Understanding That Nagging Calf Pain
Sore calf muscle treatment starts with understanding what you're dealing with and knowing the fastest ways to get relief. Whether you're an athlete pushing through training or someone who just overdid it on a long walk, calf pain can stop you in your tracks.
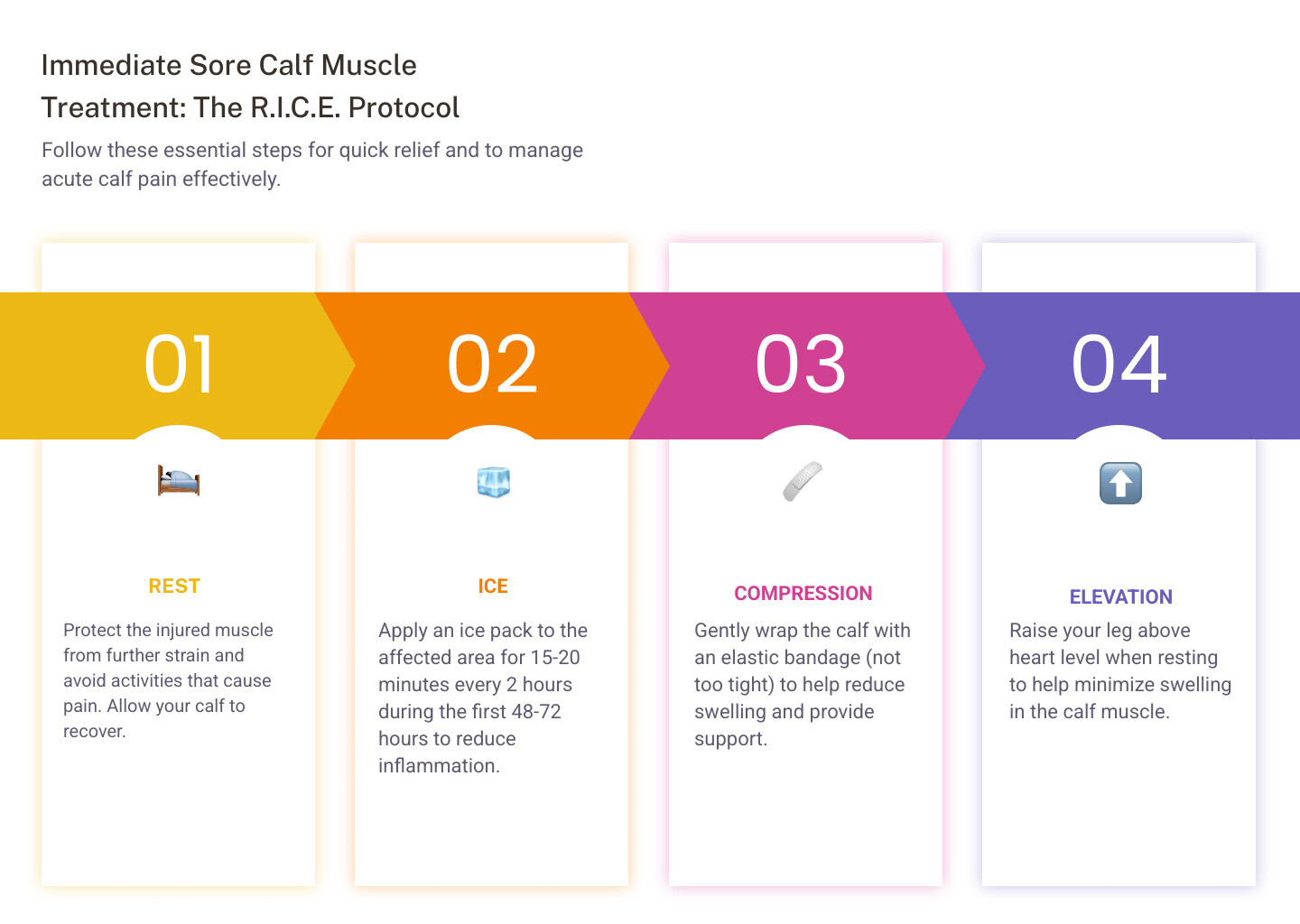
Quick Relief Methods:
- Rest and protect the muscle from further strain
- Apply ice for 15-20 minutes every 2 hours in the first 48-72 hours
- Use compression with an elastic bandage (not too tight)
- Lift your leg above heart level when resting
- Apply topical pain relief cream with menthol for soothing comfort
- Perform gentle stretches once acute pain subsides
- Stay hydrated and replenish electrolytes
Your calf is actually made up of two main muscles: the gastrocnemius (the larger, visible muscle) and the soleus (deeper muscle beneath it). These muscles meet at the Achilles tendon, which connects to your heel. When any part of this system gets overworked, strained, or cramped, you feel it.
Most calf pain comes from common causes like muscle cramps, overuse, or minor strains that you can treat at home. But it's important to know the difference between regular soreness and something more serious that needs medical attention.
The good news? Most cases respond well to simple, at-home care.
I'm Tony Enrico, and through years of working with athletes and active individuals dealing with persistent muscle discomfort, I've learned that effective sore calf muscle treatment combines immediate relief with smart recovery strategies. Whether you're managing post-workout soreness or recovering from a strain, the right approach makes all the difference.
Common sore calf muscle treatment vocab:
Why Your Calves Are Aching: Common Causes and Symptoms
Calf pain can manifest in many ways, from a dull, persistent ache to a sharp, sudden pain that makes you yelp. You might experience tightness, a feeling of stiffness, or even a visible knot in the muscle. Understanding these symptoms and their underlying causes is the first step toward effective sore calf muscle treatment.

Common Culprits: Cramps and Overuse
Most often, our calves scream at us due to muscle cramps or simply being overworked.
-
Muscle Cramps: These are sudden, involuntary contractions of the muscle that can be incredibly painful. Think of that moment when your calf seizes up in the middle of the night or during a workout – ouch!
- Causes: Muscle cramps can be triggered by several factors, including muscle overuse, dehydration, and electrolyte imbalances (like low magnesium or potassium).
- Statistics: It's quite common, with up to 50% of pregnant people experiencing muscle cramps, especially in the last three months of pregnancy. Also, about 37% of the U.S. population over 60 years of age may experience nocturnal leg cramps, often affecting the calf muscle. These can be related to other conditions or certain medications.
- Symptoms: Intense, sharp pain, a visible or palpable knot in the muscle, and temporary inability to move the affected leg.
-
Overuse and Delayed Onset Muscle Soreness (DOMS): Ever had that "good" sore feeling a day or two after a tough workout? That's DOMS, and it's a common response to new or intense physical activity.
- Causes: DOMS occurs when we push our muscles beyond their usual limits, leading to microscopic tears in muscle fibers. Our body then repairs these tears, making the muscle stronger – a natural part of muscle growth and adaptation.
- Symptoms: Muscle tenderness, stiffness, and a dull ache that typically starts 12-24 hours after exercise and can last up to 72 hours. While it can be satisfying, extreme soreness can disrupt training.
When It's More Than Soreness: Strains and Injuries
Sometimes, calf pain signals something more significant than just a cramp or DOMS. These conditions often require a more structured sore calf muscle treatment plan.
-
Calf Strain (Pulled Muscle): This happens when the muscle fibers in your calf are overstretched or torn. It's often called "tennis leg" because it's common in sports involving sudden bursts of speed or quick pivots.
- Causes: Sudden movements, overstretching, or putting excessive force through the calf muscles.
- Symptoms: Sudden, sharp pain in the back of the leg, a popping or snapping sensation at the moment of injury, swelling, bruising, and difficulty walking or rising onto your toes.
- Severity: Strains can range from mild (a few torn fibers) to severe (a complete rupture of the muscle). For details on muscle injury, you can refer to this research on muscle injury.
-
Achilles Tendonitis: This is the inflammation of the Achilles tendon, which connects your calf muscles to your heel bone.
- Causes: Overuse, sudden increase in activity, or tight calf muscles.
- Symptoms: A dull ache or tenderness in the back of your lower leg, just above the heel, especially after activity. You might also notice stiffness in the morning.
-
Contusion (Bruise): A direct blow to the calf muscle can cause a contusion.
- Causes: Impact injuries, like getting hit by a ball or falling.
- Symptoms: Localized pain, tenderness, swelling, and often visible bruising due to ruptured blood vessels under the skin.
Immediate Sore Calf Muscle Treatment at Home
For many common calf issues, especially mild strains, cramps, and DOMS, effective sore calf muscle treatment can begin right at home. Our goal is to reduce pain, minimize swelling, and kickstart the healing process.

The P.E.A.C.E. Protocol: A Modern Sore Calf Muscle Treatment
Forget R.I.C.E.? Not entirely, but the P.E.A.C.E. protocol is a more modern approach to immediate care for soft tissue injuries, emphasizing protection and early, gentle movement over complete rest. It helps prevent further damage and supports healing.
Here's how we apply the P.E.A.C.E. steps for sore calf muscle treatment:
- P - Protection: Immediately after an injury, protect the calf by reducing or restricting movement for 1 to 3 days. This doesn't mean complete immobilization, but avoiding activities that aggravate the pain.
- E - Elevation: Lift your leg above heart level as often as possible. This helps reduce swelling by allowing gravity to drain excess fluid. Prop your leg up on pillows while resting.
- A - Avoid Anti-inflammatories: In the very early stages (first few days), some experts suggest avoiding anti-inflammatory medications (like ibuprofen) as they might interfere with the natural healing process. However, for pain relief, over-the-counter options might be considered later or under medical advice.
- C - Compression: Apply a compression bandage or wrap to the calf. This helps reduce blood flow to the painful area and minimizes swelling. Ensure it's snug but not too tight – we don't want to cut off circulation! Remove compression if you experience numbness, tingling, increased pain, coolness, or swelling below the bandage.
- E - Education: Understand your injury and the recovery process. Your healthcare provider can guide you on what to expect and when to gradually return to activity. This empowers you to take an active role in your recovery.
This approach is detailed in research like "Soft-tissue injuries simply need PEACE and LOVE" Soft-tissue injuries simply need PEACE and LOVE. The key here is gentle movement rather than strict rest, which helps prevent stiffness and promotes blood flow.
Soothing Soreness with Temperature and Topical Relief
When our calves are aching, we often reach for something warm or cold. Both temperature therapies, along with topical treatments, are excellent components of sore calf muscle treatment.
- Ice Packs: For acute injuries, swelling, or tenderness, ice is our best friend. It helps numb pain and reduce inflammation. Apply an ice pack or cold compress for 10-20 minutes every 1-2 hours for the first 48-72 hours. Always place a thin cloth between the ice and your skin to prevent frostbite. The Cleveland Clinic provides excellent guidance on how to use cold therapy.
- Heat Therapy: Once the initial swelling has subsided (usually after 48-72 hours), or for general muscle stiffness and cramps, heat can be incredibly soothing. Heat helps relax and loosen tight muscles, increases blood flow to the area, and can aid in flushing out inflammation. We can use heating pads (on a low setting), warm baths, or warm compresses. Just be sure not to sleep with a heating pad on.
- Epsom Salts: A warm bath with Epsom salts (magnesium sulfate) can be a delightful way to relax muscles and potentially reduce pain. Magnesium is known for its role in muscle function and relaxation.
-
Topical Creams: These are fantastic for targeted relief. Creams containing ingredients like menthol create a cooling sensation that can distract from pain and provide temporary relief. Menthol works by interacting with cold receptors in the skin, which can help reduce pain signaling.
At Neuropasil, we understand the power of targeted relief. Our creams are formulated with ingredients like menthol, aloe, and urea to provide fast-acting, soothing comfort for sore muscles, cramps, and general aches and pains. Many of our customers, from athletes to individuals dealing with daily muscle discomfort, find our products to be an essential part of their sore calf muscle treatment. You can explore the best creams for muscle pain and see how they can help you get back on your feet.
Gentle Stretches and Exercises for Recovery
Once the acute pain begins to subside, incorporating gentle stretches and exercises is crucial for effective sore calf muscle treatment. This helps restore flexibility, improve blood flow, and prevent stiffness. Movement should always be pain-free.
- Gastrocnemius Stretch: Stand facing a wall, place your hands on it. Step one leg back, keeping your heel on the ground and your knee straight. Lean forward until you feel a stretch in your upper calf. Hold for 20-30 seconds.
- Soleus Stretch: Similar to the gastrocnemius stretch, but with the back knee slightly bent. This targets the deeper soleus muscle. Hold for 20-30 seconds.
- Calf Raises: Once you can bear weight comfortably, stand with your feet hip-width apart and slowly lift onto the balls of your feet, then lower. Start with both feet, then progress to single-leg calf raises.
- Foam Rolling: Using a foam roller can help release tension in the calf muscles. Gently roll the affected calf over the roller, stopping on tender spots for 20-30 seconds. This can improve circulation and reduce soreness, especially after exercise.
- Importance of Pain-Free Movement: The key here is not to push through pain. If a stretch or exercise causes sharp pain, stop immediately. We want to gently encourage healing and flexibility, not cause further injury. For more insights on this, you can visit our blog on muscle pain relief.
When to See a Doctor for Calf Pain
While most calf pain can be managed with home remedies, there are times when it's crucial to seek professional medical attention. Ignoring certain symptoms could lead to serious complications.
We recommend contacting a healthcare professional if you experience any of the following:
- Inability to bear weight: If you can't walk or put weight on your leg.
- Severe or sudden pain: Especially if it develops without any obvious activity or trauma.
- Significant swelling: If your calf is noticeably larger than the other.
- Skin discoloration: Redness, warmth, or tenderness, especially in one leg, could indicate a blood clot. A pale or bluish tint could signal circulatory issues.
- Warmth in the calf: A calf that feels hot to the touch could be a sign of inflammation or infection.
- Fever: If calf pain is accompanied by a fever, it warrants medical evaluation.
- Numbness or tingling: These sensations in your lower leg or foot could indicate nerve involvement.
- Pain that worsens or doesn't improve: If your calf pain persists or gets worse despite a few days of home treatment.
Red Flag Symptoms You Shouldn't Ignore
Some conditions that cause calf pain are medical emergencies. It's vital to know these red flags:
- Deep Vein Thrombosis (DVT): This is a serious condition where a blood clot forms in a deep vein, often in the leg. DVT symptoms can include swelling, pain, warmth, and redness in one leg. Up to 10% of people with symptoms often mistaken for calf muscle pulls actually have DVT, which can be life-threatening if the clot travels to the lungs. For more information on DVT symptoms and risks, consult the CDC.
-
Compartment Syndrome: This occurs when pressure builds up inside the muscles, usually after a significant injury or intense exercise. This pressure can cut off blood supply to nerves and muscles.
- Acute Compartment Syndrome: A medical emergency causing severe pain, tightness, numbness, or tingling that worsens rapidly.
- Chronic Compartment Syndrome: Pain or cramping that occurs during exercise and resolves with rest.
-
Arterial Claudication: This type of pain is caused by narrowing or blockages in the arteries that supply blood to the legs, known as peripheral arterial disease (PAD).
- Symptoms: Calf pain, cramping, or aching that occurs during physical activity (like walking) and typically subsides with rest.
- Sciatica: While originating in the lower back, sciatica can cause radiating pain, numbness, or tingling down the leg, including the calf, due to a pinched nerve.
- Diabetic Neuropathy: Nerve damage due to diabetes can cause burning, tingling, or shooting pain in the calves and feet.
Diagnosing the Root Cause of Your Sore Calf Muscle Treatment Plan
When you see a healthcare professional for calf pain, they will conduct a thorough examination to pinpoint the cause and determine the best sore calf muscle treatment plan.
- Physical Examination: The doctor will examine your leg, assess your range of motion, strength, and check for tenderness, swelling, or skin changes.
- Medical History: They'll ask about your symptoms, recent activities, any injuries, and your overall health history.
-
Imaging Tests: Depending on the suspected cause, they might order tests:
- Ultrasound: Often used to detect blood clots (DVT) or assess muscle/tendon injuries.
- MRI: Provides detailed images of soft tissues, useful for diagnosing muscle tears, tendon damage, or nerve issues.
- Differentiating Pain: A key part of diagnosis is distinguishing between muscular pain, vascular problems (like DVT or claudication), and nerve issues (like sciatica or neuropathy). This is why a professional evaluation is so important, especially if you have any red flag symptoms.
Preventing Future Calf Pain
The best sore calf muscle treatment is often prevention! By adopting a few healthy habits, we can significantly reduce our risk of experiencing calf pain.
- Proper Footwear: Wear shoes that provide adequate support and cushioning, especially during exercise. Good footwear can make a huge difference in how your calves feel.
- Hydration: Staying well-hydrated is crucial. Dehydration is a common trigger for muscle cramps. Drink plenty of water throughout the day, and more when you're active. Electrolytes also play a role, so consider electrolyte-rich fluids after intense workouts.
- Nutrition: A balanced diet supports overall muscle health. Ensure you're getting enough protein for muscle repair and antioxidants to combat inflammation.
- Gradual Exercise Progression: Avoid the "too much, too soon" trap. Gradually increase the intensity, duration, and frequency of your workouts. Our muscles need time to adapt and strengthen.
- Listen to Your Body: Pay attention to pain signals. Pushing through sharp or increasing pain can turn a minor issue into a major injury. Rest and recover when needed.
The Importance of Warm-Ups, Cool-Downs, and Stretching
These three steps are non-negotiable for anyone looking to keep their calves happy and healthy.
- Dynamic Warm-Ups: Before any physical activity, perform 5-10 minutes of dynamic warm-ups (movements that mimic your activity, like leg swings or light jogging). This increases blood flow to your muscles, making them more pliable and less prone to injury. The American Academy of Orthopaedic Surgeons (AAOS) emphasizes the importance of warm-ups.
- Static Stretching: After your workout, or as a dedicated flexibility routine, incorporate static stretches (holding a stretch for 20-30 seconds). This helps lengthen muscles, improve flexibility, and reduce post-exercise stiffness. Include stretches for both your gastrocnemius and soleus muscles.
- Cool-Downs: After intense activity, spend 5-10 minutes with light cardio (like walking) to gradually bring your heart rate down and help flush out metabolic byproducts from your muscles.
- Flexibility and Muscle Conditioning: Regular stretching and strength training keep your calf muscles conditioned, strong, and flexible, which are key factors in preventing strains and cramps.
Frequently Asked Questions about Calf Pain Relief
We get a lot of questions about calf pain, and we're here to provide some clear answers to help you manage your sore calf muscle treatment.
How long does it take for a sore calf to heal?
The recovery time for calf pain varies significantly depending on the cause and severity:
- Delayed Onset Muscle Soreness (DOMS): Typically resolves within 24-72 hours, though it can last up to 5 days for extreme soreness.
- Mild Muscle Strain: Often feels better within a few days to two weeks with proper rest and home care.
- Moderate Muscle Strain: Can take 2-4 weeks, sometimes longer, requiring a more structured rehabilitation.
- Severe Muscle Strain or Tear: May require weeks to several months of recovery, possibly involving physical therapy or even surgery.
- Muscle Cramps: Usually resolve within minutes, but residual soreness might linger for a few hours.
The key is to listen to your body and not rush the healing process.
Is it okay to walk on a strained calf muscle?
It depends on the severity of the strain.
- Mild Strain/Soreness: Gentle, pain-free movement, like light walking, is often encouraged after the initial protection phase (1-3 days post-injury). This helps prevent stiffness and promotes blood flow, aiding recovery. However, avoid any activity that causes increased pain.
- Moderate to Severe Strain: If walking causes significant pain, limping, or you can't bear weight, it's best to rest and avoid walking until advised by a healthcare professional. Pushing through severe pain can worsen the injury and prolong recovery.
Always let pain be your guide. If it hurts, don't do it!
Can massage make a calf injury worse?
The timing of massage is crucial:
- Acute Injury (First 48-72 hours): Avoid deep massage on an acute calf strain or bruise during this period. Massage can increase inflammation and bleeding, potentially worsening the injury.
- Delayed Onset Muscle Soreness (DOMS): Gentle massage can be very beneficial for DOMS, helping to reduce muscle tension and improve circulation. Research suggests that massage can reduce DOMS pain.
- Sub-Acute/Chronic Stage: Once the initial inflammation has subsided (after a few days), gentle massage can help with muscle relaxation, reduce stiffness, and break down scar tissue. If you're considering a sports massage for a recovering injury, always consult with a physical therapist or doctor first.
Conclusion: Your Next Steps for Pain-Free Calves
We've covered a lot about sore calf muscle treatment, from identifying the common culprits to understanding when to call in the professionals. Most calf pain can be effectively managed at home with simple, consistent care.
Start by implementing the P.E.A.C.E. protocol for immediate relief, incorporating both cold and heat therapies, and gently stretching as your pain allows. Prioritize prevention through proper warm-ups, cool-downs, stretching, good hydration, and appropriate footwear.
Crucially, pay attention to your body's signals. If you experience severe pain, significant swelling, skin discoloration, or any of the "red flag" symptoms we discussed, don't hesitate to seek medical attention. Your health is our top priority!
For targeted, soothing relief from muscle soreness and aches, Neuropasil's formula, powered by natural ingredients like Aloe, Urea, and Menthol, can be a valuable part of your recovery toolkit. Our fast-acting creams are designed to provide comfort for various types of pain, helping you get back to feeling your best.
Find your muscle pain relief solution
References
- American Academy of Orthopaedic Surgeons (AAOS). (n.d.). Warm-Up, Cool-Down, and Be Flexible. Retrieved from https://orthoinfo.aaos.org/en/staying-healthy/warm-up-cool-down-and-be-flexible/
- Bodman M, et al. (2022). Peripheral diabetic neuropathy. National Center for Biotechnology Information. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK442009/
- Cleveland Clinic. (n.d.). Calf Muscle Pain. Retrieved from https://my.clevelandclinic.org/health/symptoms/22274-calf-muscle-pain
- Cleveland Clinic. (n.d.). How Long to Ice an Injury. Retrieved from https://health.clevelandclinic.org/how-long-to-ice-an-injury
- Cleveland Clinic. (n.d.). Muscle Strains. Retrieved from https://my.clevelandclinic.org/health/diseases/22336-muscle-strains
- Cleveland Clinic. (n.d.). Pulled Calf Muscle. Retrieved from https://my.clevelandclinic.org/health/diseases/21558-pulled-calf-muscle
- Cleveland Clinic. (n.d.). Should You Use Ice or Heat for Pain? Retrieved from https://health.clevelandclinic.org/should-you-use-ice-or-heat-for-pain-infographic/
- Centers for Disease Control and Prevention (CDC). (n.d.). What Is Venous Thromboembolism? Retrieved from https://www.cdc.gov/ncbddd/dvt/facts.html
- ColumbiaDoctors. (n.d.). Calf Muscle Injury Information & Treatment. Retrieved from https://www.columbiadoctors.org/health-library/condition/calf-muscle-injury/
- Davis D, et al. (2022). Sciatica. National Center for Biotechnology Information. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK507908/
- Dubois B, et al. (2019). Soft-tissue injuries simply need PEACE and LOVE. British Journal of Sports Medicine, 54(2), 72. Retrieved from https://bjsm.bmj.com/content/54/2/72.long
- FamilyDoctor.org. (n.d.). Sore Muscles from Exercise. Retrieved from https://familydoctor.org/sore-muscles/
- Foran J. (2021). Deep Vein Thrombosis. American Academy of Orthopaedic Surgeons. Retrieved from https://orthoinfo.aaos.org/en/diseases--conditions/deep-vein-thrombosis/
- Harvard Health Publishing. (n.d.). How to get rid of muscle cramps in your legs. Retrieved from https://www.health.harvard.edu/pain/how-to-get-rid-of-muscle-cramps-in-your-legs
- Harvard Health Publishing. (n.d.). Muscle Strain. Retrieved from https://www.health.harvard.edu/atoz/muscle-strain-a-to-z
- Healthline. (n.d.). Calf Pain: Causes and Treatments. Retrieved from https://www.healthline.com/health/calf-pain
- Healthline. (n.d.). What Is Delayed Onset Muscle Soreness (DOMS) and What Can You Do About It? Retrieved from https://www.healthline.com/health/doms
- Healthwise, LLC. (n.d.). Calf Muscle Injury. Kaiser Permanente. Retrieved from https://healthy.kaiserpermanente.org/health-wellness/health-encyclopedia/he.calf-muscle-injury.abq4844
- Healthwise, LLC. (n.d.). Calf Muscle Injury. Lancaster General Health. Retrieved from https://www.lancastergeneralhealth.org/healthwise-library/condition-categories/first-aid?lang=en-us&DocumentId=abq4844
- Hopkins Medicine. (n.d.). Soft-Tissue Injuries. Retrieved from https://www.hopkinsmedicine.org/health/conditions-and-diseases/softtissue-injuries
- Mayo Clinic. (n.d.). Achilles Tendinitis. Retrieved from https://www.mayoclinic.org/diseases-conditions/achilles-tendinitis/symptoms-causes/syc-20369020
- Mayo Clinic. (n.d.). Muscle Cramp. Retrieved from https://www.mayoclinic.org/diseases-conditions/muscle-cramp/symptoms-causes/syc-20350820
- McClinton S, et al. (2017). Nonsurgical management of midsubstance achilles tendinopathy. ScienceDirect. Retrieved from https://www.sciencedirect.com/science/article/abs/pii/S0891842216301215
- Medical News Today. (n.d.). What causes calf muscle pain? Retrieved from https://www.medicalnewstoday.com/articles/321446
- MedicineNet. (n.d.). How Do You Relieve Sore Calves? 10 Home Remedies & Treatments. Retrieved from https://www.medicinenet.com/howdoyourelievesore_calves/article.htm
- Mulcahey M. (2019). Muscle contusion (bruise). American Academy of Orthopaedic Surgeons. Retrieved from https://orthoinfo.aaos.org/en/diseases--conditions/muscle-contusion-bruise/
- National Heart, Lung, and Blood Institute (NHLBI). (n.d.). Varicose Veins. Retrieved from https://www.nhlbi.nih.gov/health/varicose-veins
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). (n.d.). What is diabetic neuropathy? Retrieved from https://www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems/nerve-damage-diabetic-neuropathies/what-is-diabetic-neuropathy
- National Library of Medicine (NLM). (n.d.). Anatomy, Bony Pelvis and Lower Limb, Calf. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK459362/
- National Library of Medicine (NLM). (n.d.). Management of pain using magnesium sulphate: a narrative review. Retrieved from https://pubmed.ncbi.nlm.nih.gov/35086408/
- National Library of Medicine (NLM). (n.d.). The effect of cryotherapy on nerve conduction velocity, pain threshold and pain tolerance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2465313/
- National Library of Medicine (NLM). (n.d.). Water intake after dehydration makes muscles more susceptible to cramp but electrolytes reverse that effect. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6407543/
- Orthoinfo.aaos.org. (n.d.). Compartment Syndrome. Retrieved from https://orthoinfo.aaos.org/en/diseases--conditions/compartment-syndrome/
- Pabón M, et al. (2022). Achilles tendonitis. National Center for Biotechnology Information. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK538149/
- PubMed. (n.d.). Up to 10% of people with symptoms of calf pulls have DVT. Retrieved from https://pubmed.ncbi.nlm.nih.gov/12091669/
- SantaAnna JPC, et al. (2022). Muscle injury: pathophysiology, diagnosis, and treatment. National Center for Biotechnology Information. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8856841/
- Torlincasi AM, et al. (2023). Acute compartment syndrome. National Center for Biotechnology Information. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK448124/
- WebMD. (n.d.). Why Does My Calf Muscle Hurt? Retrieved from https://www.webmd.com/pain-management/ss/slideshow-why-does-my-calf-muscle-hurt
- Zemaitis MR, et al. (2023). Peripheral arterial disease. National Center for Biotechnology Information. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK430745/














