Understanding the Pain That Radiates Down Your Leg
What is sciatica? Sciatica is pain that radiates along the sciatic nerve, which runs from your lower back through your hips and buttocks and down each leg. It's a symptom (not a disease) caused by compression or irritation of the nerve roots in your lumbar spine.
Quick Answer:
- Location: Pain travels from lower back down one leg, often to the foot
- Feel: Sharp, burning, or electric shock-like sensation
- Cause: Usually a herniated disc pressing on the sciatic nerve
- Prevalence: Affects up to 40% of people at some point in their lives
- Duration: Most cases improve within 4-6 weeks
- Key Difference: Unlike general back pain, sciatica radiates down the leg below the knee
The sciatic nerve is the longest and thickest nerve in your body. When something compresses it—like a herniated disc or bone spur—the pain can be intense. About 90% of sciatica cases are caused by a spinal disc herniation, and fortunately, 80-90% of people recover without surgery, typically within several weeks.
I'm Tony Enrico, founder of Neuropasil. Our mission is to help people understand sciatica and use targeted, natural care to restore comfort and mobility.
What is Sciatica? A Deep Dive into Causes and Symptoms
If you've ever felt searing pain shoot from your lower back down your leg, you've likely experienced sciatica. Understanding what is sciatica starts with the nerve itself and why irritation can cause striking, radiating pain that disrupts daily life.
Defining Sciatica and the Sciatic Nerve
The sciatic nerve—the body's largest, formed by nerve roots L4-S3—travels from the lower spine through the hips and buttocks, down each leg to the feet. This remarkable nerve is about as thick as your thumb at its widest point. It powers muscles in the back of the knee and lower leg and supplies sensation to much of the lower limb, including the skin of your leg and the sole of your foot.
When these nerve roots are compressed, irritated, or inflamed, sciatica occurs. Clinically, this is called lumbar radiculopathy. Sciatica is a symptom signaling an underlying issue affecting the nerve, not a diagnosis by itself. The pain follows the nerve's path, which explains why discomfort can travel such a long distance from its origin in the spine.
Recognizing the Telltale Symptoms
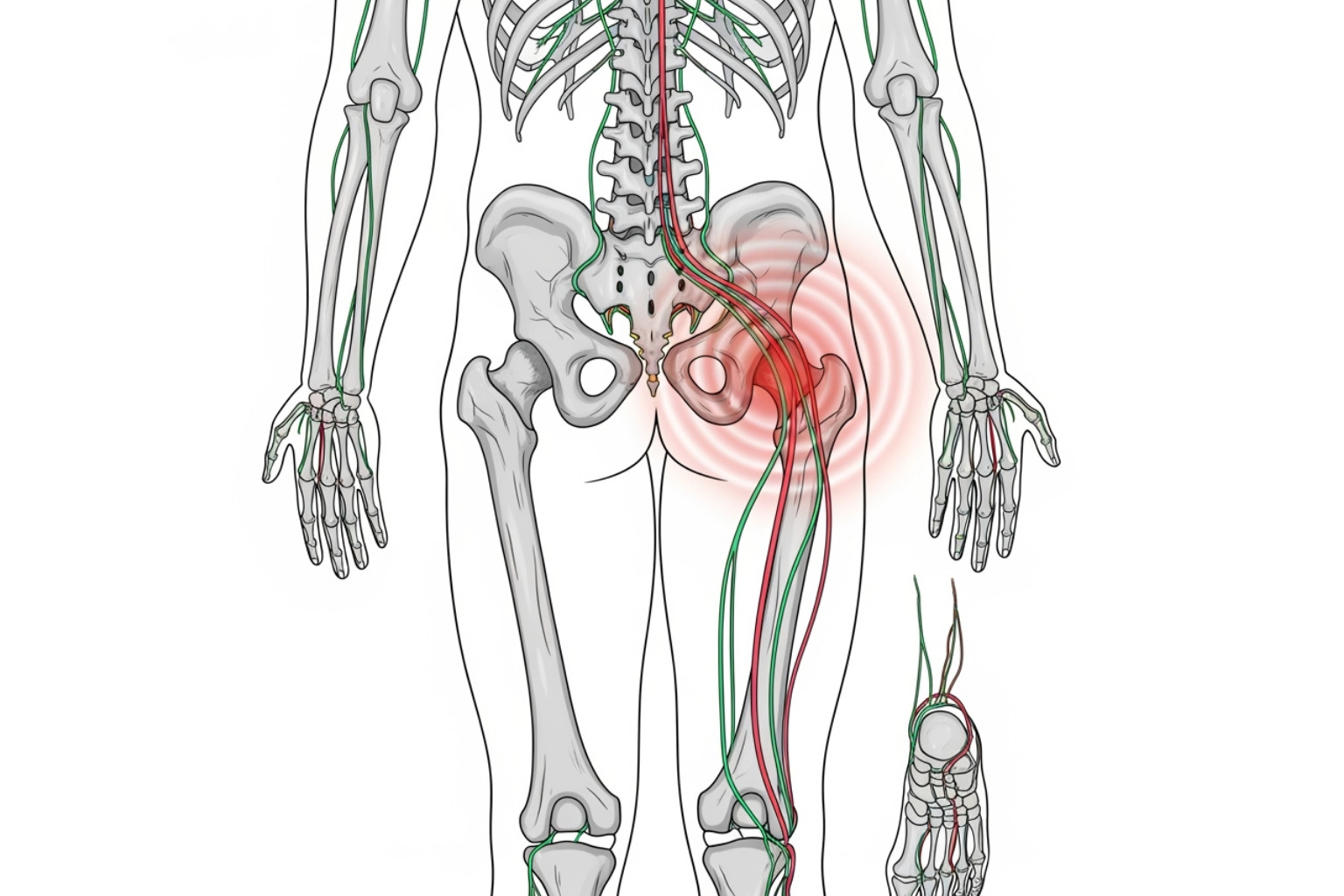
Hallmark features include pain that radiates from the lower back through the buttock and down the back of the thigh/calf—usually on one side. The pain pattern is distinctive and often follows a predictable route. It can feel like a dull ache, sharp burn, or an electric shock. The intensity can range from mild discomfort to excruciating pain that makes standing or walking difficult. Other common signs:
- Numbness/tingling in the leg or foot, often described as pins and needles
- Muscle weakness, sometimes causing foot drop or difficulty moving the foot and toes
- Burning sensation that travels down the leg
- Difficulty sitting for extended periods
Coughing, sneezing, or prolonged sitting can worsen symptoms due to increased pressure on the nerve; gentle walking or lying down may help. Symptoms often start gradually and may worsen over time without proper treatment. For more detailed information, see Decoding Sciatica Symptoms, Causes, and How to Identify Nerve Discomfort.
The Most Common Causes of Sciatic Nerve Pain
- Herniated Disc: Accounts for approximately 90% of cases; disc material presses on nerve roots when the soft inner core pushes through the tougher outer ring.
- Spinal Stenosis: Narrowed spinal canal compresses nerves, more common in adults over 50.
- Degenerative Disc Disease: Age-related disc changes can irritate nearby nerves as discs lose hydration and height. Details: Degenerative Disc Disease.
- Spondylolisthesis: A vertebra slips forward over the one below it, pinching the nerve.
- Piriformis Syndrome: Tightness/spasm of the piriformis muscle in the buttocks compresses the sciatic nerve.
Less common causes include spinal tumors, traumatic injuries, infections, or pregnancy-related pressure on the nerve. Each cause requires a different treatment approach, making proper diagnosis essential. Learn more at Why Your Sciatic Nerve Is Screaming: Causes and Relief.
Getting a Diagnosis and Finding Relief
When sharp, radiating pain shoots down your leg, a clear diagnosis guides effective relief.
What is sciatica diagnosis and when should you see a doctor?
A clinician will review your medical history and perform a focused exam: posture and gait observation, muscle strength testing, reflexes, and sensation checks. The classic straight-leg-raise (SLR) helps confirm nerve root irritation.

Imaging is used selectively: X-rays assess bony changes; MRI best visualizes discs, nerves, and ligaments; CT (sometimes with myelogram) offers detailed cross-sections. EMG/NCS can localize nerve root involvement and gauge severity.
Seek urgent care for red flags: sudden severe pain with marked numbness/weakness, symptoms after significant trauma, loss of bowel/bladder control, progressive neurological deficits, fever with back pain, new redness/swelling, pain that worsens when lying down or wakes you at night, or symptoms persisting beyond several weeks.
At-Home and Non-Surgical Treatments
Most cases improve without surgery (often within several weeks for herniated-disc–related sciatica).
- Hot and cold therapy: Ice 15-20 minutes several times daily for the first 48-72 hours; switch to heat if it feels better to relax muscles and boost circulation.
- Gentle movement: Avoid prolonged bed rest. Short walks, gentle yoga, and targeted stretches reduce stiffness and support healing. See 7 Proven Natural Ways to Treat Sciatica Pain at Home for Fast Relief.
- OTC NSAIDs: Ibuprofen or naproxen can reduce pain and inflammation; follow label directions and ask your clinician if you have other conditions or take medications.
- Topicals for targeted relief: Neuropasil nerve pain relief cream delivers fast-acting, localized comfort with Aloe, Urea, and Menthol—without systemic side effects. Many customers in New York City and across the United States use Neuropasil as a go-to nerve pain relief cream and muscle pain relief cream. Learn more: The Complete Guide to Nerve Pain Relief Creams.
Medical and Advanced Interventions
- Physical therapy: Core and hip strengthening, mobility work, and posture training to relieve current pain and prevent recurrence.
- Prescription medications: Short courses of stronger anti-inflammatories, muscle relaxants, or nerve-pain agents (e.g., gabapentin/pregabalin) when appropriate.
- Epidural steroid injections: Potent anti-inflammatory medication placed near the affected nerve root to reduce swelling and pain for weeks to months.
- Supportive therapies: Gentle massage, guided stretching; consider acupuncture or chiropractic care with qualified clinicians and inform your primary provider.
- Surgery (last resort): Microdiscectomy or laminectomy for severe or progressive deficits or when conservative care fails. Discuss risks/benefits thoroughly. See Diagnosis and treatment of sciatica.
What is Sciatica? A Deep Dive into Causes and Symptoms
When people ask what is sciatica, they’re describing radiating pain that travels from the lower back down one leg—often past the knee—sometimes with numbness, tingling, or weakness. This pattern points to irritation of the sciatic nerve or its roots (lumbar radiculopathy).
Key signs to watch for:
- Pain that follows the nerve path: lower back/buttock to the back of the thigh and calf, sometimes into the foot
- Sensations that vary from dull ache to burning or electric-shock-like pain
- Worsening with coughing, sneezing, or prolonged sitting; relief with gentle walking or lying down
Common causes include a herniated disc (most frequent), spinal stenosis, degenerative disc changes, spondylolisthesis, and piriformis syndrome; less common causes include tumors, trauma, infection, or pregnancy-related changes. For symptom details, see Decoding Sciatica Symptoms, Causes, and How to Identify Nerve Discomfort. Learn more about disc changes at Degenerative Disc Disease and broader causes at Why Your Sciatic Nerve Is Screaming: Causes and Relief.
Getting a Diagnosis and Finding Relief
The right diagnosis is your roadmap to relief and recovery.
What is sciatica diagnosis and when should you see a doctor?
Clinicians combine history (onset, aggravators/relievers, prior injuries) with a focused exam (gait, posture, strength, reflexes, sensation). A positive straight-leg-raise test supports nerve root irritation. Imaging (X-ray, MRI, CT/myelogram) and EMG/NCS are reserved for unclear, persistent, or severe cases to confirm the source of compression.
Urgent evaluation is needed for: sudden severe pain with weakness/numbness, symptoms after major trauma, loss of bowel/bladder control, progressive neurological changes, fever with back pain, new redness/swelling, night pain or pain worse lying down, or lack of improvement after several weeks.
At-Home and Non-Surgical Treatments
- Ice (first 48-72 hours) then heat as preferred
- Gentle activity and stretching; avoid prolonged bed rest
- OTC NSAIDs as directed if appropriate
- Targeted topicals like Neuropasil nerve pain relief cream with Aloe, Urea, and Menthol for fast, localized comfort; also used as a muscle pain relief cream by many customers in New York City and across the United States
Medical and Advanced Interventions
- Physical therapy: core/hip strengthening, mobility, posture training
- Prescription medications: as directed for pain, spasm, or nerve irritation
- Epidural steroid injections: reduce inflammation around affected nerve roots
- Supportive therapies: gentle massage, guided stretching; consider acupuncture or chiropractic with qualified practitioners
- Surgery (last resort): microdiscectomy or laminectomy for persistent or progressive deficits after conservative care. More details: Diagnosis and treatment of sciatica.
Sources
- American Association of Neurological Surgeons. (n.d.). Lumbar Spinal Stenosis. Retrieved from https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Lumbar-Spinal-Stenosis
- Cook, C. E., Taylor, J., Wright, A., Milosavljevic, S., Goode, A., & Whitford, M. (2014). Risk factors for first-time incidence sciatica: a systematic review. Physiotherapy Research International, 19(2), 65–78. https://pubmed.ncbi.nlm.nih.gov/24327326/
- Johns Hopkins Medicine. (n.d.). Degenerative Disc Disease. Retrieved from https://profiles.hopkinsmedicine.org/search?unified="Degenerative+Disc+Disease"&sort=networks%2Crelevance%2Cavailabilitydensitybest
- Koes, B. W., van Tulder, M. W., & Peul, W. C. (2007). Diagnosis and treatment of sciatica. BMJ, 334(7607), 1313–1317. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1895638














