Understanding Arthritis Pain: Your Path to Relief
Arthritis pain relief starts with understanding what you're up against. If you're dealing with joint pain that makes simple tasks feel impossible, you're not alone. About 25% of adults in the U.S. have some form of arthritis, making it a leading cause of pain and limited mobility.
Arthritis is the inflammation of joints, often caused by the breakdown of cartilage. The most common type is osteoarthritis (OA), a degenerative disease. Rheumatoid arthritis (RA) is an autoimmune condition where your body attacks its own joints.
While arthritis technically means "joint inflammation," most people will tell you the pain is the most bothersome symptom. That grinding, aching, or sharp pain can steal your mobility and your quality of life.
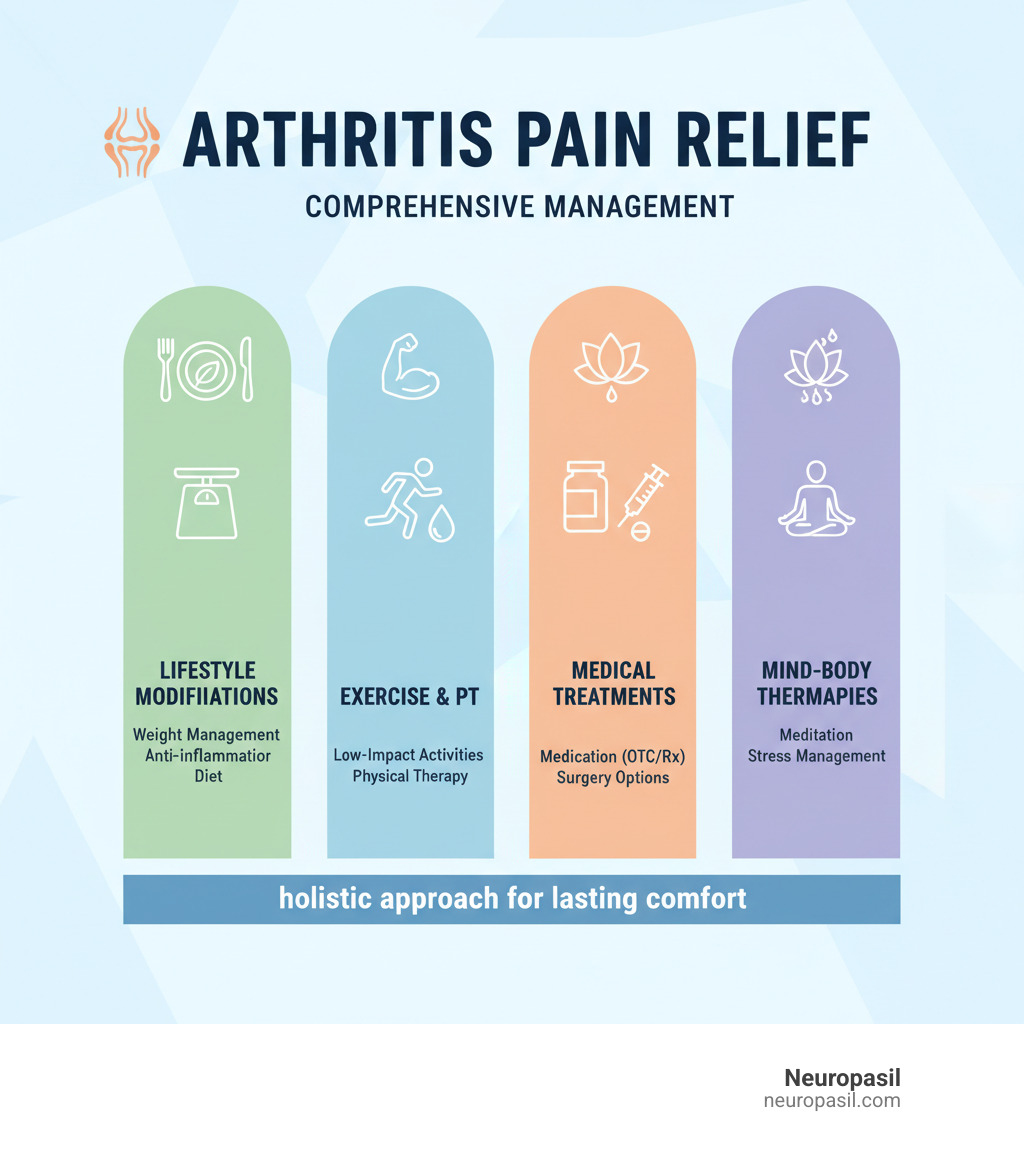
The good news is that effective arthritis pain relief isn't just about popping pills. The most successful approach combines lifestyle changes, smart exercise, medical treatments, and mind-body techniques. You don't have to choose just one path—the best results come from using multiple strategies together.
Foundational Lifestyle Changes for Arthritis Pain Relief
The journey to arthritis pain relief begins with your daily habits. These lifestyle changes are the building blocks for managing your pain and protecting your joints for years to come.
The Critical Role of Weight Management
Every extra pound you carry puts about four to five pounds of pressure on your knees. The good news? You don't need to lose a massive amount of weight to feel a difference. Studies show that losing just 5-10% of your body weight can significantly reduce joint pain and slow cartilage damage. For someone who weighs 200 pounds, that's only 10-20 pounds. Weight loss also reduces inflammation throughout your body, as fat tissue produces inflammatory chemicals.
Eating to Beat Inflammation
Your kitchen can be a powerful weapon against arthritis pain. An anti-inflammatory diet focuses on foods that naturally calm inflammation in your body.
- Fatty fish like salmon, mackerel, and sardines are packed with omega-3 fatty acids.
- Colorful vegetables and fruits like leafy greens and berries are loaded with antioxidants.
- Extra virgin olive oil contains compounds that work similarly to ibuprofen.
- Turmeric's active ingredient, curcumin, has been shown to be as effective as ibuprofen for knee pain in some studies.
On the other hand, try to limit processed foods, excess sugar, and refined carbohydrates, as they can promote inflammation. For more detailed guidance, check out resources from Harvard Health on anti-inflammatory diets and Johns Hopkins' nutrition guide for rheumatoid arthritis.
Why Quitting Smoking is Non-Negotiable
If you smoke, quitting is one of the most important things you can do for your joints. The toxins in cigarette smoke damage connective tissues, reduce blood flow to your joints, and can even make you feel pain more intensely. E-cigarettes are not a safe alternative, as they may also contain harmful chemicals. Talk to your doctor about resources to help you quit.

Movement as Medicine: Exercise and Physical Therapies
When your joints hurt, the last thing you may want to do is move. However, movement is medicine for arthritis. The key is finding the right balance between activity and rest. Gentle, regular movement strengthens the muscles that support your joints, improving mobility and reducing stiffness.
Effective Exercises for Arthritis Pain Relief
Regular, low-impact exercise is one of the most effective non-drug treatments for reducing arthritis pain. It can also boost your mood and improve sleep.
- Water exercises and swimming: The buoyancy of water supports your body, taking the pressure off your joints while you get a great workout.
- Walking: A simple and effective exercise. Start with short walks on soft surfaces and gradually increase your time and distance.
- Cycling: Whether on a stationary bike or outdoors, cycling provides a smooth, joint-friendly workout.
- Stretching and range-of-motion exercises: Just 10 minutes of gentle stretching each morning can significantly improve flexibility and reduce stiffness.
- Gentle yoga and Tai Chi: These practices combine stretching with strengthening and balance, while also helping to manage stress.
The golden rule is to balance activity with rest and never push through sharp pain. A physical therapist can help create a personalized plan for you. You can find more exercise ideas on the American Association of Hip and Knee Surgeons website.

Exercises to Approach with Caution
Not all exercises are created equal for those with arthritis. High-impact activities like running and jumping can put too much stress on your joints. Repetitive motion sports like tennis can also be problematic. If an exercise causes increased pain or swelling that lasts for more than an hour or two, it's a sign to modify your routine or try something else. Always consult with a doctor or physical therapist before starting a new exercise program.
Supportive Therapies and Assistive Devices
Exercise is just one piece of the puzzle. Other therapies and tools can also provide significant arthritis pain relief.
- Physical Therapy (PT): A physical therapist can design a custom program to strengthen muscles, improve joint function, and teach you how to move in ways that reduce stress on your joints.
- Occupational Therapy (OT): An occupational therapist helps you adapt daily tasks and your environment, suggesting tools and techniques to make activities like cooking or dressing easier.
- Braces and Splints: These can provide stability and take some of the load off damaged joints, especially for knees and hands.
- Walking Aids: Canes and walkers can significantly reduce the load on painful hips and knees.
- Orthotics: Custom shoe inserts can help distribute weight more evenly and improve your balance.
- Hot and Cold Therapy: Applying heat can soothe stiff joints, while cold packs can reduce swelling and numb acute pain.
Medical Treatments: From Medications to Surgery
When lifestyle changes and exercise aren't enough to provide the arthritis pain relief you need, it's time to explore medical treatments. Working with a healthcare professional, like a rheumatologist or orthopedic surgeon, is key to finding the right approach for your specific type of arthritis, whether it's osteoarthritis (OA) or rheumatoid arthritis (RA).

Medications for Arthritis Pain Relief
Medications are a cornerstone of arthritis management, helping to control pain and inflammation.
- Over-the-counter (OTC) medications: These are often the first line of defense. Acetaminophen (Tylenol) can help with mild to moderate pain. NSAIDs like ibuprofen and naproxen tackle both pain and inflammation but should be used cautiously due to potential side effects with long-term use.
- Prescription medications: For more severe symptoms, your doctor might prescribe stronger options. DMARDs (Disease-Modifying Antirheumatic Drugs) and Biologics are used for inflammatory arthritis like RA to slow disease progression.
- Topical treatments: Creams, gels, and patches can deliver pain relief directly to the affected joint with fewer systemic side effects. Options include capsaicin cream, diclofenac gel, and lidocaine patches.
| Medication Type | Best For | Pros | Cons |
|---|---|---|---|
| Over-the-Counter | Mild to moderate pain, occasional flares | Easy access, lower cost | Potential side effects with long-term use |
| Prescription | Moderate to severe symptoms, disease modification | More powerful, can slow disease progression | Higher cost, more side effects, requires monitoring |
| Topical | Localized pain, those who can't take oral meds | Targeted relief, fewer systemic side effects | Can cause skin irritation |
The Role of Injections
For more targeted relief, your doctor might recommend joint injections.
- Corticosteroid injections (cortisone shots) deliver a powerful anti-inflammatory directly into the joint, providing rapid relief that can last for months. They are typically limited to a few times per year per joint.
- Hyaluronic acid injections ("gel shots") are used to lubricate the joint, primarily for knee osteoarthritis. They may offer longer-lasting relief than cortisone for some people.
Injections offer fast, targeted relief but carry small risks, such as temporary pain or, rarely, infection.
When is Surgery the Right Option?
Surgery is generally considered a last resort when other treatments have failed and pain significantly impacts your quality of life.
- Joint replacement (arthroplasty) is a highly successful procedure for hips and knees, offering dramatic pain relief and improved mobility.
- Joint fusion (arthrodesis) can provide stability and pain relief for smaller joints, like those in the hands and feet, by fusing the bones together.
- Osteotomy involves realigning bones to shift weight off a damaged part of a joint, often to delay a full joint replacement in younger patients.
If your arthritis pain prevents you from doing the things you love, it may be time to discuss surgical options with an orthopedic surgeon.
Exploring Complementary and Mind-Body Approaches
Living with arthritis pain isn't just a physical battle; it's an emotional one, too. Stress and anxiety can worsen pain, creating a vicious cycle. Complementary and mind-body techniques can help you break this cycle by changing your relationship with pain and activating your body's natural healing responses.
Using the Mind-Body Connection
- Mindfulness and Meditation: These practices teach you to observe pain without judgment, which can reduce its intensity and your emotional reaction to it. Even a few minutes a day can help. The Arthritis Foundation offers guidance on different meditation styles.
- Deep Breathing: When pain strikes, we often hold our breath or breathe shallowly, increasing stress. Slow, deep breaths can activate your body's relaxation response and ease tension.
- Cognitive Behavioral Therapy (CBT): This form of therapy helps you identify and reframe negative thought patterns about your pain, which can significantly improve your ability to cope.

Alternative Therapies and Supplements
Many people find relief by adding alternative therapies to their treatment plan. Always discuss these with your doctor to ensure they are safe for you.
- Acupuncture: This ancient practice involves inserting thin needles into specific points on the body. Research suggests it can help manage arthritis pain, possibly by releasing natural pain-relieving chemicals called endorphins.
- Massage Therapy: Massage can improve circulation, reduce muscle tension around sore joints, and provide a sense of well-being. Even simple self-massage can be beneficial.
-
Nutritional Supplements: While the evidence varies, some supplements are popular for arthritis relief.
- Turmeric: Contains curcumin, a powerful anti-inflammatory.
- Omega-3 Fatty Acids: Found in fish oil, these can help reduce inflammation, especially in rheumatoid arthritis.
- Glucosamine and Chondroitin: Though research is mixed, some individuals report benefits.
- SAM-e: A compound that may help with both pain and mood.
Because supplements are not regulated like medications, it's important to choose high-quality products. The Arthritis Foundation provides reliable information on this topic.
Frequently Asked Questions about Arthritis Pain
Living with arthritis can bring up many questions. Here are answers to some of the most common ones we hear.
How much weight do I need to lose to feel a difference in my joint pain?
You don't need to achieve a drastic weight loss to feel better. Research shows that losing just 5-10% of your body weight can significantly reduce stress on your joints and decrease pain, especially in the knees and hips. For every pound you lose, you reduce the load on your knees by about four pounds.
Can exercise make my arthritis worse?
This is a common fear, but the right kind of exercise is actually one of the best non-drug treatments for arthritis. While high-impact activities like running can be jarring, low-impact exercises are highly beneficial. Activities like swimming, cycling, and walking strengthen the muscles that support your joints, improving stability and reducing pain. The key is to listen to your body and avoid pushing through sharp pain.
What is the fastest way to relieve an arthritis flare-up?
When you're in the middle of a painful flare-up, you want relief quickly. Here are a few strategies:
- Cold Therapy: For swollen, inflamed joints, apply a cold pack wrapped in a towel for 15-20 minutes to reduce swelling and numb the area.
- Heat Therapy: For stiffness and aching without significant swelling, a warm bath or heating pad can help relax muscles and ease discomfort.
- Over-the-Counter (OTC) Medications: Anti-inflammatory drugs like ibuprofen or naproxen can provide relatively fast relief from both pain and inflammation.
These are short-term solutions. If flare-ups are frequent or severe, it's important to consult your doctor to adjust your long-term management plan.
Conclusion: Creating Your Personalized Pain Management Plan
Finding lasting arthritis pain relief is a journey, not a destination. It requires a comprehensive approach that combines lifestyle adjustments, targeted exercise, medical treatments, and mind-body practices.
Start with the fundamentals: maintaining a healthy weight and adopting an anti-inflammatory diet can significantly reduce the burden on your joints. Accept movement as medicine, focusing on low-impact activities like swimming or walking to build strength and flexibility without causing further strain.
Work closely with your healthcare team to find the right medical treatments for you, whether it's over-the-counter aids, prescription medications, or injections. And don't forget the power of your mind—techniques like meditation and deep breathing can change your perception of pain and improve your overall quality of life.
The most effective plan is a personalized one. You are the most important member of your healthcare team. By staying informed, communicating with your doctors, and being proactive, you can find the right combination of strategies to manage your arthritis and live a fuller, more active life.
As part of a comprehensive natural strategy, consider exploring additional resources that might complement your pain management plan. You can learn more about natural approaches in our guide Managing Arthritis Pain: A Guide to Long-Lasting Relief or find how natural solutions like Neuropasil might fit into your overall wellness routine by visiting Find natural solutions for pain relief with Neuropasil.
Medical Treatments: From Medications to Surgery
When lifestyle adjustments and physical therapies aren't enough to manage arthritis pain relief, medical interventions become necessary. It's crucial to work closely with a healthcare professional, such as a rheumatologist or orthopaedic surgeon, to determine the most appropriate treatment path for your specific type of arthritis and its severity. Treatments for osteoarthritis (OA) often differ from those for inflammatory conditions like rheumatoid arthritis (RA).
Medications for Arthritis Pain Relief
Medications play a vital role in controlling pain, reducing inflammation, and, in some cases, slowing disease progression. Always discuss medication use with a healthcare professional to ensure safety and appropriateness.
- Over-the-counter (OTC): Acetaminophen for pain; NSAIDs (ibuprofen, naproxen) for pain and inflammation. Use the lowest effective dose and be mindful of stomach, kidney, and heart risks.
- Prescription: DMARDs, biologics, and JAK inhibitors for inflammatory arthritis (like RA) to slow disease activity. These require monitoring for side effects and infections.
- Topical: Capsaicin, diclofenac gel, and lidocaine patches can ease localized joint pain with fewer systemic effects.
In some cases, injections (such as corticosteroids or hyaluronic acid for knees) offer targeted relief. When pain and disability remain severe despite other treatments, surgery (e.g., joint replacement, fusion, or osteotomy) may be appropriate after discussion with your surgeon.
Exploring Complementary and Mind-Body Approaches
Living with arthritis can feel like you're fighting a battle on multiple fronts. The pain isn't just physical - it affects your mood, your sleep, your relationships, and your overall quality of life. That's why the most effective approach to arthritis pain relief goes beyond just treating your joints. It recognizes that your mind and body are deeply connected, and that emotional well-being plays a crucial role in how you experience pain.
When stress and worry rise, pain often feels worse. Mind-body techniques help break this cycle by lowering stress responses and improving how your brain processes pain signals.
Using the Mind-Body Connection
- Mindfulness and meditation: Practicing daily—even briefly—can reduce perceived pain and stress. The Types of Meditation for Arthritis from the Arthritis Foundation can help you get started.
- Deep breathing: Slow, diaphragmatic breathing (for example, inhale 4, hold 4, exhale 6) activates relaxation and eases muscle tension.
- Progressive muscle relaxation: Systematically tense and release muscle groups to reduce hidden tension.
- Cognitive Behavioral Therapy (CBT): Reframes unhelpful thoughts about pain and builds coping skills; often delivered by therapists trained in pain management.
- Guided imagery/hypnosis: Directs attention toward calming sensations and away from pain signals.

Alternative Therapies and Supplements
- Acupuncture: May trigger the release of natural pain-relieving chemicals. See the Arthritis Foundation's information on acupuncture and consult qualified practitioners.
- Massage therapy: Can improve circulation, reduce muscle tension, and promote relaxation; self-massage techniques can help between sessions.
- Nutritional supplements: Discuss with your doctor to avoid interactions and choose quality products. Options people often consider include:
- Turmeric (curcumin)
- Omega-3 fatty acids (fish oil)
- Glucosamine and chondroitin (mixed evidence)
- SAM-e
- CBD/medical marijuana (where legal; evidence evolving)
The Popular Supplements for Arthritis from the Arthritis Foundation provides helpful guidance.
Frequently Asked Questions about Arthritis Pain
How much weight do I need to lose to feel a difference in my joint pain?
Even losing 5–10% of your body weight can noticeably reduce stress on weight-bearing joints and ease pain—every pound lost removes roughly four to five pounds of load from your knees.
Can exercise make my arthritis worse?
The right exercise helps. Prioritize low-impact activities (walking, swimming, cycling, gentle yoga), build up gradually, and avoid pushing through sharp pain. If symptoms flare or persist, consult a physical therapist for a custom plan.
What is the fastest way to relieve an arthritis flare-up?
Use cold packs 15–20 minutes for swollen, inflamed joints; use heat for stiffness without significant swelling. Short-term use of OTC anti-inflammatories (like ibuprofen or naproxen) can help—ask your doctor about safe dosing and frequency.
Conclusion: Creating Your Personalized Pain Management Plan
Lasting arthritis pain relief comes from combining strategies: weight management and an anti-inflammatory diet, regular low-impact movement, appropriate medical care, and mind-body techniques to lower stress and reframe pain.
Work with your healthcare team to adjust treatments as your needs change, and track what helps you most. Small, consistent steps add up.
As part of a comprehensive natural strategy, consider exploring additional resources that might complement your pain management plan. You can learn more about natural approaches in our guide Managing Arthritis Pain: A Guide to Long-Lasting Relief or find how natural solutions like Neuropasil might fit into your overall wellness routine by visiting Find natural solutions for pain relief with Neuropasil.
You've got this—progress, not perfection.













