Why Understanding the Sciatic Nerve Matters for Pain Relief
The sciatic nerve is the longest and widest nerve in the body. When it becomes compressed or irritated, it causes sciatica—a painful condition affecting about 40% of people at some point, according to some estimates. Pain from sciatic nerve irritation can range from a mild ache to sharp, burning sensations that make it difficult to walk, sit, or sleep. Understanding this vital nerve is the first step toward relief.
Quick Facts About the Sciatic Nerve:
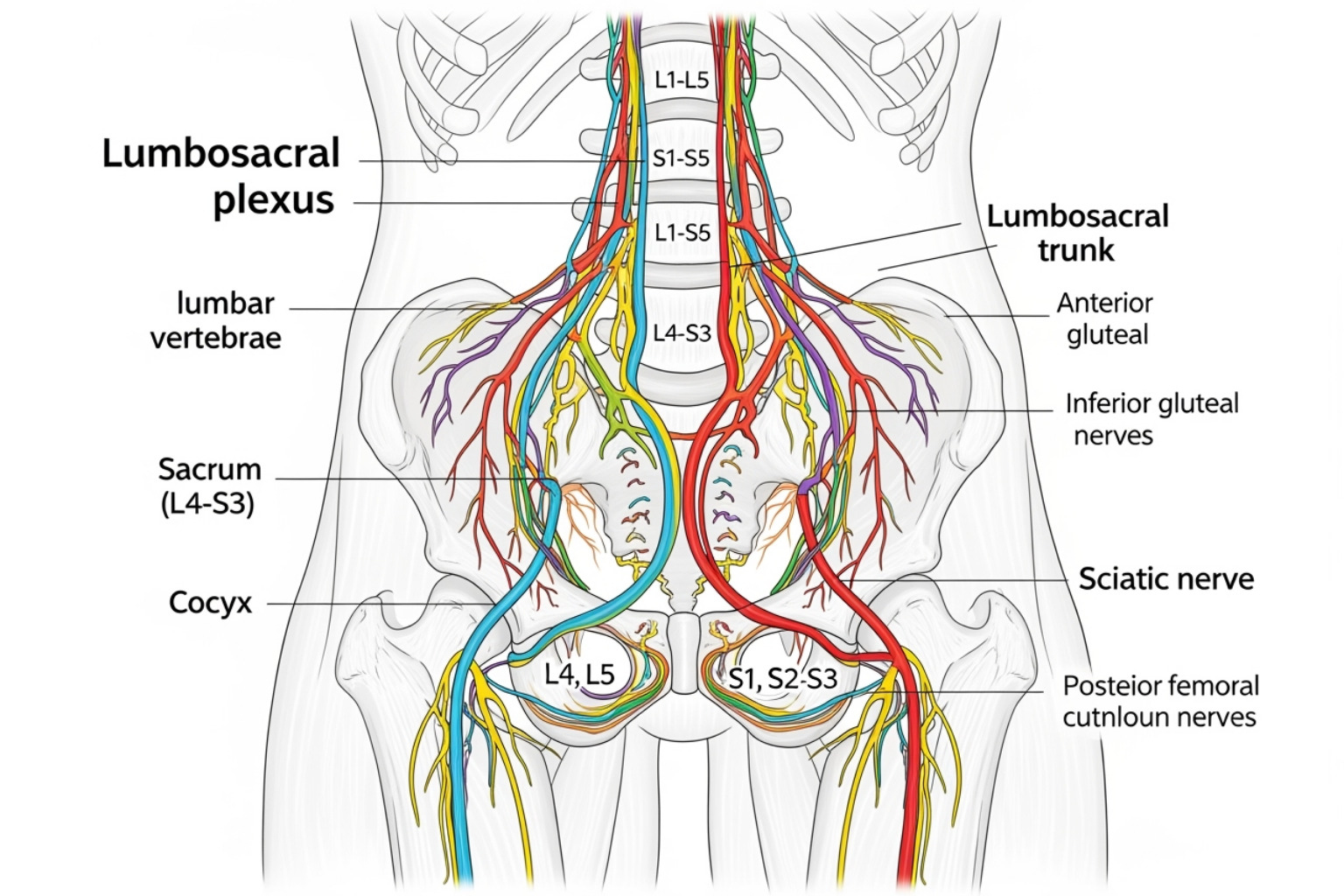
- Location: Starts at spinal nerves L4-S3 in your lower back and extends down the back of each leg to your foot.
- Size: Up to 2 centimeters wide at its thickest point.
- Function: Controls movement and sensation in your legs and feet.
- Common Issue: Sciatica occurs when the nerve is pinched or inflamed, causing radiating pain, numbness, or weakness.
I'm Tony Enrico, and at Neuropasil, we've helped thousands find relief from sciatic nerve pain with our topical nerve pain relief cream. Our mission is to help one million people regain their comfort by 2028, because no one should live at the mercy of pain.
Understanding the Sciatic Nerve and Sciatica
Your body's vast nerve network acts as a messenger system, and the sciatic nerve is a major player. When this nerve gets compressed or irritated, you experience sciatica, turning simple activities like sitting or standing into a challenge. Let's explore what makes this nerve so important and what happens when it causes trouble.
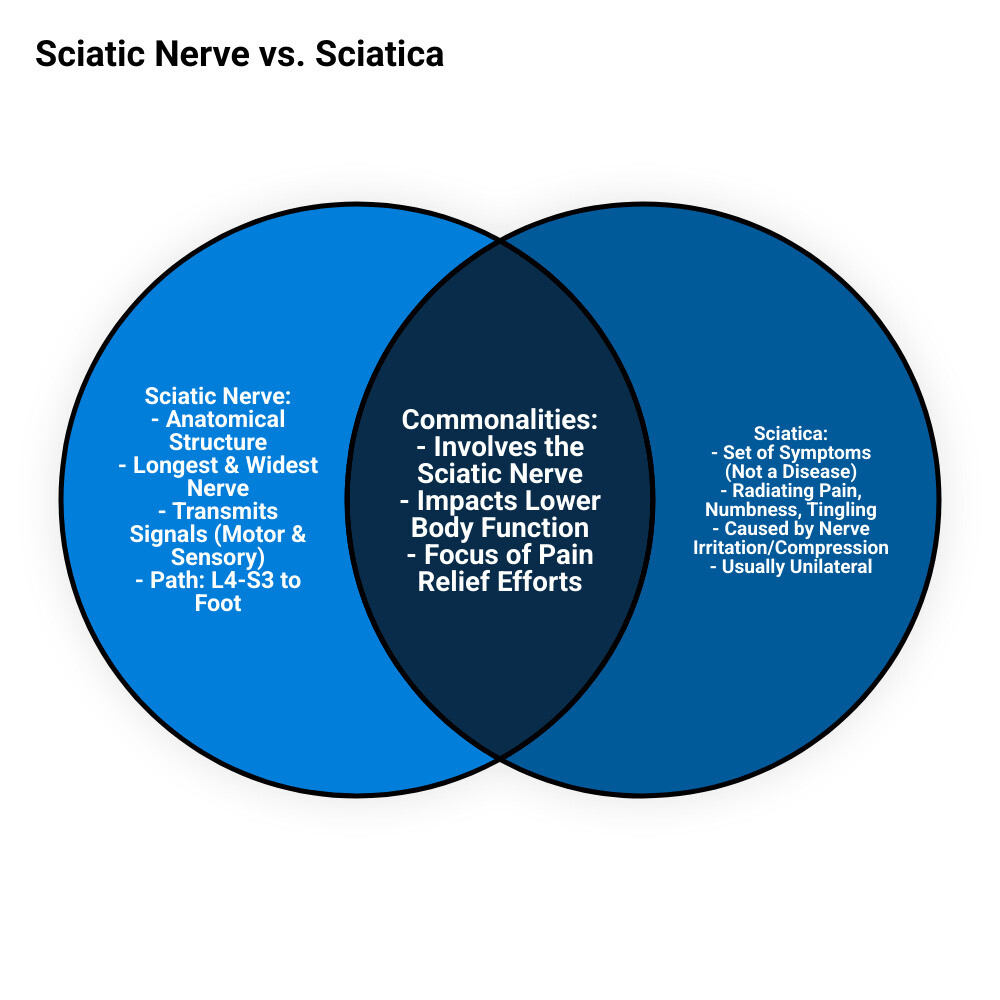
What is the Sciatic Nerve?
The sciatic nerve is the body's main communication cable to the legs. It forms from five nerve roots in the lower back (L4-S3) and runs from the pelvis, through the buttocks, and down the back of each leg. Near the knee, it branches into the tibial and common peroneal nerves, extending to the foot. You can learn more about its path in this anatomy of the sciatic nerve resource.
This nerve has two critical jobs:
- Motor function: It controls the muscles for walking, standing, and bending your knee, ankle, and toes.
- Sensory function: It provides feeling (touch, temperature, pain) to the back of your thigh, lower leg, and the sole of your foot.
What is Sciatica?
It's important to know that sciatica is a symptom, not a disease. It's the term for the pain and neurological issues that occur when the sciatic nerve or its roots are compressed or inflamed. The hallmark of sciatica is radiating pain that follows the nerve's path, typically starting in the lower back and shooting down one leg (unilateral pain). Along with pain, you might feel numbness, tingling, or weakness in the affected leg.
Distinguishing between true sciatica (direct nerve root involvement) and sciatica-like conditions (mimicked symptoms from other issues) is key to finding the right treatment. Our Sciatica Symptoms 101 guide offers a more detailed breakdown.
Causes and Common Symptoms of Sciatica
When that telltale pain shoots down your leg, something is almost always pressing on or irritating your sciatic nerve. Understanding the root cause is the first step toward finding lasting relief.

What Causes Sciatic Nerve Pain?
Most sciatica cases trace back to the lower spine. The most common causes include:
- Herniated Disks: The soft center of a spinal disk pushes out and presses on a nerve root. This is the leading cause of sciatica.
- Spinal Stenosis: A narrowing of the spinal canal that squeezes the nerves.
- Degenerative Changes: Age-related wear and tear, such as bone spurs or degenerative disc disease, can lead to nerve compression.
- Spondylolisthesis: A condition where one vertebra slips over another, pinching a nerve.
Other causes include piriformis syndrome, where a buttock muscle compresses the sciatic nerve, direct injury to the lower back, and pressure from pregnancy. For more on triggers, see our guide: Why Your Sciatic Nerve is Screaming: Causes and Relief.
Common Symptoms and Associated Risk Factors
Sciatica symptoms follow the nerve's path, usually on one side, from the lower back down the leg. Common sensations include:
- Sharp, stabbing, or electric shock-like pain
- A burning sensation
- Numbness or tingling ("pins and needles"), often in the foot or toes
- Muscle weakness in the leg or foot, which can cause a "foot drop"
Pain often worsens with prolonged sitting, coughing, or sneezing.
Several factors increase your risk, including age, obesity, a sedentary lifestyle, occupations that involve heavy lifting or prolonged sitting, diabetes, and smoking, as noted by health authorities like the Mayo Clinic. Learn more about what to look for in our Sciatica Pain Symptoms guide.
Diagnosing and Treating Sciatic Nerve Pain
When sciatic nerve pain disrupts your life, it's encouraging to know that effective diagnostic tools and treatments are available to help you regain comfort and mobility.
How is Sciatica Diagnosed?
Diagnosing sciatica begins with a discussion of your symptoms and medical history, followed by a physical exam. Your doctor will check your reflexes, muscle strength, and watch how you walk. A key diagnostic tool is the straight-leg raise test, where lifting your affected leg while lying down reproduces the pain, strongly suggesting sciatica.
If symptoms are severe or persistent, imaging tests may be ordered. While X-rays can show bone issues, an MRI is the gold standard for viewing soft tissues like herniated disks and nerves. A CT scan or EMG (which measures nerve electrical activity) may also be used to pinpoint the problem.
Conventional Treatment and Relief Strategies
The good news is that 80-90% of people with sciatica improve without surgery, often within several weeks. Treatment focuses on reducing pain and restoring mobility. Conservative strategies are the first line of defense:
- Activity Modification: Avoid activities that worsen pain, but stay gently active. Light walking and stretching are often beneficial.
- Medications: Over-the-counter NSAIDs (like ibuprofen) can reduce pain and inflammation. Your doctor may also prescribe muscle relaxers or other pain relievers.
- Physical Therapy: A physical therapist can design a program to strengthen your core, improve flexibility, and teach you proper body mechanics to protect your back.
These strategies are covered in-depth in The Definitive Guide to Relieving Sciatic Nerve Pain.
Topical Solutions for Fast Relief
For immediate, targeted relief, a nerve pain relief cream can be an invaluable tool. Unlike oral medications, topical solutions work directly where you hurt.
Our Neuropasil cream is formulated with powerful natural ingredients to soothe sciatic nerve pain:
- Menthol provides a cooling sensation that distracts pain receptors.
- Aloe calms inflammation and soothes irritated tissues.
- Urea helps the active ingredients penetrate deeply for maximum effect.
Applying our muscle pain relief cream to your lower back, buttocks, or down your leg gives you control over your pain. It's a strategy many of our customers rely on for sciatica, neuropathy, and general muscle soreness. For more on this approach, see our guides: Fast Track to Comfort: Immediate Solutions for Sciatica Pain and The Ultimate Guide to Best Cream for Sciatica Pain.
Prevention, Complications, and When to Seek Help
While you can't always prevent sciatica, you can take meaningful steps to protect your sciatic nerve and reduce your risk. It's also vital to know what complications to watch for and when to seek medical help.
Can Sciatica Be Prevented?
While some risk factors like age are unavoidable, you can take proactive steps to protect your sciatic nerve. Prevention is an investment in your future comfort.
- Exercise Regularly: Keep your back muscles strong and flexible with activities like walking, swimming, or cycling.
- Strengthen Your Core: Strong abdominal and back muscles support your spine. Yoga and Pilates are excellent for this.
- Maintain Good Posture: Sit with your back supported and feet flat on the floor. When standing, keep your weight evenly distributed. See these tips for maintaining good posture.
- Lift Smart: Bend at your knees, not your waist, and keep heavy objects close to your body.
- Manage Your Weight: Extra weight adds stress to your spine.
- Quit Smoking: Nicotine impairs blood flow to your spinal disks, accelerating degeneration.
Potential Complications and Impact on Daily Life
While most cases resolve, untreated or severe sciatica can lead to complications like permanent nerve damage, foot drop (weakness that causes the foot to drag), or a loss of feeling in the affected leg. The impact on daily life can be significant, making it hard to walk, sit, or sleep comfortably.
When to See a Doctor for Sciatica
Mild sciatica often improves with self-care, but you should see a doctor if your pain is severe, lasts longer than a week, or keeps getting worse.
Seek emergency medical care immediately for any of the following symptoms, as they can signal a serious condition called Cauda Equina Syndrome, a medical emergency:
- Sudden, severe weakness or numbness in one or both legs
- Loss of bladder or bowel control
- Numbness in your "saddle" area (inner thighs, buttocks, back of legs)
- Pain following a violent injury (like a car accident)
These are medical emergencies that require immediate attention to prevent permanent damage.
Frequently Asked Questions about Sciatica
When you're dealing with sciatic nerve pain, questions are natural. Here are clear, helpful answers to some of the most common concerns.
Can sciatica affect both legs at the same time?
Yes, though it's uncommon. Sciatica usually affects only one leg. When it occurs in both legs (bilateral sciatica), it often signals a more significant central spinal issue, like a large herniated disk or severe spinal stenosis, and requires prompt medical evaluation. If you have symptoms in both legs, see a doctor promptly.
How long does it take for sciatica to go away?
The timeline varies. Acute sciatica often resolves within 4 to 6 weeks with conservative care. Chronic sciatica (lasting over three months) can be more persistent. However, the outlook is positive: 80% to 90% of people get better without surgery.
Is walking good for sciatica?
Yes, gentle walking is highly beneficial. It improves blood flow to reduce inflammation, triggers the release of natural painkillers (endorphins), and prevents muscle stiffness. Start with short, comfortable walks and listen to your body. If pain increases, scale back. The goal is consistent, gentle movement.
Conclusion
Understanding the sciatic nerve is the first step to managing the pain of sciatica. While it can be debilitating, most people find relief with a proactive approach.
By staying gently active, practicing good posture, and strengthening your core, you can support your spine and ease pressure on the nerve. For flare-ups, physical therapy, activity modification, and medical treatments can guide your recovery.
When you need fast, targeted relief, a topical cream can make all the difference. Neuropasil's formula, with Menthol, Aloe, and Urea, delivers soothing comfort directly to the source of your pain, helping you manage sciatica, neuropathy, and muscle aches.
My name is Tony Enrico, and our mission at Neuropasil is to help one million people find relief from pain by 2028. You don't have to live at the mercy of pain. By taking informed action, you can reclaim your comfort and quality of life.
Ready to take the next step? Explore our blog for more strategies on managing nerve pain.
References
The information in this article was sourced from the following trusted medical and research institutions. We encourage you to explore them for further reading.
- Mayo Clinic: Sciatica - Symptoms and causes - Mayo Clinic
- Cleveland Clinic: Sciatica: What It Is, Causes, Symptoms, Treatment & Pain Relief - Cleveland Clinic
- StatPearls (NCBI): Anatomy, Sciatic Nerve - StatPearls - NCBI Bookshelf
- StatPearls (NCBI): Sciatica - StatPearls - NCBI Bookshelf
- Cleveland Clinic: Health Effects of Poor Posture













