation techniques can significantly impact your pain levels.
The Path to Recovery: Early Intervention and Future Outlook
Recovering from post-op nerve pain is an active process. The choices made in the first few weeks and months after surgery can dramatically affect your long-term outcome. Early intervention is your best defense against pain becoming a chronic issue.
Why Early Intervention is Crucial
The window for preventing chronic post-op nerve pain is smaller than most people realize. The first few months are critical.
Preventing the transition to chronic pain is like stopping a snowball from rolling down a hill. What starts as acute discomfort can grow into a much larger problem if not addressed quickly. When pain signals fire repeatedly, your central nervous system can "learn" to be in pain through a process called central sensitization.
Early, comprehensive treatment can interrupt this process. Studies show that patients who receive prompt care for post-op nerve pain have better outcomes, including less pain and a faster return to normal activities. Acting quickly can be the difference between a full recovery and years of chronic pain.
When to See a Pain Management Specialist
Knowing when to seek specialized help for post-op nerve pain is important. Here are some signs it's time to see a specialist:
- Pain lasting over 3 months: At this point, the pain is considered chronic.
- Pain isn't responding to initial treatments: If basic approaches aren't working, it's time for more specialized expertise.
- Pain significantly impacts your daily life: If pain affects your sleep, work, or mental health, seek help immediately.
- Worsening symptoms: If burning, numbness, or shooting pains are increasing, it suggests ongoing nerve irritation that needs evaluation.
- New numbness or weakness: These symptoms could indicate progressive nerve damage and require immediate attention.
Pain management specialists have a broader toolkit for diagnosing and treating neuropathic pain.
New Research and Future Directions
The field of post-op nerve pain treatment is advancing rapidly, offering real hope.
- Functional neuroimaging (fMRI) allows us to see pain in the brain, leading to more targeted treatments.
- Genetic research is identifying markers for pain susceptibility, which may soon allow for personalized prevention strategies.
- Novel drug targets are being developed to work specifically on neuropathic pain pathways.
- Neuromodulation technology, like spinal cord stimulators, is becoming smaller and more effective at providing targeted relief.
- Objective measures for pain are being developed to provide a more accurate diagnosis and assessment of treatment effectiveness.
For those interested in the latest breakthroughs, resources like advances in clinical research from Mass General offer valuable insights. The future of treatment is moving toward more personalized and precise therapies.
Frequently Asked Questions about Post-Surgical Nerve Pain
You're not alone in wondering about post-op nerve pain - we hear these questions every day from patients who are trying to understand what's happening to their bodies. Let's address the most common concerns with straightforward, honest answers.
How long does nerve pain last after surgery?
This is probably the first question on your mind, and unfortunately, there's no simple one-size-fits-all answer. The timeline for post-op nerve pain varies dramatically from person to person.
For many people, nerve pain gradually fades as healing progresses. Nerves are notoriously slow healers - they regenerate at roughly 1 millimeter per day. That means if a nerve needs to heal over several centimeters, you're looking at weeks or even months for complete recovery.
The good news is that most acute nerve pain does resolve on its own within a few weeks to several months. Your body has remarkable healing abilities, and given time, many nerve irritations settle down naturally.
However, we need to be honest about the other possibility. For some patients, post-op nerve pain becomes a chronic condition, persisting for more than three months or even years. This happens when the nervous system undergoes those changes we discussed earlier - central sensitization - where your pain pathways essentially get "stuck" in an overactive state.
The importance of treatment cannot be overstated here. Early intervention significantly improves your chances of preventing acute pain from becoming chronic. While potential for permanency exists in severe cases, proper medical care dramatically reduces this risk and helps most people find meaningful relief.
Can post-op nerve pain be prevented?
This is such an important question, and the answer gives us real hope. While we can't prevent post-op nerve pain entirely - surgery inherently involves some risk to nerves - modern medicine has developed several powerful strategies to dramatically reduce your risk.
- Preventive analgesia: Giving pain medication before, during, and immediately after surgery can shield the nervous system and prevent it from becoming hypersensitive.
- Careful surgical technique: Experienced surgeons use precise methods to minimize nerve damage during procedures.
- Regional anesthesia: Nerve blocks or epidurals can provide superior pain control by numbing specific areas, reducing the pain signals that can trigger chronic issues.
- Pre-operative risk assessment: Identifying patients at higher risk allows medical teams to implement more aggressive preventive strategies.
- Managing acute pain effectively: Poorly controlled pain right after surgery is a strong predictor of chronic pain development. That's why your medical team takes your post-surgical pain so seriously.
Is it normal to have shooting pains after surgery?
Yes, shooting pains can be a common symptom after surgery, and this often catches patients off guard. These sharp, electric-like sensations typically indicate nerve irritation or regeneration - essentially, your nerves are "waking up" and sometimes send mixed signals as they heal.
Think of it like static on a radio as it searches for the right frequency. As your nerves repair themselves, they can misfire occasionally, creating those startling shooting sensations. In many cases, this is actually a sign that healing is happening, even though it's uncomfortable.
However, you need to know when to be concerned. Shooting pains warrant medical attention if they're getting worse over time, becoming unbearably intense, or if you're developing new numbness or weakness. These could signal ongoing nerve damage that needs immediate treatment.
The key is differentiating from normal healing. Normal post-surgical shooting pains tend to gradually decrease in frequency and intensity over weeks. They might be triggered by movement or touch initially but should become less bothersome as healing progresses.
If your shooting pains are disrupting your sleep, preventing you from moving normally, or persisting without any improvement after several weeks, don't hesitate to reach out to your healthcare provider. They can assess whether what you're experiencing falls within the normal range or requires specific treatment for post-op nerve pain.
You know your body best. If something feels wrong or concerning, it's always better to ask questions and get reassurance than to suffer in silence.
Take Control of Your Recovery Journey
You've made it through surgery, but now you're facing something you didn't expect: post-op nerve pain. If you're reading this, you're already taking an important first step - learning about what's happening to your body and what you can do about it.
Throughout this guide, we've walked through the complex world of nerve pain after surgery. We've seen how surgical trauma can damage delicate nerves, leading to that burning, tingling, or shooting pain that feels so different from regular surgical discomfort. We've explored who's most at risk and how doctors figure out what's really going on when your pain doesn't follow the usual healing timeline.
The good news? You have options. From physical therapy that helps retrain your nervous system to topical treatments that target pain right where you feel it, there's a whole toolkit available. Mind-body approaches like meditation and gentle exercise can calm your overactive pain signals, while emerging treatments offer hope for even better solutions in the future.
Here's what we want you to remember most: early intervention makes all the difference. That persistent burning sensation or those electric shock pains aren't something you need to "tough out." The sooner you address nerve pain, the better your chances of preventing it from becoming a long-term companion.
Your recovery journey should be personalized to you. What works for your neighbor might not be your best solution. That's why a multidisciplinary care team - including your surgeon, primary doctor, physical therapist, and possibly a pain specialist - can be so valuable. They can help create a treatment plan that addresses your specific symptoms, lifestyle, and goals.
Neuropasil as a topical option to discuss with your doctor can be one piece of your comprehensive pain management strategy. Combined with other treatments, topical solutions may help provide the comfort and relief you're seeking as you work toward recovery.
You don't have to steer this alone. Whether you're dealing with post-surgical tingling that's lasted longer than expected or severe nerve pain that's disrupting your life, professional help is available. Taking charge of your recovery means asking questions, advocating for yourself, and seeking the care you deserve.
Your surgery was meant to improve your life. Don't let nerve pain steal that promise from you.













