What You Need to Know About Lower Back Nerve Pain
Lower back nerve pain is a sharp, shooting, or burning sensation traveling from your lower back down your leg. Unlike muscle soreness, this pain follows a specific nerve path, often feeling like an electric shock or pins and needles.
Quick Answer:
- What it is: Pain from irritation or compression of nerve roots in your lower back (sciatica or lumbar radiculopathy).
- Common causes: Herniated disc, spinal stenosis, bone spurs, or injury.
- Key symptoms: Sharp pain radiating down the leg, numbness, tingling, or weakness.
- Treatment: Most cases (80-90%) improve within 4-6 weeks with conservative care like rest, ice/heat, gentle movement, and topical relief.
- When to see a doctor: Immediately if you lose bowel/bladder control, have severe leg weakness, or pain after trauma.
This is a common experience. Eight in 10 people will have lower back pain in their lifetime, and up to 4 in 10 will develop sciatica, the most frequent type of lower back nerve pain.
Knowing the difference is key. Muscle pain is typically localized, while nerve pain travels from the back down the leg. This occurs when compressed or irritated spinal nerves send pain signals along their pathway.
The good news is that most cases resolve with self-care. Effective symptom management can help while your body heals. Identifying the cause of your pain, whether acute or chronic, is the first step to relief.
I'm Tony Enrico, creator of Neuropasil. I developed our products after seeing how lower back nerve pain impacted people's lives. Through research and collaboration with experts, my goal is to help people find natural, effective relief and regain their freedom of movement.
Understanding Lower Back Nerve Pain: Symptoms and Causes
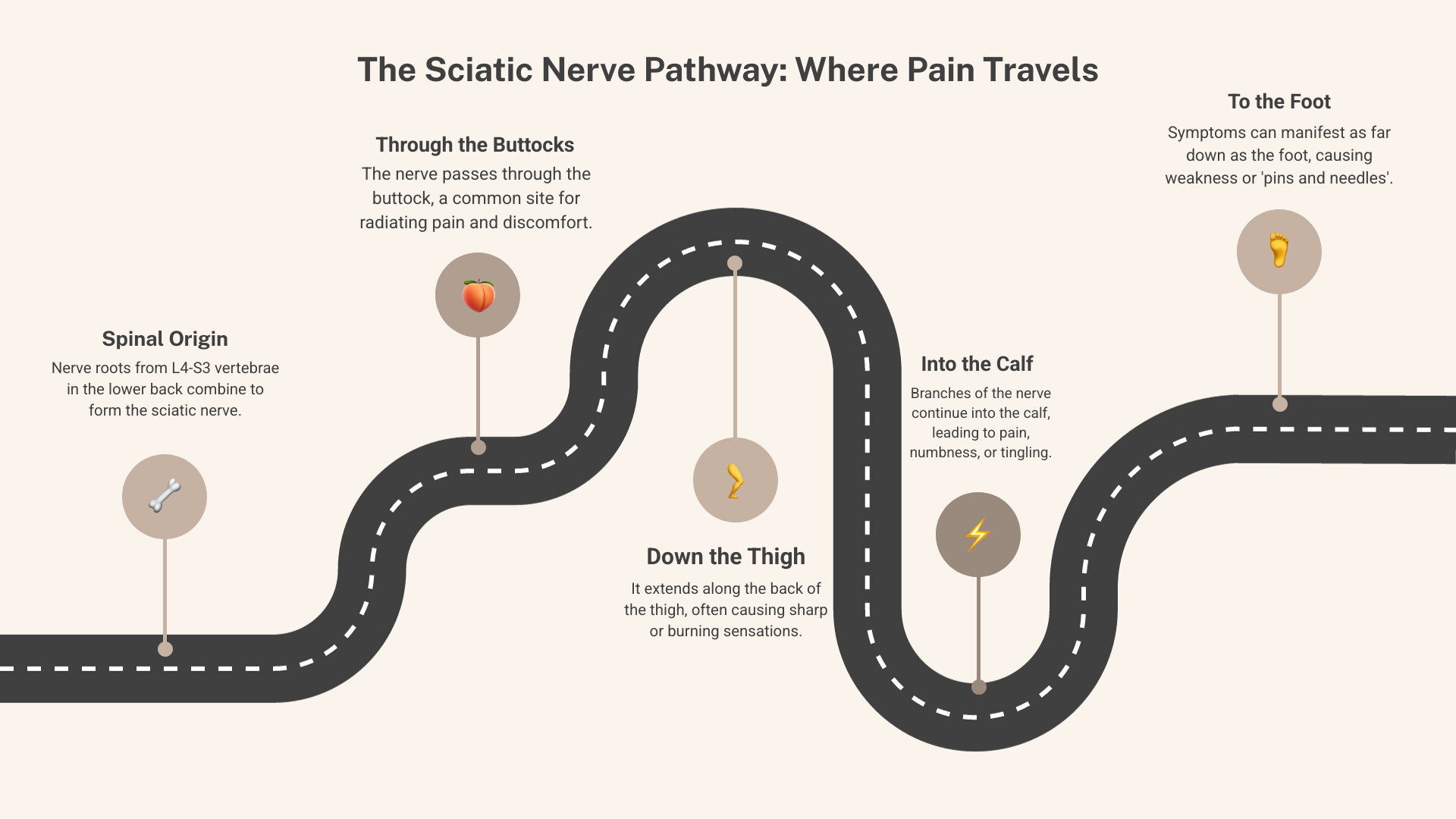
Lower back nerve pain, often called sciatica or lumbar radiculopathy, refers to pain from an irritated or pinched nerve root in the lumbar spine. Unlike a general ache, this pain travels along a specific nerve path. When a spinal nerve is compressed or irritated, it can cause pain, numbness, or tingling anywhere along its path. This is known as radicular pain, which travels down the leg, whereas muscular (axial) pain typically stays in the lower back.
This is a common issue. About 8 out of 10 people will experience lower back pain, and up to 4 out of 10 will suffer from sciatica, the most prevalent type of lower back nerve pain.
Sciatica vs. General Back Pain
Distinguishing between general back pain and sciatica is key to finding relief. General pain is often a dull ache localized in the back, while sciatica is a sharp, burning, or electric shock-like pain that radiates down the leg. Numbness, tingling, and weakness in the leg or foot are also hallmark signs of nerve involvement, which are not typical of muscular back pain.
Here's a quick side-by-side comparison to make it even clearer:
| Feature | General Lower Back Pain | Lower Back Nerve Pain (Sciatica/Lumbar Radiculopathy) |
|---|---|---|
| Pain Location | Primarily in the lower back; may extend to buttocks. | Radiates from lower back down the leg (thigh, calf, foot). |
| Pain Character | Dull ache, stiffness, localized sharp pain, muscle spasm. | Sharp, shooting, burning, electric shock-like sensation. |
| Numbness/Tingling | Rare, unless underlying nerve issue. | Common in the leg, foot, or toes. |
| Weakness | Less common, usually due to muscle inhibition. | Possible in leg or foot muscles (e.g., foot drop). |
| Movement Impact | Pain with specific movements, stiffness. | Pain worsens with sitting, coughing, sneezing, bending. |
Common Causes of Nerve Compression
Several conditions can put pressure on the nerves in your lower back:
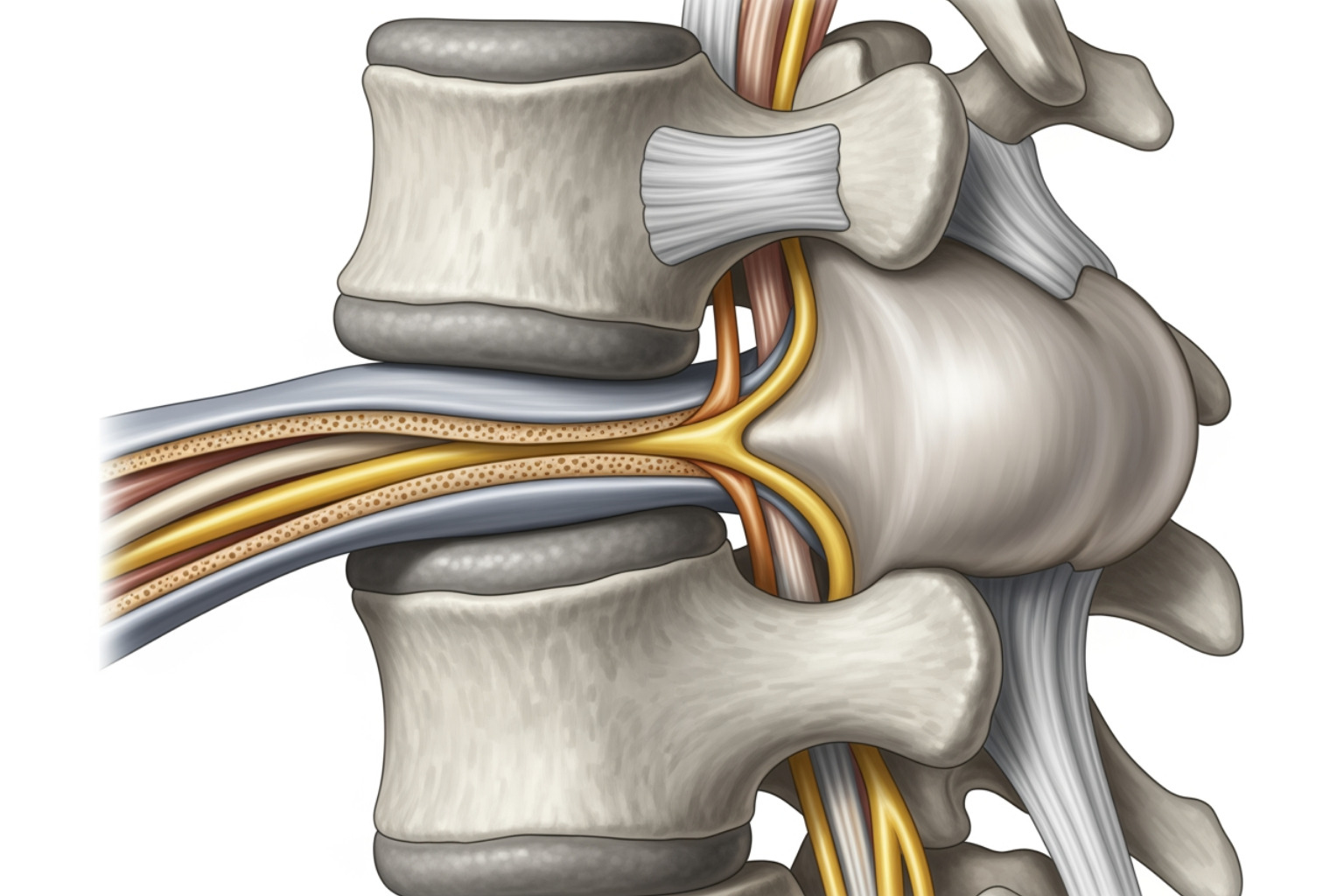
Herniated Disc: The most common cause. The soft center of a spinal disc pushes out and presses on a nerve root. It's most common in people aged 30 to 50.
Spinal Stenosis: A narrowing of the spaces within your spine, which can put pressure on the spinal cord and nerves. It often develops with age. Learn more from the Mayo Clinic.
Spondylolisthesis: This happens when one vertebra slips forward over the one below it, pinching nerve roots.
Bone Spurs (Osteophytes): Extra bone growth, common with aging, can narrow the spinal canal and compress nerves.
Piriformis Syndrome: A less common cause where a tight or spasming piriformis muscle in the buttock irritates the nearby sciatic nerve.
Trauma or Injury: Falls, accidents, or improper heavy lifting can damage spinal structures and lead to nerve compression.
Recognizing the Symptoms of Lower Back Nerve Pain
Tuning into your symptoms is crucial. Key signs of lower back nerve pain include:
- Sharp, shooting, or burning pain: An intense sensation that travels in a clear path.
- Pain radiating from the buttock down the leg: Often affecting only one side, this pain can extend to the thigh, calf, or foot.
- Numbness or a "pins-and-needles" sensation: A classic sign of nerve irritation, like a limb "falling asleep."
- Muscle weakness or foot drop: Significant nerve compression can affect muscle function, causing weakness or difficulty lifting the front of your foot.
- Pain worsens with sitting, coughing, or sneezing: These actions increase pressure in the spinal canal, aggravating nerve pain.
Diagnosis and When to See a Doctor
Diagnosing lower back nerve pain is the first step toward relief. A healthcare professional will typically start with a review of your medical history and symptoms, followed by a physical examination. During the exam, your doctor may use the straight leg raise test, where lifting your leg while you lie down reproduces the pain, indicating nerve irritation. They will also check your reflexes, muscle strength, and sensation to identify which nerves are affected.
To get a clearer picture, imaging tests may be used:
- X-rays show bone issues like spurs or alignment problems but not soft tissues.
- An MRI (Magnetic Resonance Imaging) provides a detailed view of soft tissues, showing herniated discs, stenosis, and nerve compression.
- CT scans (Computed Tomography) offer detailed images of bone structures and can also reveal disc problems.
- Electromyography (EMG) and Nerve Conduction Studies (NCS) measure nerve and muscle electrical activity to pinpoint nerve damage and its severity.

The Diagnostic Process
The diagnostic process involves consulting a healthcare professional and describing your symptoms in detail—what the pain feels like, where it travels, and what makes it better or worse. Based on this and neurological tests, imaging may be ordered if symptoms are severe or don't improve after several weeks of conservative care. You can learn more about when these tests are ordered on this NCBI Bookshelf resource.
Red Flags: When to Seek Immediate Medical Help
While most cases of lower back nerve pain improve with conservative care, certain "red flag" symptoms require immediate medical attention as they can indicate a serious condition. Seek emergency care if you experience any of the following:
- Loss of bowel or bladder control: A critical sign of severe nerve compression (cauda equina syndrome).
- Progressive or severe leg weakness: Sudden weakness or "foot drop" that makes walking difficult.
- Numbness in the groin or "saddle" area: Numbness around the groin, buttocks, and inner thighs, another sign of cauda equina syndrome.
- Pain following a severe accident or trauma: Pain after a fall or car accident requires an immediate check for fractures or spinal damage.
- Unexplained weight loss or fever: When combined with back pain, these could signal an infection or tumor.
When it comes to these critical symptoms, it's better to be safe than sorry.
Effective Treatments for Lower Back Nerve Pain
The good news is that most lower back nerve pain is treatable, often without surgery. The goal of treatment is to reduce pain and improve mobility. About 80% to 90% of people with sciatica, the most common type of lower back nerve pain, improve without surgery, typically within four to six weeks of starting conservative care. Patience is key, as it can take time for treatments to work.
At-Home and Lifestyle Management
Start with these simple, effective at-home strategies as your first line of defense:
- Activity modification (avoiding prolonged rest): Avoid prolonged bed rest, which can worsen pain. Instead, engage in gentle movement and avoid activities that aggravate your symptoms. The goal is to stay active without causing more irritation.
- Ice and heat therapy: Use cold packs for the first few days to reduce acute pain and swelling. Afterward, switch to heat to relax muscles and improve blood flow. Always protect your skin and avoid heat on new injuries.
- Maintaining good posture: Good posture is crucial. Use lumbar support when sitting and try to ease strain when standing for long periods by shifting your weight.
- Using topical creams for targeted relief: Topical creams can provide comfort right where you need it. Neuropasil Nerve Pain Relief Cream is formulated with natural ingredients like Aloe, Urea, and Menthol to calm nerve discomfort at the source, offering fast-acting relief. You can learn more about using topical creams for targeted relief on our blog.
Professional Support and Guidance
If at-home strategies aren't enough, professional support can help:
- Physical therapy recommendations: A physical therapist can be a game-changer, creating a personalized exercise plan to strengthen your core, improve flexibility, and teach you proper body mechanics to reduce nerve pressure.
- Guidance from healthcare providers: Your doctor can provide an accurate diagnosis and guide your treatment options, offering advice on activity levels and other interventions.
- Personalized exercise plans: Working with a professional ensures your exercises are custom to your condition, minimizing injury risk and maximizing recovery.
- When to consider further medical evaluation: If symptoms worsen or don't improve after 4 to 6 weeks of conservative care, consult your doctor. They may suggest further tests or interventions. For more detailed information, you can refer to OrthoInfo.
Prevention: Exercises and Lifestyle Changes
Proactive lifestyle choices are powerful tools in preventing lower back nerve pain. By building resilience and being mindful of your movements, you can significantly reduce your risk.
Key Risk Factors to Be Aware Of
Knowing what factors increase your risk is the first step toward prevention:
- Age: The risk of sciatica peaks in the 40s, while disc issues are most common between 30 and 50. Age-related changes like spinal stenosis also increase risk.
- Obesity: Excess weight, particularly around the midsection, adds stress to the spine and can accelerate disc degeneration.
- Sedentary lifestyle: Lack of movement weakens core support muscles, and prolonged sitting increases pressure on spinal discs.
- Occupations: Jobs requiring heavy lifting, prolonged driving, or awkward postures put a strain on the lower back.
- Smoking: Nicotine reduces blood flow to spinal discs, which can speed up their degeneration and increase injury risk.
- Diabetes: This condition can cause nerve damage throughout the body, including the lower back. You can learn more about this risk factor from the Cleveland Clinic.
Stretches and Exercises to Manage Lower Back Nerve Pain
Regular movement, stretching, and strengthening are among the best ways to prevent and manage lower back nerve pain. Always consult a healthcare professional before starting a new exercise program if you're in pain.
Here are a few gentle stretches to improve flexibility:
- The Knee-to-chest stretch: Lie on your back with knees bent. Gently pull one knee to your chest, hold for 20-30 seconds, and switch legs.
- For the Piriformis stretch, lie on your back with knees bent. Cross one ankle over the opposite knee and gently pull the thigh of the non-crossed leg toward you. Hold for 20-30 seconds and repeat on the other side.
- A general Gluteal stretch can also be beneficial. From your back, pull one knee towards your opposite shoulder to release tightness in your hip and gluteal muscles.
Beyond stretching, core strengthening is vital. Exercises like planks build spinal support without adding strain. A 2020 study showed that specific stabilization exercises were effective at providing pain relief.
Incorporating good ergonomics at work and home, along with proper lifting techniques (bend your knees, keep your back straight), can make a huge difference. For even more ideas, you can find more exercises for pain relief on our blog.
Frequently Asked Questions about Lower Back Nerve Pain
If you're struggling with lower back nerve pain, it's normal to have questions. Here are answers to some of the most common ones.
How long does a pinched nerve in the lower back last?
The duration varies depending on the cause and severity. Most acute cases improve within 4 to 6 weeks with conservative care. More chronic conditions may require ongoing management. If your symptoms persist or worsen after 6 weeks, consult your healthcare professional to adjust your treatment plan.
Is walking good for a pinched nerve in the lower back?
Yes, gentle walking is often beneficial as it promotes blood flow, reduces stiffness, and keeps support muscles active. Start slowly and listen to your body. If walking increases your pain, stop and consult a physical therapist. They can guide you on the right type and amount of activity to stay active without aggravating the nerve.
What does a pinched nerve in the lower back feel like?
A pinched nerve in the lower back feels different from a muscle ache. It's typically a sharp, shooting, or burning pain, sometimes like an electric shock. The pain radiates down the nerve's path into the buttock, leg, and foot. You may also experience numbness, tingling, or, in severe cases, muscle weakness or foot drop. The exact sensations depend on which nerve is affected.
Conclusion
You now know that lower back nerve pain is a specific condition, distinct from a simple backache. This traveling, burning pain is a sign that a nerve needs attention.
The key takeaway is that there's hope. Between 80-90% of cases improve without surgery, often through conservative care like gentle movement, good posture, and targeted stretches. Prevention is rooted in building a strong core, maintaining good posture, and using proper lifting techniques.
When you need targeted relief, Neuropasil Nerve Pain Relief Cream offers a natural approach. Formulated with Aloe, Urea, and Menthol, it provides fast-acting, soothing comfort right where you need it. It's an essential tool for managing sciatica, nerve pain, and general soreness.
We created Neuropasil to help you move freely and comfortably. Understanding your pain is the first step, and you've taken it today.
Learn more about our nerve relief formula and find how natural, targeted relief can help you reclaim your active life.
References
When we set out to create this guide on lower back nerve pain, we wanted to make sure every piece of information came from trusted, credible sources. After all, when you're dealing with pain, you deserve accurate, reliable information you can count on.
We've drawn from leading medical institutions and peer-reviewed research to bring you the most current understanding of nerve pain, its causes, and effective treatments. Here are the sources that informed this article:
University Hospitals provided excellent insights on distinguishing between general low back pain and sciatica, helping us understand the nuanced differences that matter when you're seeking relief.
The Cleveland Clinic has been an invaluable resource, offering comprehensive information about sciatica—from what it is and what causes it, to treatment options and pain relief strategies. You can explore their detailed guide at https://my.clevelandclinic.org/health/diseases/12792-sciatica.
Mayo Clinic helped us understand the symptoms and underlying causes of both sciatica and spinal stenosis. Their evidence-based approach to patient education is second to none. Learn more about sciatica at https://www.mayoclinic.org/diseases-conditions/sciatica/symptoms-causes/syc-20377435, and explore spinal stenosis at https://www.mayoclinic.org/diseases-conditions/spinal-stenosis/symptoms-causes/syc-20352961.
The National Institute of Neurological Disorders and Stroke provided essential statistics and facts about low back pain prevalence and impact. Their 2020 fact sheet is available at https://www.ninds.nih.gov/sites/default/files/migrate-documents/lowbackpain20-ns-5161march2020508c.pdf.
Alexander CE and colleagues contributed crucial information about lumbosacral radiculopathy through their comprehensive StatPearls publication, which you can access at https://www.ncbi.nlm.nih.gov/books/NBK430837/. This resource was particularly helpful in understanding when imaging tests are typically ordered and the diagnostic process.
The research by Kostadinović S and colleagues (2020) provided evidence for the efficacy of lumbar stabilization and thoracic mobilization exercises in reducing pain intensity and improving functional disability in chronic low back pain patients. This randomized controlled trial reinforced our recommendations for exercise-based management. You can read the full study at https://pubmed.ncbi.nlm.nih.gov/32675390/.
Finally, OrthoInfo from the American Academy of Orthopaedic Surgeons offered practical guidance on herniated disks in the lower back, including when to consider further medical evaluation. Their patient education resources are available at https://orthoinfo.aaos.org/en/diseases--conditions/herniated-disk-in-the-lower-back/.
We're committed to keeping this information current and accurate. As new research emerges and our understanding of lower back nerve pain evolves, we'll continue to update this guide with the latest evidence-based insights.














