Understanding Your Arthritis Treatment Options
Best arthritis medication depends entirely on your specific type of arthritis, disease severity, and personal health profile—but generally starts with over-the-counter options like acetaminophen or NSAIDs (ibuprofen, naproxen), progresses to prescription-strength NSAIDs and corticosteroids for moderate pain, and advances to disease-modifying drugs (DMARDs) or biologics for inflammatory arthritis when joint damage needs to be slowed or stopped [1].
Quick Answer: Best Arthritis Medications by Severity
| Severity Level | Best Medication Options | Key Considerations |
|---|---|---|
| Mild Pain | Acetaminophen (Tylenol), Topical NSAIDs | Fewer side effects, good for osteoarthritis |
| Moderate Pain | Oral NSAIDs (Ibuprofen, Naproxen), Prescription NSAIDs | Watch for stomach/heart risks |
| Inflammatory Arthritis | DMARDs (Methotrexate), Corticosteroids | Requires regular monitoring |
| Severe/Uncontrolled | Biologics (TNF inhibitors), JAK Inhibitors | Targeted therapy, infection risk |
Arthritis hurts. Whether you're dealing with osteoarthritis from years of wear and tear or rheumatoid arthritis attacking your joints, the pain can steal your ability to train, work, or simply enjoy daily activities.
The good news? You have options—many options.
From simple over-the-counter pills to advanced biologic injections, the landscape of arthritis treatment has evolved dramatically. But with over 100 forms of arthritis and related diseases, and dozens of medication classes to choose from, finding the right treatment can feel overwhelming.
The goal is clear: reduce inflammation, relieve pain, prevent joint damage, and help you stay active. The path to get there varies for everyone.
For osteoarthritis—where inflammation plays a minor role—acetaminophen or topical treatments might be your first stop. For inflammatory types like rheumatoid arthritis, disease-modifying drugs become critical to prevent irreversible joint damage, which often occurs within the first two years of diagnosis [2].
Some medications work fast but carry risks. Others take months to show results but can actually slow disease progression. Some are pills you swallow; others are creams you rub on or shots you inject.
This guide breaks down every major category of arthritis medication—from the pharmacy shelf to the rheumatologist's office—so you can understand what works, what the risks are, and when to move from one treatment tier to the next.
I'm Tony Enrico, and through my work with Neuropasil, I've spent years helping people find effective relief from nerve and joint pain, including exploring how topical treatments complement traditional best arthritis medication approaches for comprehensive pain management.
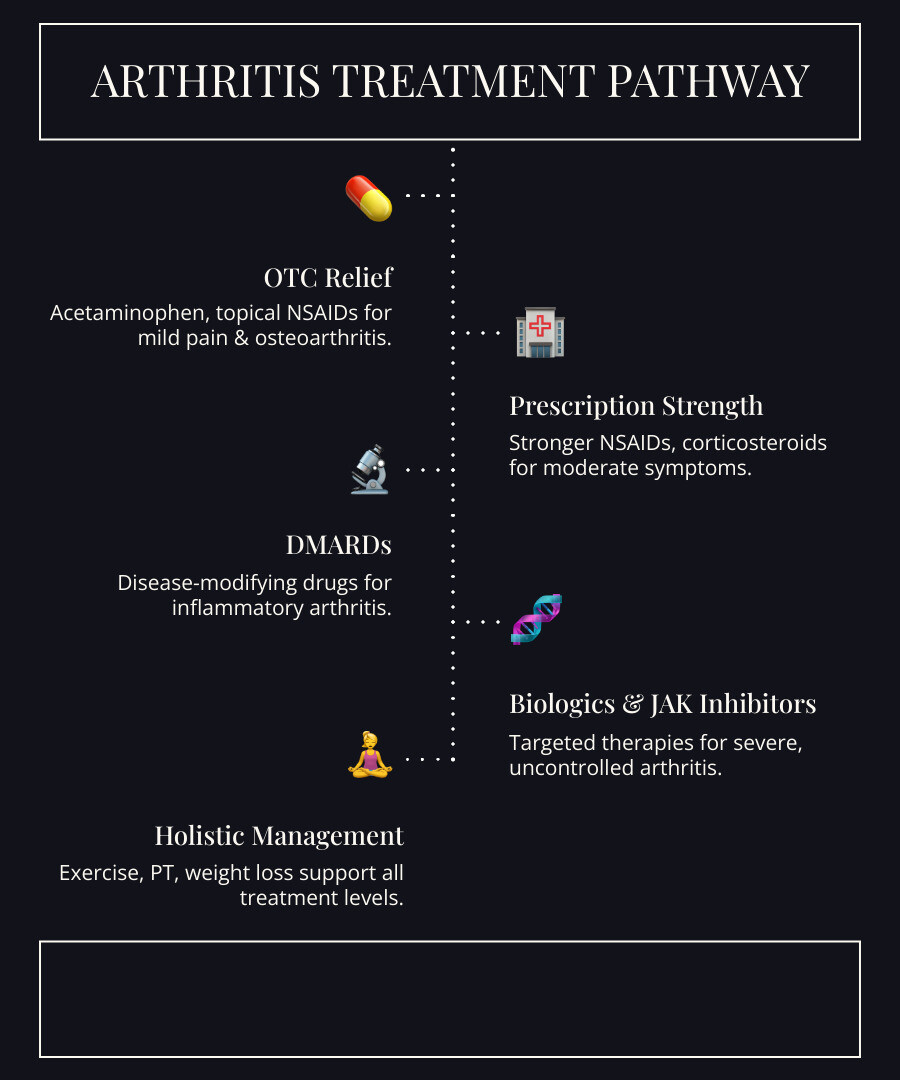
Starting with Over-the-Counter (OTC) Relief
When arthritis pain first flares up, many of us instinctively reach for something quick and easy from the local pharmacy. Over-the-counter (OTC) medications are often our first line of defense, offering accessibility and managing mild to moderate pain effectively. For many, finding the best arthritis medication starts right here.

Finding the Best Arthritis Medication Over-the-Counter
The world of OTC pain relief for arthritis can be broadly divided into two main categories: acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs). Each works a little differently, so understanding their distinctions is key to choosing wisely.
Acetaminophen (Tylenol) This is a go-to for pain relief. Acetaminophen, known as paracetamol outside the U.S., primarily targets pain, making it an excellent choice for osteoarthritis where inflammation plays a minor role. It's often the first-line drug treatment for this type of arthritis [3]. It helps ease mild to moderate pain but doesn't directly tackle inflammation.
NSAIDs (Nonsteroidal Anti-Inflammatory Drugs) Our NSAID options include popular choices like:
- Ibuprofen (Advil, Motrin): A common NSAID that works by blocking the production of pain-signaling chemicals called prostaglandins. This means it not only relieves pain but also reduces inflammation.
- Naproxen (Aleve): Another effective NSAID, similar to ibuprofen, but often provides longer-lasting relief, meaning you might take it less frequently.
- Aspirin: While historically a widely used pain reliever for arthritis, today low-dose aspirin is more commonly used for heart health prevention. For arthritis pain and inflammation, other NSAIDs are generally preferred due to aspirin's higher rate of gastrointestinal toxicity at the doses needed for significant arthritis relief [3].
Here's a quick comparison to help us decide:
| Feature | Acetaminophen (Tylenol) | NSAIDs (Ibuprofen, Naproxen, Aspirin) |
|---|---|---|
| Pain Relief | Excellent for mild to moderate pain | Excellent for mild to moderate pain |
| Inflammation Reduction | No significant effect | Reduces inflammation effectively |
| Primary Risks | Liver damage (with overdose) | Stomach bleed, heart attack, stroke, kidney problems |
Topical Treatments: Relief Right Where It Hurts
Sometimes, we want to target the pain precisely where it lives—right in our aching joints. That's where topical treatments come in. These creams, gels, and patches offer localized relief, often with fewer systemic side effects than oral medications because less of the drug is absorbed throughout the body.
Topical options include:
-
Counterirritants: These products create a distracting sensation, like heating or cooling, to help us forget about the pain.
- Menthol: Found in many topical pain relief products, menthol creates a cooling sensation that can temporarily alleviate discomfort.
- Capsaicin: Derived from chili peppers, capsaicin creams work by reducing the chemical that nerve cells use to send pain signals, creating a warming sensation.
- Topical NSAIDs: These bring the anti-inflammatory power of NSAIDs directly to the joint. A common example is diclofenac gel, which was previously prescription-only and is now available over-the-counter. This type of gel penetrates the skin to target the source of inflammation and pain locally. It's FDA-approved for short-term use for osteoarthritis pain in specific joints like the knees and hands. The American College of Rheumatology strongly recommends topical NSAIDs for knee osteoarthritis [4].
At Neuropasil, we understand the power of targeted relief. Our creams, powered by ingredients like menthol, are designed to soothe joint discomfort directly. They are a great complement to oral medications, helping us rub away the ache. Explore how these localized solutions can help us manage our pain: Beyond the pill-how topical treatments can soothe arthritis pain.
Understanding the Risks of OTC Medications
While OTC medications are convenient, we must respect their power and potential risks. It's crucial to always follow dosage instructions carefully to avoid serious side effects.
- Acetaminophen Risks: Our liver works hard to process acetaminophen. Taking too much can cause liver damage, which can be severe. The general recommendation is not to exceed 3,000 milligrams per day for most adults [5]. For individuals with liver disease or those who consume alcohol heavily, the risks are even higher.
-
NSAID Risks: NSAIDs, while effective for pain and inflammation, come with their own set of warnings [6]:
- Stomach Bleeding: NSAIDs can increase the risk of serious stomach problems, including internal bleeding and ulcers. This is why many doctors recommend taking them with food or, for long-term use, possibly with a stomach-protecting medication.
- Heart Attack and Stroke: NSAIDs can increase our chances of having a heart attack or stroke. This risk is particularly concerning for those with existing heart conditions.
- High Blood Pressure: They can also lift blood pressure.
- Kidney Problems: NSAIDs can impair renal function in certain patients, leading to salt retention, edema, and increased blood pressure, especially in those with kidney disease.
- Drug Interactions: A critical interaction to be aware of is between ibuprofen and low-dose aspirin. If we're taking low-dose aspirin for heart health, taking ibuprofen can interfere with aspirin's protective cardiovascular benefits [6].
Understanding these risks helps us make informed choices.
When to See a Doctor: Moving Beyond Self-Treatment
OTC medications are a great starting point, but there comes a time when we need professional guidance. Self-treating can only go so far, and delaying a proper diagnosis and treatment plan can lead to worse outcomes, especially for inflammatory types of arthritis where joint damage can occur rapidly.
It's important for us to know when OTC isn't enough and when it's time to bring in the experts. We should consult a doctor or pharmacist if we experience any of the following [7]:
- Hot, swollen joints: This often indicates significant inflammation that might require stronger intervention.
- Severe pain: If our pain is debilitating or significantly impacting our daily life despite OTC efforts.
- Symptoms affecting daily life: If arthritis prevents us from performing routine activities, working, or enjoying hobbies.
- Numerous joints with pain: This could signal a more widespread condition like rheumatoid arthritis.
- Unexplained symptoms: Any new or worsening symptoms that don't fit a simple explanation.
A pharmacist can offer valuable advice on OTC choices and potential drug interactions. However, for a comprehensive diagnosis and custom treatment plan, a doctor, particularly a rheumatologist (a specialist in arthritis and other musculoskeletal conditions), is indispensable. They can help us understand the nuances of our condition and guide us toward the best arthritis medication for our unique needs. For a basic understanding of arthritis, check out our guide: Arthritis 101.
Navigating Prescription Options: The Best Arthritis Medication from Your Doctor
When OTC solutions don't provide sufficient relief or if our arthritis is more severe or inflammatory, our doctor will likely recommend prescription medications. These options are designed to create custom treatment plans, effectively manage moderate to severe arthritis, and crucially, slow or even stop disease progression, especially in inflammatory conditions.
Prescription-Strength NSAIDs and Corticosteroids
Sometimes, we need a stronger version of what's available over the counter, or a powerful anti-inflammatory for quick relief.
- Prescription-Strength NSAIDs: These are simply stronger doses of NSAIDs than what we can buy OTC. They work in the same way—by reducing pain and inflammation—but are prescribed when OTC doses aren't enough. Our doctor will weigh the benefits against the increased risks of side effects, such as stomach problems, heart attack, stroke, and kidney issues, which are more pronounced with higher doses and long-term use.
-
Corticosteroids (e.g., Prednisone): These are powerful anti-inflammatory medications that act quickly by mimicking natural cortisol hormones. They're often used as a short-term "bridge" therapy to control severe flares or to provide rapid relief while other slower-acting medications, like DMARDs, begin to take effect. However, steroids are usually only taken for a short time because long-term use can have serious side effects, including:
- Weight gain
- Cataracts
- High blood pressure
- Osteoporosis (weakening of the bones)
- Easy bruising
- Muscle weakness
- Thinning of the skin
Disease-Modifying Antirheumatic Drugs (DMARDs)
For inflammatory arthritis like rheumatoid arthritis, DMARDs are a game-changer. These aren't just about pain relief; they're about slowing or stopping the inflammation that causes joints to worsen and the disease to progress. This is crucial because joint damage in rheumatoid arthritis can occur early in the disease course [2]. Common DMARDs include:
- Methotrexate: Often a first-line treatment for rheumatoid arthritis due to its efficacy and favorable toxicity profile [8]. It works by suppressing the immune system, reducing inflammation. However, it can affect our blood cells and liver, so regular blood tests are essential to monitor this [8].
- Sulfasalazine: This DMARD is sometimes used for rheumatoid arthritis, particularly for patients who might have liver issues, as it can be a preferable alternative to methotrexate in some cases.
- Hydroxychloroquine: Often considered for very mild, seronegative, and nonerosive forms of rheumatoid arthritis. While generally well-tolerated, regular eye exams are necessary due to a rare risk of ocular toxicity [8].
The main downside of DMARDs is that they work by weakening our immune system's ability to fight germs, which raises our chances for getting infections. Also, they can take weeks or even months to show their full effect, which is why corticosteroids are sometimes used initially as a bridge [8].
What is the Best Arthritis Medication for Severe Pain? Biologics & JAK Inhibitors
When conventional DMARDs aren't effective enough to control severe inflammatory arthritis, our doctor might consider more targeted therapies: biologics and JAK inhibitors. These represent some of the most advanced best arthritis medication options available today.
-
Biologics: These are a special type of DMARD. Unlike traditional DMARDs that broadly suppress the immune system, biologics target specific molecules or pathways involved in the inflammatory process. They are powerful and effective for many people with inflammatory arthritis. Examples include:
- TNF inhibitors (e.g., adalimumab, etanercept, infliximab): These block tumor necrosis factor (TNF), a key inflammatory protein.
- Other biologics target different inflammatory pathways, such as interleukins (IL-6 inhibitors) or specific immune cells (B-cell depletion, T-cell costimulatory blockers). Biologics are typically administered via self-injection or IV infusion, and often used in combination with methotrexate. However, with all TNF antagonists and other biologics, there is an increased risk of infection, both mild and severe, because they still weaken the immune system.
- JAK Inhibitors (Janus Kinase Inhibitors): These are a newer class of targeted synthetic DMARDs. They are small-molecule drugs that work inside cells to block signals that cause inflammation. They are taken orally and are an option for patients with rheumatoid arthritis or psoriatic arthritis who haven't responded well to other treatments, including biologics. Like biologics, JAK inhibitors also carry an increased risk of infection, and some, like tofacitinib, have been associated with a possible increased risk of cardiovascular events and malignancies, as noted by the FDA [9].
These advanced therapies are reserved for more severe cases due to their potency, cost, and potential side effects, but they can dramatically improve the lives of individuals with challenging inflammatory arthritis.
Beyond the Pill: A Holistic Approach to Arthritis Management
While medications are vital, we've learned that truly effective arthritis management involves a comprehensive approach. Combining medication with lifestyle changes, physical therapies, and even some complementary treatments can significantly improve our quality of life and help us regain control over our bodies.
Exercise as Medicine
"Exercise is medicine." It’s a powerful statement, and for arthritis, it’s absolutely true. Regular physical activity is one of the most effective non-pharmacological treatments for arthritis pain and inflammation [10].
How does it help?
- Pain Relief: Movement keeps joints lubricated and can reduce stiffness.
- Reducing Inflammation: Regular exercise helps reduce systemic inflammation in the body.
- Strengthening Muscles: Strong muscles around our joints provide better support and protection, reducing stress on the affected areas.
- Overall Health Benefits: Exercise also decreases fatigue, reduces anxiety and depression, increases bone density, and lowers our risk of heart disease—all common concerns for people with arthritis.
The key is choosing the right kind of exercise. We recommend:
- Low-impact aerobics: Activities like walking, cycling, or swimming are excellent for heart health and endurance without putting excessive stress on our joints.
- Flexibility exercises: Practices like yoga or Tai Chi improve range of motion and joint flexibility, helping us move more freely.
- Light strength training: Building muscle mass is crucial for supporting our joints.
Choosing to exercise regularly means we are managing our arthritis; it isn’t managing us. Consult a health professional trained in exercise and arthritis, such as a physical therapist or specialized kinesiologist, to get started safely and effectively.
Physical Therapy, Surgery, and Lifestyle Changes
Beyond exercise, a range of other non-pharmacological approaches can significantly impact our arthritis journey.
- Physical Therapy (PT): A physical therapist can create a personalized program to improve our range of motion, strengthen muscles around affected joints, and teach us proper body mechanics to reduce strain.
- Occupational Therapy (OT): An occupational therapist can help us adapt our daily activities and environments to protect our joints and conserve energy. They might recommend assistive devices like specialized jar openers or tools to make tasks easier.
- Assistive Devices: Canes, walkers, braces, and splints can help protect joints, reduce pain, and improve mobility.
-
Surgery: For severe joint damage, especially in conditions like osteoarthritis or advanced rheumatoid arthritis, surgery may be considered. Options include:
- Joint Repair: To smooth joint surfaces or realign bones.
- Joint Replacement (Arthroplasty): For severely damaged joints, particularly hips and knees, where the damaged parts are replaced with artificial ones. These prosthetic joints can last 10 to 20 years [12].
- Joint Fusion: In some cases, fusing bones together can reduce pain, though it eliminates joint movement.
- Weight Loss: Excess weight puts immense stress on weight-bearing joints like our knees and hips. Losing even a modest amount of weight can make a big difference. Studies show that losing at least 10% of body weight (e.g., 20 pounds for a 200-pound person) can cut osteoarthritis pain in half [11].
- Heat and Cold Therapy: Simple home remedies can offer significant relief. Applying heat can relax stiff muscles and joints, while cold packs can reduce swelling and numb pain.
For more detailed strategies on managing daily pain, we encourage you to read our guide: Managing arthritis pain-a guide to long-lasting relief.
Complementary and Alternative Therapies
Many of us explore complementary and alternative therapies (CAM) in our quest for relief. While some show promise, it's crucial to approach them with a healthy dose of skepticism and always discuss them with our doctor, especially due to potential interactions with other medications.
- Acupuncture: This ancient Chinese practice involves inserting fine needles into specific points on the body. While some people report short-term benefits for arthritis pain, the evidence for long-term effectiveness is mixed.
- Glucosamine and Chondroitin: These supplements are popular for osteoarthritis. Some studies suggest they may ease aches for moderate to severe knee OA, but the overall evidence is mixed [13]. If we choose to try them, it's recommended to take them for at least three months to assess effectiveness [14]. Supplements are not as strictly regulated as drugs, so quality can vary.
- Fish Oil Supplements: Rich in omega-3 fatty acids, fish oil may help reduce symptoms of some arthritis types due to its anti-inflammatory properties. However, they can interfere with certain medications, so always consult a doctor.
- Massage: A gentle massage can temporarily relieve muscle stiffness and pain around affected joints.
- Yoga and Tai Chi: These mind-body practices combine gentle movements, stretching, and meditation, which can improve flexibility, balance, and reduce stress, easing arthritis symptoms.
While these therapies might not be the best arthritis medication in a conventional sense, they can be valuable additions to a holistic pain management plan for some individuals. The key is to be informed and work with our healthcare team.
Conclusion: Creating Your Personalized Arthritis Action Plan
Navigating arthritis medications can feel like a complex journey, but understanding the different tiers of treatment empowers us to take control. There is no single "best arthritis medication" that works for everyone. Our ideal path is unique, depending on our specific type of arthritis, its severity, our individual health profile, and our personal preferences.
We've explored everything from accessible over-the-counter options like acetaminophen and NSAIDs, along with soothing topical treatments, to potent prescription medications such as corticosteroids, DMARDs, biologics, and JAK inhibitors. We've also highlighted the critical role of non-pharmacological approaches—exercise, physical therapy, weight management, and complementary therapies—in achieving holistic relief.
The most important takeaway is the power of shared decision-making. Always engage openly with our healthcare provider—our doctor, rheumatologist, and pharmacist—to discuss our symptoms, concerns, and treatment goals. Together, we can craft a personalized arthritis action plan that leverages the most effective and safest options for us.
At Neuropasil, we're dedicated to helping you find comfort. Whether you're dealing with the everyday aches of arthritis or seeking targeted relief for nerve and muscle pain, our fast-acting topical creams are designed to provide soothing support.
Find your comfort with our fast-acting pain relief cream
Explore our blog for more tips on managing pain
Sources
- Arthritis - Diagnosis and treatment - Mayo Clinic
- Rheumatoid Arthritis (RA) Treatment - Johns Hopkins Arthritis Center
- Comparing Pain Meds for Osteoarthritis - Arthritis Foundation
- 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee - Arthritis & Rheumatology
- Acetaminophen Information - U.S. Food and Drug Administration (FDA)
- FDA Drug Safety Communication: FDA strengthens warning that non-aspirin nonsteroidal anti-inflammatory drugs (NSAIDs) can cause heart attacks or strokes - U.S. Food and Drug Administration (FDA)
- When to See a Doctor for Arthritis Pain - Arthritis Foundation
- 2021 American College of Rheumatology Guideline for the Treatment of Rheumatoid Arthritis - Arthritis & Rheumatology
- FDA requires warnings about increased risk of serious heart-related events, cancer, blood clots, and death for JAK inhibitors - U.S. Food and Drug Administration (FDA)
- Physical Activity for Arthritis - Centers for Disease Control and Prevention (CDC)
- Losing Weight Is a First-line Treatment for Knee Osteoarthritis Pain - Arthritis Foundation
- Total Knee Replacement - American Academy of Orthopaedic Surgeons (AAOS)
- Glucosamine and Chondroitin for Osteoarthritis - National Center for Complementary and Integrative Health (NCCIH)
- Glucosamine and Chondroitin Sulfate - Arthritis Foundation















