What You Need to Know About Diabetes Neuropática
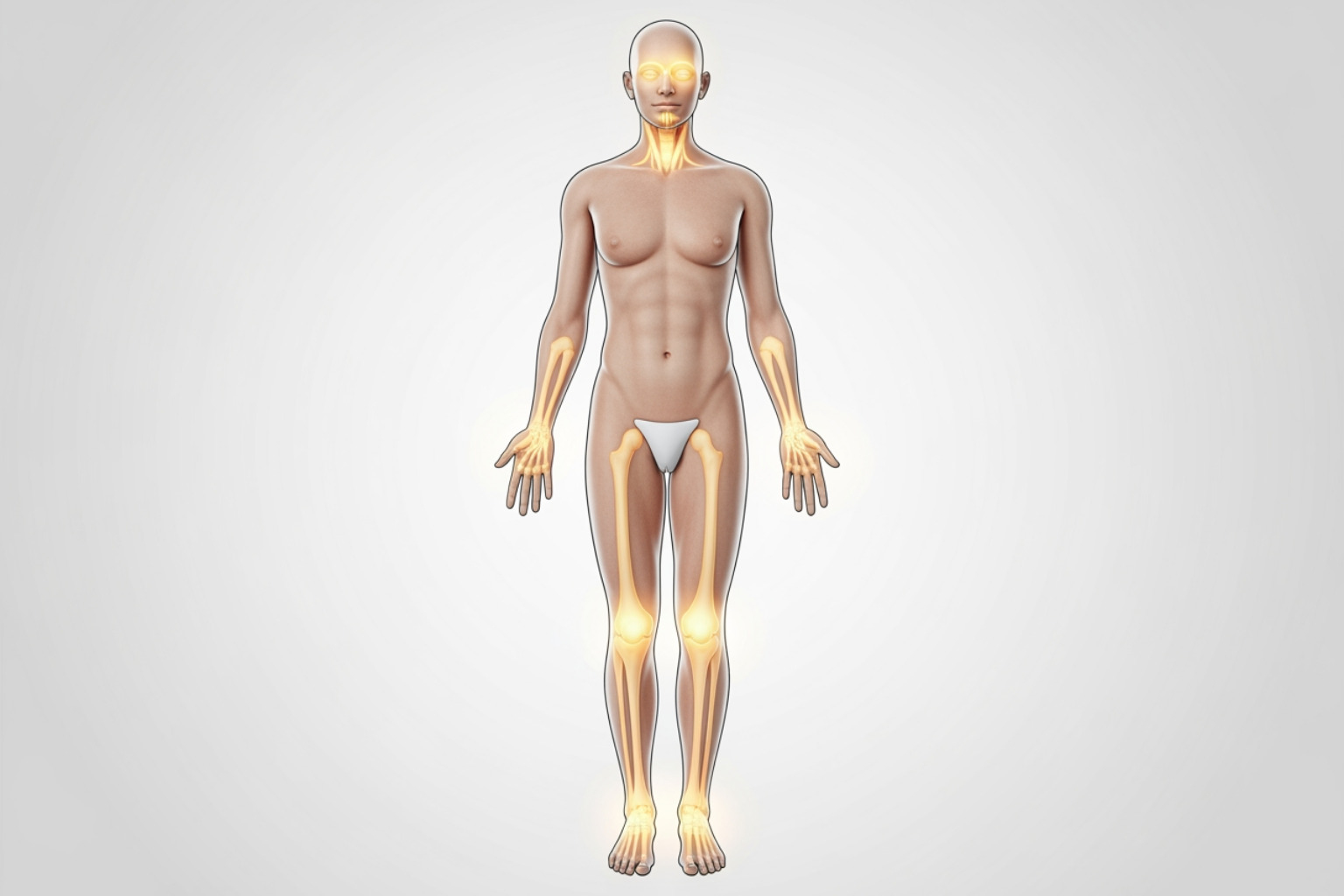
Diabetes neuropática is nerve damage caused by prolonged high blood sugar levels in people with diabetes. It's one of the most common complications of diabetes, affecting up to 50% of people living with the condition. This nerve damage primarily impacts the peripheral nervous system (nerves in your feet, legs, hands, and arms) and the autonomic nervous system (nerves controlling internal organs). Understanding this condition is crucial because it can significantly impact your daily life, from causing painful sensations and loss of feeling to affecting your heart, digestive system, and bladder.
Quick Answer: Diabetes neuropática is progressive nerve damage resulting from chronic high blood glucose levels. It manifests in four main types:
- Peripheral Neuropathy - Most common; affects extremities with numbness, tingling, burning pain
- Autonomic Neuropathy - Affects internal organs, heart rate, digestion, bladder control
- Proximal Neuropathy - Causes severe pain and weakness in hips, thighs, buttocks
- Focal Neuropathy - Sudden damage to specific nerves, often in the head, torso, or legs
Key Statistics:
- Diabetes is the most common cause of neuropathy in the Western world
- Approximately 20% of patients with diabetes experience chronic neuropathic pain
- The condition can be prevented or slowed through strict blood sugar control
The good news? While nerve damage is challenging to reverse completely, managing your blood glucose levels, maintaining a healthy lifestyle, and using targeted relief strategies can significantly slow progression and improve symptoms.
I'm Tony Enrico, founder of Neuropasil, and I've dedicated my work to helping people find relief from the debilitating effects of nerve pain, including diabetes neuropática. Through years of research and listening to thousands of people living with neuropathy, I've seen how proper management and the right supportive therapies can restore comfort and quality of life.
Diabetes neuropática basics:
Types and Symptoms of Diabetes Neuropática
Diabetes neuropática is not a single condition but rather a group of nerve disorders that can affect different parts of your body. The type of neuropathy you experience depends on which nerves are damaged. Understanding these distinctions is key to recognizing symptoms and seeking appropriate care.
Peripheral Neuropathy
This is the most common form of diabetes neuropática, primarily affecting the nerves in your feet, legs, hands, and arms. Think of it as your body's outer communication lines getting fuzzy. The symptoms often develop gradually, sometimes going unnoticed until significant nerve damage has occurred.
Common symptoms we see include:
- Numbness or reduced ability to feel pain or temperature changes, especially in the feet. This can be particularly dangerous as it might lead to unnoticed injuries.
- Tingling or burning sensations, often described as a "pins and needles" feeling.
- Sharp pains or cramps. For some, even the weight of a bedsheet can cause extreme discomfort.
- Extreme sensitivity to touch, where light contact can feel painful (allodynia).
- Muscle weakness, which can make simple tasks like gripping objects or walking challenging.
- Loss of balance and coordination, increasing the risk of falls.
These symptoms often worsen at night and typically affect both sides of your body. If you're experiencing any of these, especially in your extremities, it's crucial to identify nerve damage symptoms and consult your doctor.
Autonomic Neuropathy
Autonomic neuropathy affects the nerves that control your involuntary body functions – the ones you don't even think about. These nerves regulate your heart rate, blood pressure, digestion, bladder, sweat glands, and sex organs. When these systems go awry, it can lead to a host of surprising symptoms:
- Heart and blood vessels: You might feel light-headed or dizzy when standing up (orthostatic hypotension) due to issues with blood pressure regulation. Damage to these nerves can also make your heart respond more slowly to stress or exercise, and can even hide the warning signs of a heart attack.
- Bladder and bowels: Bladder control issues, such as difficulty emptying your bladder completely (leading to urinary tract infections), or, conversely, incontinence. Digestive problems like constipation, diarrhea, or a combination of both are also common.
- Stomach (gastroparesis): This is a condition where your stomach empties too slowly, leading to nausea, vomiting, bloating, loss of appetite, and early satiety. This can make blood sugar control very difficult.
- Sweat glands: You might experience excessive sweating (hyperhidrosis), particularly during meals (gustatory sweating), or a reduced ability to sweat (anhidrosis), leading to heat intolerance.
- Sex organs: For men, this can manifest as erectile dysfunction, and for women, as vaginal dryness or difficulty with arousal.
- Eyes: Damage to nerves controlling your pupils can make them slow to respond to changes in light, causing difficulties with night driving.
- Hypoglycemia unawareness: A particularly dangerous symptom where your body no longer sends warning signals (like shakiness or sweating) when your blood sugar drops too low.
Proximal Neuropathy (Diabetic Amyotrophy)
This is a rarer but often severely debilitating form of diabetes neuropática. It affects the nerves in your thighs, hips, or buttocks, typically on one side of the body. We often see it more frequently in older men with type 2 diabetes.
Key symptoms include:
- Sudden, severe pain in the hip, buttock, or thigh.
- Weak and atrophied thigh muscles, making it difficult to stand up from a sitting position.
- Loss of reflexes in the affected leg.
- Significant weight loss.
The good news is that proximal neuropathy often improves over several months to a few years, though physical therapy is usually needed to regain strength.
Focal Neuropathy (Mononeuropathy)
Focal neuropathy involves sudden damage to a single, specific nerve, leading to weakness or pain in the area that nerve supplies. Unlike peripheral neuropathy, which affects many nerves, focal neuropathy is localized.
Common manifestations include:
- Bell's palsy: Weakness or paralysis on one side of the face.
- Carpal tunnel syndrome: This is the most common type of focal neuropathy, where a nerve in the wrist is compressed. While less than 10% of people with diabetes experience symptoms, about 25% of people with diabetes have some nerve compression at the wrist. Symptoms include numbness, tingling, and weakness in the hand and fingers.
- Double vision or difficulty focusing, if cranial nerves affecting the eyes are involved.
- Pain in a specific area like the shin, foot, lower back, or chest wall.
Many focal neuropathies without nerve entrapment often improve on their own over weeks or months.
Causes, Risk Factors, and Diagnosis
Understanding what drives diabetes neuropática is the first step toward effective management and prevention. It's a complex interplay of factors, but the central theme revolves around the impact of diabetes on your nervous system.
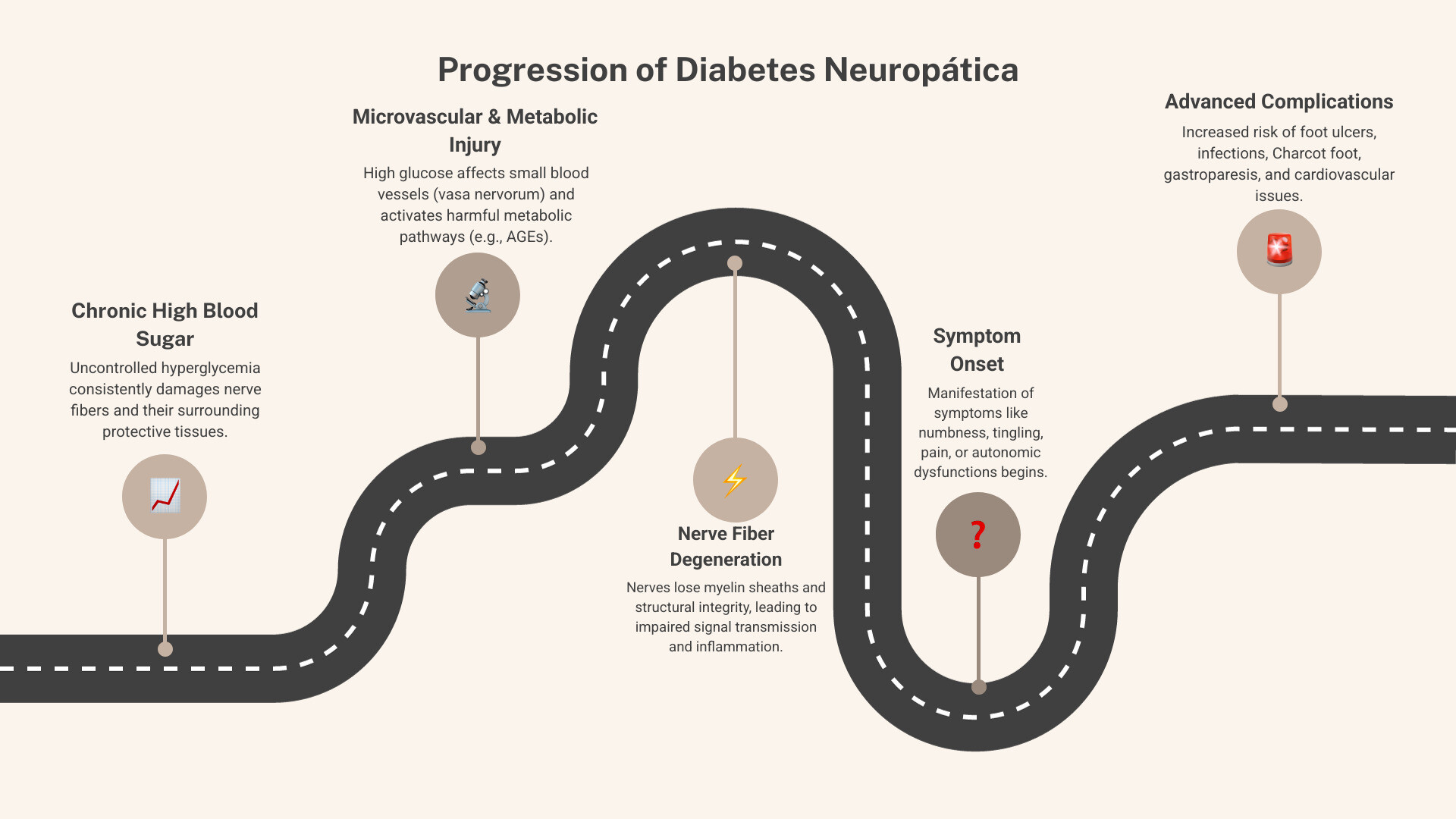
The Root Cause: The Role of Blood Glucose in Diabetes Neuropática
The primary culprit behind diabetes neuropática is chronic high blood sugar, or hyperglycemia. Over time, persistently liftd glucose levels wreak havoc on nerves in several ways:
- Direct nerve damage: High glucose directly injures nerve fibers, impairing their ability to transmit signals effectively.
- Damage to small blood vessels (vasa nervorum): Nerves, like all tissues, require a steady supply of oxygen and nutrients. Chronic high blood sugar damages the tiny blood vessels that nourish the nerves (called vasa nervorum). This leads to a reduction in blood flow, starving the nerves and causing ischemic injury. Think of it like a garden hose slowly getting kinked, reducing water supply to your plants.
- Metabolic pathways: Hyperglycemia activates several damaging metabolic pathways, such as the polyol pathway and the formation of advanced glycation end-products (AGEs). These processes accumulate toxic byproducts within nerve cells, further contributing to their dysfunction and death.
- Inflammation and oxidative stress: High blood sugar triggers inflammation and increases oxidative stress throughout the body, including the nervous system. This creates a hostile environment for nerves, leading to damage.
Research highlights that while hyperglycemia is central, other factors like impaired insulin signaling and dyslipidemia also contribute significantly to the development of diabetes neuropática. There's growing evidence that these primary initiators may converge on a common pathway involving mitochondrial bioenergetics, disrupting the energy production within nerve cells. For a deeper dive into the scientific mechanisms, you can explore detailed scientific research on the mechanisms of neuropathic pain.
Key Risk Factors
While diabetes is the overarching cause, several factors increase your likelihood of developing or worsening diabetes neuropática:
- Poor glucose control: This is arguably the most significant risk factor. The longer and more poorly controlled your blood sugar levels are, the higher your risk.
- Duration of diabetes: The longer you've had diabetes, the greater your chances of developing neuropathy.
- Kidney disease: Diabetic nephropathy (kidney disease) is closely linked to neuropathy, as kidney dysfunction can lead to a buildup of toxins that further damage nerves.
- High blood pressure (hypertension): Hypertension can exacerbate microvascular damage, reducing blood flow to nerves.
- High cholesterol and triglycerides (dyslipidemia): Liftd fat levels in the blood contribute to nerve damage and are increasingly recognized as important factors, especially in type 2 diabetes and metabolic syndrome.
- Obesity: Being overweight or obese increases the risk, partly due to its association with insulin resistance and inflammation.
- Smoking: Smoking constricts blood vessels, further impairing blood flow to nerves and accelerating damage.
- Excessive alcohol consumption: Alcohol itself is neurotoxic and can directly damage nerves, compounding the effects of diabetes.
How Doctors Diagnose the Condition
Diagnosing diabetes neuropática involves a comprehensive approach, as symptoms can sometimes mimic other conditions. Your doctor will typically combine a thorough review of your medical history, a physical exam, and specialized tests.
The diagnostic process often includes:
- Physical and neurological exam: Your doctor will check your reflexes, muscle strength, and sensation (light touch, vibration, temperature, pain) in your arms and legs.
- Comprehensive foot exam: Given the high risk of foot complications, a detailed examination of your feet is crucial. This includes checking for skin changes, calluses, deformities, and signs of poor circulation.
- Monofilament test for sensitivity: A simple, painless test where your doctor uses a soft nylon filament to gently touch specific points on your foot. If you can't feel the monofilament, it indicates a loss of protective sensation, a key sign of peripheral neuropathy.
- Nerve conduction studies (NCS) and Electromyography (EMG): These tests measure how fast electrical signals travel through your nerves and how your muscles respond to these signals. They help assess the function of larger nerve fibers and identify nerve damage.
- Quantitative Sudomotor Axon Reflex Test (QSART) or Sudoscan: These tests measure the function of your sweat glands, which are controlled by small nerve fibers. They are particularly useful for detecting early autonomic and small fiber neuropathy.
- Skin biopsy: A small skin sample is taken (usually from the leg) to measure the density of intraepidermal nerve fibers (IENFD). This is considered a reliable method for diagnosing small fiber neuropathy, which often presents with painful symptoms.
- Blood tests: To rule out other causes of neuropathy, your doctor may check for thyroid problems, kidney disease, or low vitamin B12 levels. Interestingly, metformin use, a common diabetes medication, can sometimes lead to low vitamin B12.
Managing and Treating Diabetes Neuropática
Living with diabetes neuropática can be challenging, but we've seen countless individuals improve their quality of life with a proactive, multi-faceted approach. While there's currently no cure for nerve damage, we can significantly slow its progression and manage symptoms effectively.

The Foundation: Blood Sugar Control
This is the cornerstone of managing diabetes neuropática. Uncontrolled blood sugar is the primary driver of nerve damage, so bringing it into a healthy range is the most critical step to prevent further progression and potentially improve existing symptoms.
- Diet and nutrition: Following a balanced diabetes meal plan is essential. This often involves limiting refined carbohydrates, sugars, and unhealthy fats, and focusing on whole foods, lean proteins, and plenty of fiber.
- Regular exercise: Physical activity helps lower blood sugar, improves circulation, and can even stimulate nerve regeneration. We encourage regular, moderate exercise like walking, swimming, or cycling.
- Adherence to diabetes medications: Taking insulin or other prescribed oral medications as directed by your doctor is vital for maintaining stable blood glucose levels.
- Monitoring HbA1c levels: Regular HbA1c tests provide an average picture of your blood sugar control over the past 2-3 months. Achieving and maintaining your target HbA1c is a powerful way to protect your nerves.
Approaches for Symptom Relief
Since diabetes neuropática can cause significant discomfort, managing symptoms is a key part of improving daily life. These options aim to relieve symptoms, not reverse the nerve damage itself. Always consult your healthcare professional for a personalized treatment plan.
Common pharmacological approaches include:
- Anticonvulsants: Medications like gabapentin and pregabalin, originally developed for seizures, are often first-line treatments for neuropathic pain. They work by calming overactive nerve signals.
- Antidepressants: Certain antidepressants, including tricyclic antidepressants (e.g., amitriptyline, nortriptyline) and serotonin-norepinephrine reuptake inhibitors (SNRIs) like duloxetine and venlafaxine, can be very effective for nerve pain, even in people without depression. They alter brain chemicals involved in pain perception.
- Topical medications: Creams, patches, or sprays containing ingredients like lidocaine or capsaicin can provide localized pain relief.
Supportive therapies also play a crucial role:
- Physical therapy: A physical therapist can help you improve strength, balance, and gait, reducing the risk of falls and making daily activities easier.
- Transcutaneous Electrical Nerve Stimulation (TENS): This therapy uses mild electrical currents delivered through electrodes on the skin to help block pain signals.
- Acupuncture: Some individuals find relief from neuropathic pain through acupuncture, though more research is needed to establish its widespread efficacy.
Topical and Supportive Approaches for Diabetes Neuropática
When it comes to managing the persistent discomfort of diabetes neuropática, especially the burning, tingling, and aching sensations, topical solutions can offer targeted relief without the systemic side effects of oral medications. We understand the need for fast, soothing comfort.
Topical creams designed for nerve pain relief, such as Neuropasil cream with natural ingredients like Menthol and Aloe, work to provide soothing relief right where you need it. Menthol creates a cooling sensation that can distract from pain and desensitize nerve endings, while Aloe is known for its anti-inflammatory and skin-soothing properties. These ingredients can significantly help in managing the daily discomforts of neuropathy. You can explore topical solutions for nerve pain like ours.
Beyond topical applications, several supportive measures can complement your overall treatment plan:
- Physical therapy: As mentioned earlier, physical therapy is invaluable. It focuses on improving muscle strength, flexibility, balance, and gait stability, which are often compromised by neuropathy. This can help prevent falls and maintain independence.
-
Supportive supplements (always consult your healthcare provider):
- Alpha-lipoic acid (ALA): This antioxidant has shown promise in some studies for reducing symptoms of peripheral diabetic neuropathy, particularly when administered intravenously. Oral supplementation may also offer benefits.
- Benfotiamine: A fat-soluble derivative of vitamin B1, benfotiamine has demonstrated efficacy in improving nerve function and reducing neuropathic pain in some individuals with diabetes.
While these supportive approaches can be very helpful, they should always be discussed with your healthcare provider to ensure they are appropriate for your specific condition and won't interact with other medications.
Prevention, Complications, and Quality of Life
The journey with diabetes neuropática is often about proactive management. By understanding how to prevent its onset or progression, recognizing potential complications, and addressing its impact on your well-being, you can maintain a higher quality of life.
Can Diabetic Neuropathy Be Prevented?
While some aspects of diabetes are challenging, preventing or slowing the progression of diabetes neuropática is largely within our control through diligent management of diabetes.
Key preventive strategies include:
- Strict glycemic control: This is the single most important factor. Consistently keeping your blood sugar levels within your target range can prevent nerve damage or significantly slow its worsening. Studies show that tight glucose control can reduce the risk of DPN by a substantial margin, especially in early-diagnosed type 1 diabetes.
- Managing blood pressure and cholesterol: High blood pressure and unhealthy cholesterol levels (dyslipidemia) contribute to vascular damage, which in turn harms nerves. Controlling these factors protects your circulatory system and, consequently, your nerves.
- Maintaining a healthy weight: Obesity is a significant risk factor. Losing excess weight can improve insulin sensitivity and reduce inflammation, both beneficial for nerve health.
- Regular physical activity: Exercise improves blood flow, helps manage blood sugar, and supports overall cardiovascular health, all of which are protective for nerves.
- Quitting smoking: Smoking severely damages blood vessels and directly harms nerves. If you smoke, seeking help to quit smoking is one of the most impactful steps you can take for your nerve health.
- Limiting alcohol: Excessive alcohol consumption is neurotoxic and exacerbates nerve damage in people with diabetes.
Potential Complications of Untreated Neuropathy
Ignoring diabetes neuropática can lead to serious, even life-threatening, complications. We cannot stress enough the importance of early detection and consistent management.
Key complications include:
- Foot ulcers and infections: Loss of sensation in the feet means you might not feel cuts, blisters, or sores. These unnoticed injuries can quickly become infected, leading to severe tissue damage.
- Charcot foot: A severe foot deformity that can develop due to nerve damage. Bones in the foot weaken and fracture, but because of neuropathy, you might not feel the pain, leading to continued walking on the injured foot and further collapse of the arch.
- Risk of amputation: Untreated foot ulcers and infections, especially when combined with poor circulation, are a leading cause of non-traumatic lower-limb amputations.
- Falls due to loss of balance: Peripheral neuropathy impairs balance and coordination, significantly increasing the risk of falls and related injuries like fractures.
- Chronic pain: For many, the constant burning, tingling, or sharp pains can be debilitating, impacting daily activities and quality of life.
- Gastroparesis complications: Delayed stomach emptying can lead to unpredictable blood sugar levels, malnutrition, and severe nausea and vomiting.
- Cardiovascular autonomic neuropathy (CAN): This serious complication affects the nerves controlling your heart and blood vessels, leading to an increased risk of heart attacks, silent heart attacks, and sudden cardiac death. CAN is associated with a significantly higher mortality rate.
Impact on Daily Life and Mental Health
Beyond the physical symptoms, diabetes neuropática profoundly affects a patient's overall quality of life and mental well-being.
- Chronic pain and sleep disturbance: Persistent neuropathic pain can make it difficult to sleep, leading to fatigue, irritability, and a reduced ability to cope with daily stressors.
- Reduced mobility and independence: Weakness, balance problems, and foot complications can limit your ability to walk, drive, or engage in hobbies, leading to a loss of independence.
- Anxiety and social isolation: The constant pain and fear of complications (like falls or amputations) can lead to significant anxiety. Reduced mobility and discomfort may also cause individuals to withdraw from social activities, leading to isolation.
- Depression: The chronic nature of the pain, the limitations it imposes, and the fear of future complications can take a heavy toll on mental health, often leading to depression. It's a cruel cycle, as depression can also worsen pain perception. We recognize the importance of addressing both the physical and emotional aspects of nerve pain.
Frequently Asked Questions about Diabetes Neuropática
Here are some common questions we hear about diabetes neuropática:
Can diabetic neuropathy be reversed?
Nerve damage from diabetes neuropática is often difficult to reverse completely. However, strict blood sugar control can significantly slow or stop its progression and, in some cases, improve symptoms. Early intervention is crucial. While we might not be able to "undo" all damage, we can certainly prevent further deterioration and manage existing symptoms effectively.
How long does it take for diabetic neuropathy to develop?
Diabetes neuropática typically develops gradually over many years. It's not usually an overnight occurrence. The risk increases significantly the longer an individual has diabetes, especially if blood sugar levels are not consistently well-managed. Some people may have mild nerve damage for years before noticing any symptoms.
Is walking good for diabetic neuropathy?
Yes, for many people, regular, moderate exercise like walking is beneficial for diabetes neuropática. It improves blood flow to the extremities, helps control blood sugar levels, and can even reduce pain symptoms. However, wear appropriate, well-fitting footwear and to check your feet daily for any signs of injury, especially if you have reduced sensation. Always consult your doctor or a physical therapist before starting a new exercise regimen to ensure it's safe and custom to your specific condition.
Conclusion: Taking Control of Your Nerve Health
As we've explored, diabetes neuropática is a significant and complex complication of diabetes, but it's not a destiny to passively accept. The cornerstone of prevention and management lies in meticulous blood sugar control, supported by a healthy lifestyle that includes a balanced diet, regular exercise, smoking cessation, and responsible alcohol consumption.
While there's no magic bullet, a combination of medical guidance and supportive therapies can effectively manage symptoms, reduce pain, and drastically improve your quality of life. Proactive care, vigilant self-monitoring (especially for your feet), and open communication with your healthcare team are essential.
For soothing, targeted relief from neuropathic discomfort, we encourage you to explore natural, topical options. Our Neuropasil cream, with its blend of Menthol and Aloe, is designed to provide fast, comforting relief for nerve and muscle pain. We believe in empowering you to take control of your nerve health and live a fuller, more comfortable life. Learn more about Neuropasil's approach to pain relief.
References
- What Is Diabetic Neuropathy? - NIDDK
- Diabetic Neuropathies - StatPearls NCBI Bookshelf
- Advances in Interventional Therapies for Painful Diabetic Neuropathy: A Systematic Review
- Diabetic Neuropathy - Symptoms, Causes - Mayo Clinic
- Diabetic neuropathy - Symptoms, diagnosis and treatment - BMJ Best Practice
- Neuropathic pain - Wikipedia
- Scientific research on the mechanisms of neuropathic pain - NCBI PMC
- Quitting smoking - Smokefree.gov
- Depression - NIMH













