What You Need to Know About Sciatica Symptoms
Sciatica symptoms are a common form of nerve pain, affecting up to 40% of people in the U.S. The condition is known for its sharp, shooting pain that travels from the lower back, through the buttock, and down the leg, often described as a burning or electric shock sensation.
The most common sciatica symptoms include:
- Sharp, shooting pain radiating from the lower back down one leg
- Burning or electric shock-like sensations along the nerve path
- Numbness and tingling in the leg, foot, or toes
- Muscle weakness in the affected leg
- Pain that worsens with sitting, coughing, or sneezing
- One-sided symptoms, as sciatica usually affects only one leg
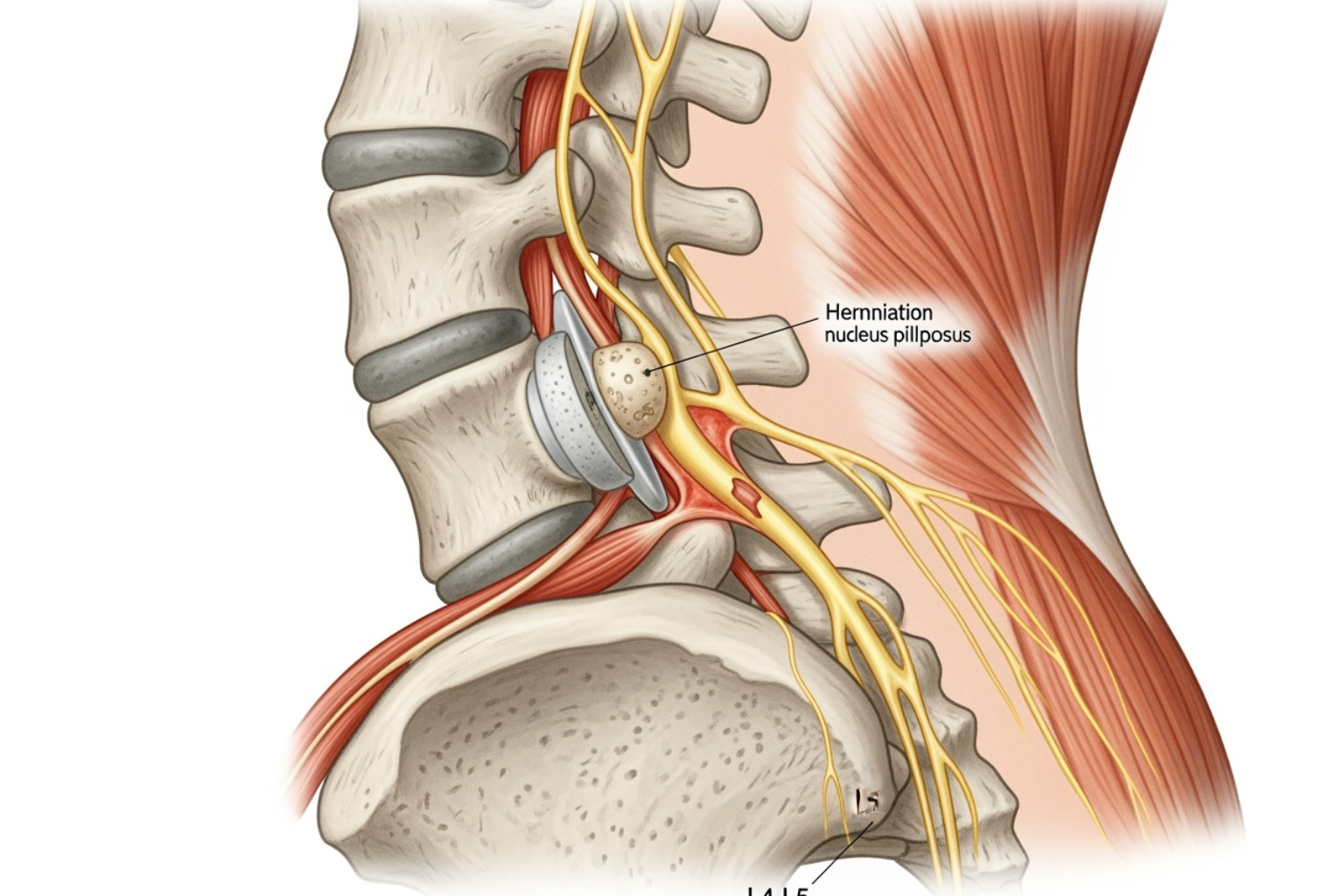
The sciatic nerve, the longest and thickest in the body, extends from your lower back down each leg. When compressed or irritated by issues like a herniated disc or spinal stenosis, it causes the radiating pain that defines sciatica.
While most common between ages 30-50, sciatica can occur at any age. Fortunately, 80-90% of people recover without surgery, typically within 4-6 weeks with proper care.
I'm Tony Enrico, and my work in developing pain relief solutions has shown me that early recognition of sciatica symptoms and effective pain management are key to improving recovery and quality of life.
Understanding the Most Common Sciatica Symptoms
If you've felt a sharp pain travel from your lower back down your leg, you might be experiencing sciatica symptoms. This isn't a typical backache; it's a distinctive nerve pain caused by irritation or compression of the sciatic nerve, the longest and thickest nerve in your body. This nerve starts in your lower spine and runs down each leg to your toes. When it's affected by a herniated disc, spinal stenosis, or other issues, it creates the signature radiating pain of sciatica.
Sciatica symptoms are unique because the pain travels. The intensity can range from a dull ache to sharp, shooting bolts. Key characteristics include:
- One-sided pain: Sciatica almost always affects just one leg. Pain in both legs is rare and requires immediate medical attention.
- Lower back, buttock, and leg pain: The pain often starts in the lower back but is most defined by its path through the buttock and down the leg, sometimes reaching the foot. The exact path depends on which nerve root is affected.
- Sensory and motor changes: Beyond pain, you might experience numbness, "pins and needles" tingling, or strange hot/cold sensations. More concerning symptoms include muscle weakness, difficulty lifting your foot ("foot drop"), or changes in your gait.
- Triggers: Symptoms often worsen with prolonged sitting, coughing, sneezing, or bending forward.
For a comprehensive look at how these sensations manifest, our guide on Sciatica Pain Symptoms provides additional insights.
Decoding Your Sciatica Pain Symptoms
Learning to identify sciatica symptoms can help you get the right treatment faster.
- Sciatica vs. General Back Pain: The main difference is that sciatica pain travels, often past the knee, while general back pain usually stays localized.
- Pain vs. Numbness: You can experience both at once. Nerve compression affects different nerve fibers, some carrying pain signals and others handling sensation.
- Tingling and "Pins-and-Needles": This sensation, called paresthesia, is a clear sign your nerve isn't functioning normally.
- Muscle Weakness: If your leg feels weak or your foot drags, the nerve compression may be affecting muscle control. This requires prompt medical evaluation.
- Acute vs. Chronic Pain: Acute sciatica appears suddenly and usually resolves in a few weeks. Chronic sciatica persists for months and requires more comprehensive management.
What Does Sciatica Pain Feel Like?
People often use similar descriptions for sciatica symptoms:
- Burning Sensation: A deep, persistent burn that feels like it's coming from inside your leg.
- Sharp, Shooting Pain: Sudden, intense jolts that travel from your back to your foot in an instant.
- Electric Shock-like Jolts: Similar to sharp pain but even more powerful, causing muscles to contract.
- Dull, Constant Ache: A nagging discomfort that makes it hard to get comfortable in any position.
- Leg Cramps: Deep, sustained cramps that don't respond to typical remedies like stretching.
The variety and unpredictability of these sensations are a normal part of sciatica. For more information on managing these sensations, explore our resource on Sciatica Pain.
What's Behind the Pain? Causes and Risk Factors
Sciatica isn't a disease itself but a symptom that something is irritating your sciatic nerve. This major nerve pathway runs from your lower back down to your toes. When something puts pressure on it, you get the characteristic sciatica symptoms. To learn more about the source of this pressure, see our guide on Lower Back Pain Causes.
Primary Causes of Sciatica
Several conditions are common culprits behind sciatica symptoms:
- Herniated Discs: The most common cause (about 90% of cases). The soft center of a spinal disc pushes through its outer layer, pressing on a nerve root.
- Spinal Stenosis: A narrowing of the spinal canal, often due to age-related changes like bone spurs, which squeezes the nerves.
- Degenerative Disc Changes: As we age, discs lose water and flexibility, leading to bulging or bone spurs that can irritate nerve roots.
- Spondylolisthesis: One vertebra slips forward over the one below it, potentially pinching a nerve.
- Piriformis Syndrome: A muscle deep in the buttock (the piriformis) spasms and compresses the sciatic nerve.
- Pregnancy: Hormonal changes, weight gain, and shifts in posture can all put pressure on the sciatic nerve.
- Traumatic Injuries: Falls, accidents, or sports injuries can damage the spine and lead to nerve compression.
- Rare Causes: In rare instances, tumors, infections, or blood clots can cause sciatica.
Are You at Risk? Key Sciatica Risk Factors
Certain factors increase your likelihood of developing sciatica symptoms:
- Age: Herniated discs are most common in people aged 20-50, while spinal stenosis is more likely after 60.
- Excess Weight: Extra body weight, especially around the midsection, increases stress on your spine.
- Occupation: Jobs that involve heavy lifting, prolonged sitting, or frequent twisting put your back at risk.
- Sedentary Lifestyle: Weak core muscles provide less support for your spine, making it more vulnerable.
- Diabetes: High blood sugar can damage nerves, increasing susceptibility to nerve-related pain.
- Poor Posture: Slouching or standing improperly puts uneven stress on your spine over time.
- Smoking: Nicotine reduces blood flow to spinal discs, weakening them and slowing healing.
While you can't control age, you can influence many of these risk factors through lifestyle changes to protect your back.
Finding Relief: From Diagnosis to Treatment
When sciatica symptoms strike, the main goal is relief. The journey starts with a proper diagnosis, followed by a custom treatment plan.
A healthcare provider will typically perform a physical exam, checking your reflexes, muscle strength, and range of motion. The straight leg raise test, where a doctor lifts your affected leg while you lie down, is a strong indicator of sciatic nerve irritation if it reproduces your pain.
Imaging tests may be recommended in some cases. An X-ray can show bone spurs or alignment issues, while an MRI provides a detailed view of soft tissues like discs and nerves, helping to identify herniated discs or spinal stenosis. However, imaging isn't always necessary, especially if symptoms are mild and improving.

At-Home and Conservative Treatments
The great news is that 80-90% of people with sciatica get better without surgery. Most treatment plans begin with conservative methods you can do at home.
- Ice and Heat Therapy: Use cold packs for the first few days to reduce inflammation (20 minutes at a time). After that, switch to a heating pad to relax muscles. Many find alternating between hot and cold provides the best relief.
- Gentle Movement and Stretching: Contrary to instinct, extended bed rest can slow recovery. Light activities like walking and swimming, along with specific stretches for the hamstrings and lower back, can reduce inflammation and pressure on the nerve.
- Over-the-counter Topical Relief Creams: For targeted, fast-acting comfort, our Neuropasil natural solutions are formulated with ingredients like Aloe, Urea, and Menthol to soothe aggravated nerves. Applying the cream can help manage sciatica symptoms throughout the day.
- Physical Therapy-Inspired Exercises: A therapist can teach you exercises to strengthen your core and improve flexibility. A strong core acts as a natural brace for your back, relieving pressure on the sciatic nerve.
These self-care approaches often resolve sciatica symptoms within a few weeks. For more natural relief options, see our guide on Nerve Pain Relief with Neuropasil Natural Solutions.
When to Consider Advanced Care
If symptoms persist or worsen after several weeks of self-care, it's time to consult your healthcare provider. Advanced care may be needed if the pain is severe or debilitating.
In rare cases, a specialist may recommend additional interventions like corticosteroid injections to reduce inflammation around the nerve root. For the small percentage of people with severe, persistent symptoms that don't respond to other treatments, surgery might be an option. Procedures like microdiscectomy or laminectomy aim to remove whatever is pressing on the nerve, providing lasting relief.
Prevention, Complications, and When to Seek Help
The prognosis for sciatica is excellent, with 80-90% of people recovering fully without surgery, often within a few weeks. However, sciatica can recur if the underlying causes aren't addressed. Making thoughtful lifestyle adjustments is key to preventing future episodes. For more insights, A comprehensive guide to sciatica from Mayo Clinic offers excellent information.
How to Prevent Sciatica
Preventing future sciatica symptoms is possible with these effective strategies:
- Regular Exercise: Strengthen your core (abdominal and back muscles) with activities like walking, swimming, or Pilates. A strong core supports your spine and reduces pressure on discs.
- Maintain Good Posture: Sit with good lower back support and feet flat on the floor. Stand tall to minimize stress on your spinal discs.
- Proper Lifting Techniques: Always bend at your knees, not your waist. Keep heavy objects close to your body and avoid twisting while lifting.
- Healthy Weight Management: Maintaining a healthy weight reduces the load on your lower back.
- Avoid Smoking: Nicotine impairs blood flow to your spinal discs, weakening them and slowing healing.
- Ergonomic Workspace: Adjust your chair, desk, and monitor to support good posture, and take frequent breaks to stand and stretch.
When to See a Doctor for Sciatica Symptoms
While most cases improve with self-care, some situations require professional medical attention.
Contact your healthcare provider if:
- Pain persists over a few weeks despite self-care.
- Pain is severe and worsening, disrupting sleep or daily activities.
- Pain follows a violent injury, like a fall or car accident.
Seek emergency medical attention for these red flag symptoms:
- Loss of bladder or bowel control: This may signal Cauda Equina Syndrome, a rare but critical condition requiring immediate surgery.
- Progressive leg weakness or numbness: Especially if you develop "foot drop" (difficulty lifting your foot).
- Sudden, severe pain accompanied by significant numbness or muscle weakness.
If something feels seriously wrong, trust your instincts and seek medical advice promptly to ensure you receive the appropriate care.
Frequently Asked Questions about Sciatica
When dealing with sciatica symptoms, it's natural to have questions. Here are answers to some of the most common concerns.
How long does sciatica usually last?
This is probably the first thing everyone wants to know when they're dealing with sciatica symptoms - and I completely understand why! When you're experiencing that sharp, shooting pain down your leg, even a day can feel like an eternity.
Here's the encouraging news: acute sciatica typically lasts between 4 to 6 weeks. Many people with mild cases find their symptoms improve even faster, often within just a few days to two weeks with proper self-care. Your body has an amazing ability to heal itself when given the right support.
The statistics are truly on your side here. Between 80% to 90% of people recover from sciatica with conservative care - no surgery required. That's an incredibly positive outlook for something that can feel so debilitating when you're in the thick of it.
However, if your sciatica symptoms decide to overstay their welcome and persist beyond six weeks, it's time to have another conversation with your healthcare provider. Chronic sciatica can linger for months or even years, but this doesn't mean you're stuck with it forever. It simply means your treatment plan might need some adjustments or a fresh perspective.
Can sciatica affect both legs at the same time?
This question often comes up when people start feeling discomfort in their "good" leg and begin to panic. Let me ease your mind: bilateral sciatica is quite rare. The typical pattern for sciatica is that it affects one leg at a time, following the path of one sciatic nerve down one side of your body.
Think of your sciatic nerves as two separate highways running from your lower back down each leg. Usually, there's only a "traffic jam" on one side at a time. When both sides are affected simultaneously, it's like having construction on both highways - possible, but much less common.
If you are experiencing sciatica symptoms in both legs at the same time, this often indicates a more serious underlying cause. Conditions like severe spinal stenosis, where the spinal canal becomes significantly narrowed, can sometimes affect nerve roots on both sides. In very rare cases, it could signal something like Cauda Equina Syndrome, which requires immediate medical attention.
The bottom line? Bilateral sciatica requires prompt medical evaluation. Don't wait to see if it gets better on its own - your healthcare provider needs to determine what's causing symptoms on both sides.
Is bed rest good for sciatica?
I wish I had a dollar for every time someone told me they spent a week in bed hoping their sciatica symptoms would disappear! It's such a natural instinct when you're in pain - find the most comfortable position and stay there. Unfortunately, this approach often backfires.
Prolonged bed rest is actually not recommended for sciatica. While taking a day or two to rest during an acute flare-up is perfectly reasonable, staying in bed for extended periods can actually make things worse. It's counterintuitive, I know, but your body needs movement to heal properly.
Here's what happens when you stay immobile for too long: your muscles begin to weaken, your joints become stiff, and inflammation can actually increase. It's like letting a car sit in the garage for months - everything starts to seize up and work less efficiently.
Instead, gentle activity and movement are beneficial for most people with sciatica. This doesn't mean you should be running marathons or lifting heavy boxes. Think more along the lines of gentle walks around the block, light stretching, or even just changing positions regularly throughout the day. These activities help reduce inflammation and stiffness while keeping your body's natural healing processes active.
The key is finding that sweet spot between rest and activity. Listen to your body, but don't let fear of pain keep you completely sedentary. Movement, when done thoughtfully, is often one of your best allies in overcoming sciatica symptoms.
Conclusion: Your Path to a Pain-Free Life
Understanding the sharp pains, tingling, and electric jolts of sciatica symptoms is the first step toward reclaiming your comfort. Remember this key takeaway: sciatica is a treatable symptom, not a life sentence. The prognosis is overwhelmingly positive, with 80% to 90% of people recovering using conservative treatments alone.
Your body has a remarkable ability to heal, and you can support it through proactive pain management. Strengthening your core, maintaining good posture, and staying active are proven strategies to manage current pain and prevent future flare-ups of sciatica symptoms.
At Neuropasil, we've seen countless people find their way back to a comfortable life. Our natural, fast-acting topical creams, powered by Aloe, Urea, and Menthol, deliver targeted relief right where you need it. Our formula is designed to soothe aggravated nerves and provide the comfort you deserve.
Your journey transforms now. Armed with knowledge and effective self-care strategies, you can step confidently into a more comfortable future.
Ready to experience targeted, soothing relief? Find natural, topical relief for your sciatica pain and take the next step toward the pain-free life you deserve.














