Understanding the Sharp Reality of Acute Sciatic Nerve Pain
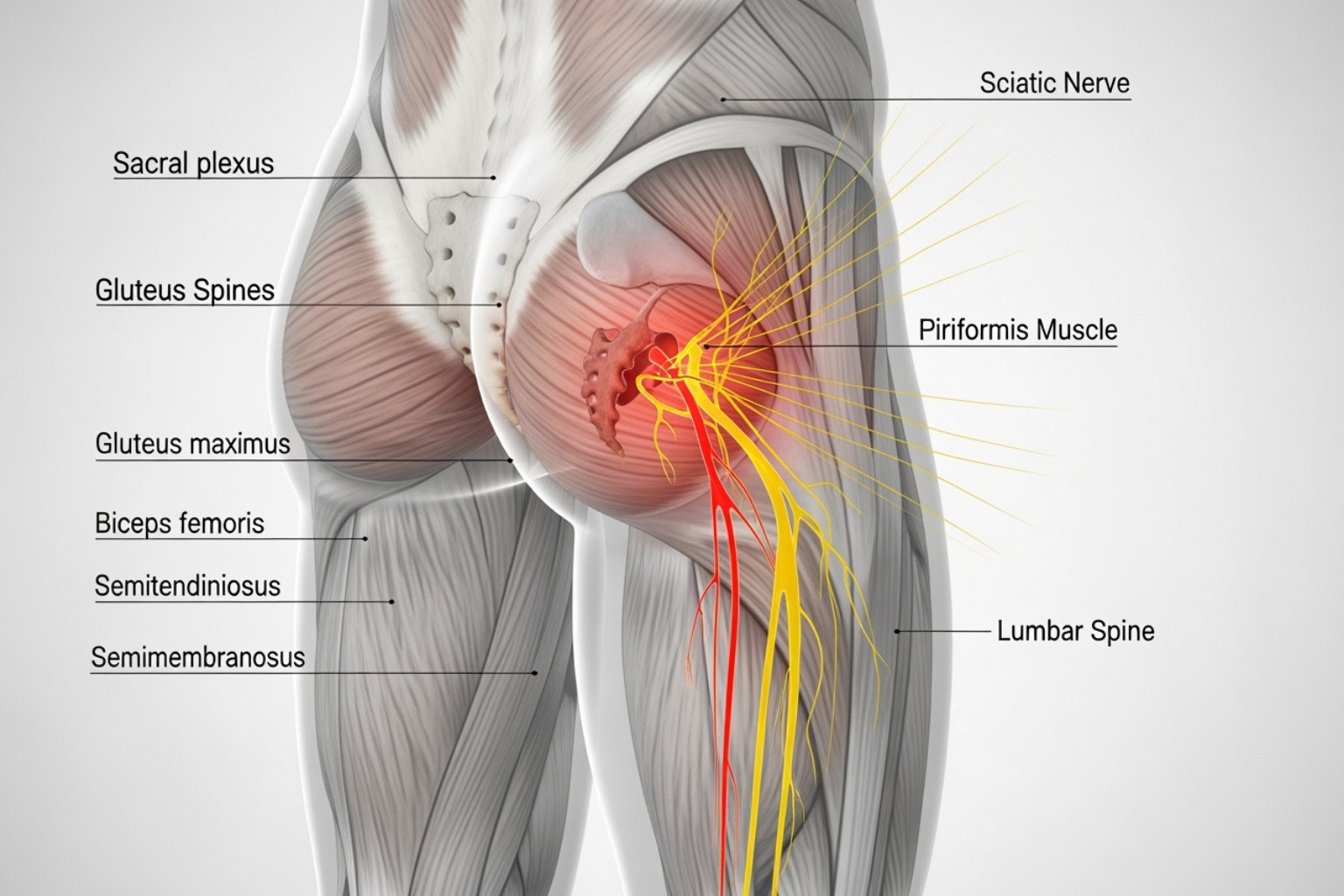
Acute sciatica pain is a common and disruptive form of nerve pain. It occurs when the sciatic nerve—the longest and thickest nerve in the body—becomes compressed or irritated, sending sharp, shooting pain from the lower back down through the buttock and leg.
Quick Answer: What You Need to Know About Acute Sciatica Pain
- What it is: Lower back pain with nerve pain (radiculopathy) that travels below the knee, lasting up to 6 weeks.
- How common: About 40% of people in the U.S. experience sciatica during their lifetime.
- Typical symptoms: Sharp, burning, or electric shock-like pain down one leg, numbness, tingling, or muscle weakness.
- Most common causes: Herniated disc, spinal stenosis, bone spurs, or muscle compression (piriformis syndrome).
- Recovery time: Most cases resolve within 4-6 weeks with conservative treatment.
- Good news: 80-90% of people get better without surgery.
Sciatica isn't a condition itself—it's a symptom of an underlying issue affecting the sciatic nerve. The nerve starts in the lower back, runs through the buttocks, and extends down each leg. When something puts pressure on this nerve, you feel pain along its pathway.
Acute vs. Chronic Sciatica
The key difference lies in duration:
- Acute sciatica lasts less than 6 weeks and often resolves with self-care and conservative treatment.
- Chronic sciatica persists beyond 12 weeks and may require more intensive medical intervention.
Most people experience acute sciatica, which is severe and sudden but temporary. While the discomfort can be debilitating, understanding what's happening and how to respond can make a significant difference in your recovery.
Decoding the Pain: Symptoms and Common Causes
Understanding what acute sciatica pain feels like and what's causing it can guide you toward the right relief strategies.
Hallmark Symptoms of Acute Sciatica
Acute sciatica pain is often described as a sharp, burning sensation or an electric shock that shoots from the lower back down the leg. The pain follows a distinctive pathway, starting in the lower back, traveling through the buttock, and radiating down the back of the leg, often below the knee. Sciatica almost always affects just one side of the body.
Beyond pain, you might notice numbness, tingling ("pins and needles"), or muscle weakness in your leg or foot. These symptoms signal that a nerve is being compressed or irritated. Everyday actions like coughing, sneezing, or sitting for long periods can intensify the pain, making it difficult to find a comfortable position.
For a more detailed exploration of these symptoms, see our comprehensive guide on sciatica symptoms.
The Most Common Causes of Sciatic Nerve Compression
Sciatica is a symptom that something is putting pressure on the sciatic nerve or its nerve roots.
The most frequent culprit is a herniated disc. Spinal discs have a soft center and a tough exterior. When the outer layer tears, the inner material can push out and press on a nerve root.
Other common causes include:
- Spinal stenosis: A narrowing of the spinal canal that puts pressure on the spinal cord and nerves, often due to age-related wear and tear.
- Bone spurs (osteophytes): Bony growths on the vertebrae that can pinch the sciatic nerve.
- Piriformis syndrome: When the piriformis muscle in the buttock tightens or spasms, it can compress the sciatic nerve, which runs nearby.
- Degenerative disc disease: An age-related condition where spinal discs lose moisture and elasticity, making them more prone to damage.
As Dr. Kevin Taliaferro notes in what doctors wish patients knew about sciatica, sciatica is a broad term for what can be a multi-faceted issue, which is why an accurate diagnosis is important. For more information, see our definitive guide to what causes sciatic nerve pain.
Is It Sciatica or Something Else?
Not all leg or back pain is sciatica. General low back pain is typically localized and doesn't radiate down the leg. Hip problems, such as arthritis, usually cause pain in the groin or outer hip and worsen with hip rotation.
The key differentiator for sciatica is pain radiating below the knee. While other conditions can cause thigh or buttock pain, discomfort that travels from the lower back or buttock down the leg past the knee is almost certainly sciatica. If the pain feels like a nerve being zapped rather than a sore muscle, a nerve is likely involved. For more details on pain levels, our guide from mild to intense sciatica pain can help you understand your symptoms.
Immediate Self-Care Strategies for Acute Sciatica Pain
When acute sciatica pain strikes, you can use several effective at-home strategies to manage pain, improve mobility, and begin your recovery.
At-Home Remedies for Quick Relief
Hot and Cold Therapy: During the first 48-72 hours, apply an ice pack wrapped in a towel to the painful area for 15-20 minutes at a time to reduce inflammation. After the initial phase, switch to a heating pad or warm bath to relax tense muscles and improve blood flow.
Gentle Movement: While rest is tempting, prolonged bed rest can worsen stiffness. Gentle movement, such as short walks, is beneficial. Listen to your body and avoid any activity that increases pain.
Positional Relief: The right sleeping position can relieve pressure on the sciatic nerve. If you sleep on your back, place a pillow under your knees. If you're a side sleeper, place a pillow between your knees to align your hips, pelvis, and spine.
For a comprehensive look at natural pain management, check out our guide on 7 Proven Natural Ways to Treat Sciatica Pain at Home for Fast Relief.

The Role of Over-the-Counter Approaches
Over-the-counter solutions can be valuable for managing acute sciatica pain. Oral pain relievers like nonsteroidal anti-inflammatory drugs (NSAIDs)—such as ibuprofen or naproxen—work by reducing both pain and inflammation. Always follow dosage instructions and consult a healthcare professional if you have underlying health conditions.
Topical nerve pain relief creams offer a targeted alternative. Applying a cream directly to the painful area delivers relief where it's needed most, without the systemic side effects of oral medications.
Our Neuropasil Nerve Pain Relief Cream is formulated with natural ingredients like Aloe, Urea, and Menthol to calm irritated nerves and relax tense muscles. The cooling sensation provides therapeutic comfort. Many customers rely on our cream for sciatica, neuropathy, fibromyalgia, and general joint or muscle discomfort, as it allows them to manage pain without the concerns associated with oral medications.
For a deeper understanding of how topical solutions can help, explore our deep dive into topical solutions for nerve pain.
Safe Exercises to Alleviate Acute Sciatica Pain
Gentle, targeted exercises are a powerful tool for relief. They are designed to take pressure off the nerve, improve flexibility, and strengthen the muscles supporting your spine. Always warm up with a few minutes of light movement before stretching.
Knee-to-chest stretch: Lie on your back with knees bent. Gently pull one knee to your chest, hold for 20-30 seconds, and switch legs. This helps decompress the lower spine.
Seated piriformis stretch: Sit in a chair and place the ankle of your affected leg on your opposite knee. Lean forward slightly with a straight back until you feel a stretch in your buttock. Hold for 20-30 seconds.
Cat-cow stretch: On your hands and knees, alternate between arching your back (dropping your belly) and rounding it (pulling your belly button to your spine). This mobilizes the entire spine.
Hamstring stretch: Lie on your back and loop a towel around the arch of one foot. Gently pull the towel to straighten your leg until you feel a stretch. Hold for 20-30 seconds.

Crucially, never push through pain. If a stretch worsens your symptoms, stop immediately. Consistency and caution are key. For more insights, explore our drug-free sciatica solutions.
Navigating Professional Care
While self-care is effective, professional guidance is sometimes essential for managing acute sciatica pain. Knowing when to seek help can ensure a smoother recovery.
When to See a Doctor for Your Pain
Consult a healthcare provider if your pain persists beyond a week or two despite home care, or if it worsens. Severe, debilitating pain that interferes with daily life also warrants immediate medical attention. Pain following a significant injury, such as a car accident or fall, should always be evaluated by a doctor.
Certain "red flag" symptoms require emergency care as they may indicate Cauda Equina Syndrome, a serious condition requiring urgent treatment to prevent permanent damage. Seek immediate help for:
- Loss of bladder or bowel control
- Sudden or progressive weakness in one or both legs
- Numbness in the inner thighs, groin, or rectal area ("saddle anesthesia")
The Cleveland Clinic advises, "Call your doctor if self-care measures don't ease symptoms, if pain lasts longer than a week, is severe, or worsens." For more guidance, the Cleveland Clinic's resource on sciatica is an excellent reference.
What to Expect from Medical Evaluation
A medical evaluation for acute sciatica pain typically begins with a thorough medical history and a physical examination. Your doctor will check your reflexes, muscle strength, and sensation. A common diagnostic test is the straight leg raise, where lifting the affected leg while you lie on your back reproduces the pain, suggesting nerve irritation.
Most cases of acute sciatica do not require immediate imaging. However, if your pain is severe, persistent, or accompanied by red flag symptoms, your doctor may order tests. X-rays can show bone issues, while MRI or CT scans provide detailed images of soft tissues like discs and nerves. Nerve conduction studies (EMG) may be used to assess nerve damage.
Doctors typically emphasize conservative, non-invasive care first. This may include physical therapy, lifestyle modifications, and topical pain relief. Our nerve pain relief cream can complement your doctor's plan by providing targeted relief. For more on this topic, see our article on finding the best topical for sciatica.
The Role of Physical Therapy and Advanced Interventions
For most people, a comprehensive treatment plan for acute sciatica pain starts with physical therapy and may progress to other interventions if needed.
Physical therapy is often the cornerstone of recovery. A physical therapist will guide you through exercises to strengthen core muscles, improve flexibility, and reduce nerve pressure. This may involve manual therapy, customized exercises, and education on safe movement.
If over-the-counter options are insufficient, a doctor might prescribe muscle relaxers, stronger anti-inflammatories, or nerve pain medications.
For severe pain that doesn't respond to other treatments, epidural steroid injections may be considered. These injections deliver corticosteroids near the spinal nerves to reduce inflammation and provide temporary pain relief, which can help you participate more effectively in physical therapy.
Encouragingly, 80% to 90% of people with sciatica get better without surgery. Surgery is a last resort, typically considered only after conservative treatments fail, if there is progressive neurological decline, or in emergencies like Cauda Equina Syndrome. The goal is always to find the least invasive, most effective path to recovery.
The Road to Recovery: Prognosis, Prevention, and Long-Term Health
Understanding the recovery timeline and adopting preventive habits can help you heal from acute sciatica pain and reduce the risk of future flare-ups.
Recovery Time and Potential Complications
While it may feel relentless, the intense pain of acute sciatica is usually temporary. Most cases of acute sciatica resolve within 4 to 6 weeks with conservative treatment. The body's natural healing processes, combined with proper management, are highly effective.
Full recovery and strengthening may take longer. Consistency with exercises and lifestyle adjustments is crucial for both immediate and long-term relief.
However, ignoring severe or persistent sciatica can lead to complications. Permanent nerve damage is a risk with prolonged nerve compression, potentially causing chronic pain, numbness, or weakness. A specific complication is foot drop, where muscle weakness makes it difficult to lift the front of your foot. If acute sciatica is not properly addressed, it can transition into chronic pain, which persists beyond 12 weeks and is more difficult to treat.
Timely intervention is key to preventing these complications and ensuring a smooth recovery. For a comprehensive guide, see our guide to sciatica relief.
Lifestyle Modifications to Prevent Future Episodes
Once you recover from acute sciatica pain, certain lifestyle changes can significantly reduce your risk of recurrence.
Regular Exercise: Focus on strengthening your core (abdominal and back muscles) to support your spine. Activities like planks, bird-dogs, and gentle yoga or Pilates are excellent choices.
Good Posture: When sitting, use a supportive chair with your feet flat on the floor. When standing, keep your back straight and weight evenly distributed. A lumbar support pillow can help maintain the natural curve of your lower back.
Proper Lifting Techniques: Always bend at your knees, not your waist. Keep objects close to your body and use your leg muscles to lift. Avoid twisting while lifting.

Maintain a Healthy Weight: Excess body weight adds stress to your spine. A balanced diet and regular activity help protect your back.
Avoid Prolonged Sitting: Take frequent breaks to stand, stretch, and walk around, especially if you have a desk job.
Quit Tobacco: Nicotine impairs blood flow to spinal discs, hindering their ability to heal and increasing injury risk.
By integrating these habits, you invest in a healthier, more comfortable future. For more on posture, how to maintain good posture is a valuable resource.
Frequently Asked Questions about Acute Sciatica Pain
How long does acute sciatica typically last?
Most cases of acute sciatica pain resolve within 4 to 6 weeks with conservative self-care and treatment. The exact duration can vary depending on the underlying cause, your overall health, and how closely you follow your treatment plan. If you don't see improvement after a couple of weeks, or if the pain worsens, consult your doctor.
Can I exercise with acute sciatica?
Yes, gentle movement is encouraged. Activities like short walks and specific, gentle stretches can help reduce pain and speed up recovery. However, you should avoid strenuous exercise, heavy lifting, and any movements that significantly worsen your pain. A physical therapist can help design a safe and effective exercise program for your specific needs.
How can I differentiate sciatica from other types of back pain?
The hallmark of sciatica is pain that radiates from the lower back, through the buttock, and down the path of the sciatic nerve in the leg, often extending below the knee. It is typically accompanied by nerve-related symptoms like numbness, tingling, or weakness. In contrast, general low back pain is usually localized to the back, and hip problems typically cause pain in the groin or outer hip, not radiating down the leg.
Conclusion
When acute sciatica pain strikes, it can be overwhelming. However, while the pain is intense, it is usually temporary, and you have significant control over your recovery.
Self-care is a powerful first step. Simple strategies like hot and cold therapy, gentle movement, and supportive sleeping positions can provide substantial relief. At the same time, knowing when to seek professional help is crucial. If pain persists, worsens, or is accompanied by "red flag" symptoms, consult a healthcare provider. 80-90% of people recover without surgery.
Prevention is key for long-term health. Maintaining good posture, strengthening your core, and using proper lifting techniques can dramatically reduce your risk of future episodes.
For targeted, soothing relief, natural topical solutions like Neuropasil Nerve Pain Relief Cream can be a valuable part of your management plan. Our formula, with Aloe, Urea, and Menthol, calms irritated nerves and relaxes sore muscles without the systemic side effects of oral medications.
You are not alone on this journey. To see how Neuropasil can help, explore our drug-free solutions for nerve pain relief. For more information on topical treatments for sciatica, read our ultimate guide to the best cream for sciatica pain.
Healing takes time, but with the right approach, you can reclaim your comfort and return to the activities you love.
References
Throughout this guide on acute sciatica pain, we've drawn upon trusted medical institutions and research to ensure you receive accurate, reliable information.
The foundational understanding of sciatica comes from leading healthcare organizations. The Mayo Clinic provides extensive information on sciatica symptoms and causes, and the Cleveland Clinic offers detailed guidance on sciatica diagnosis and treatment.
We were particularly struck by insights from the American Medical Association, whose article on what doctors wish patients knew about sciatica highlighted the importance of an accurate diagnosis. The NHS inform resource on sciatica also provided a valuable perspective on conservative treatment.
For broader context, the National Institute of Neurological Disorders and Stroke offers a comprehensive low back pain fact sheet. The Cleveland Clinic also contributed specific guidance on maintaining good posture, which is essential for prevention.
Practical self-care strategies were informed by sources like Mount Nittany Health's guide on sciatica self-care at home. Research on treatment effectiveness was informed by the Family Physicians Inquiries Network study on the most effective therapies for acute sciatica.
We are committed to providing evidence-based information you can trust, because managing acute sciatica pain effectively starts with understanding the facts.














