Understanding the Path to Relief: Why Millions Seek to Relieve Sciatic Nerve Pain
If you need to relieve sciatic nerve pain, you're not alone. About 40% of people experience this sharp, radiating discomfort at some point in their lives. The good news? 80-90% of people with sciatica improve within a few weeks with the right approach.
Quick Relief Options:
- Hot and cold therapy (15-20 minutes each)
- Gentle stretches like knee-to-chest and piriformis stretches
- Short walks to maintain mobility
- Proper posture and supportive seating
- Over-the-counter pain relievers for inflammation
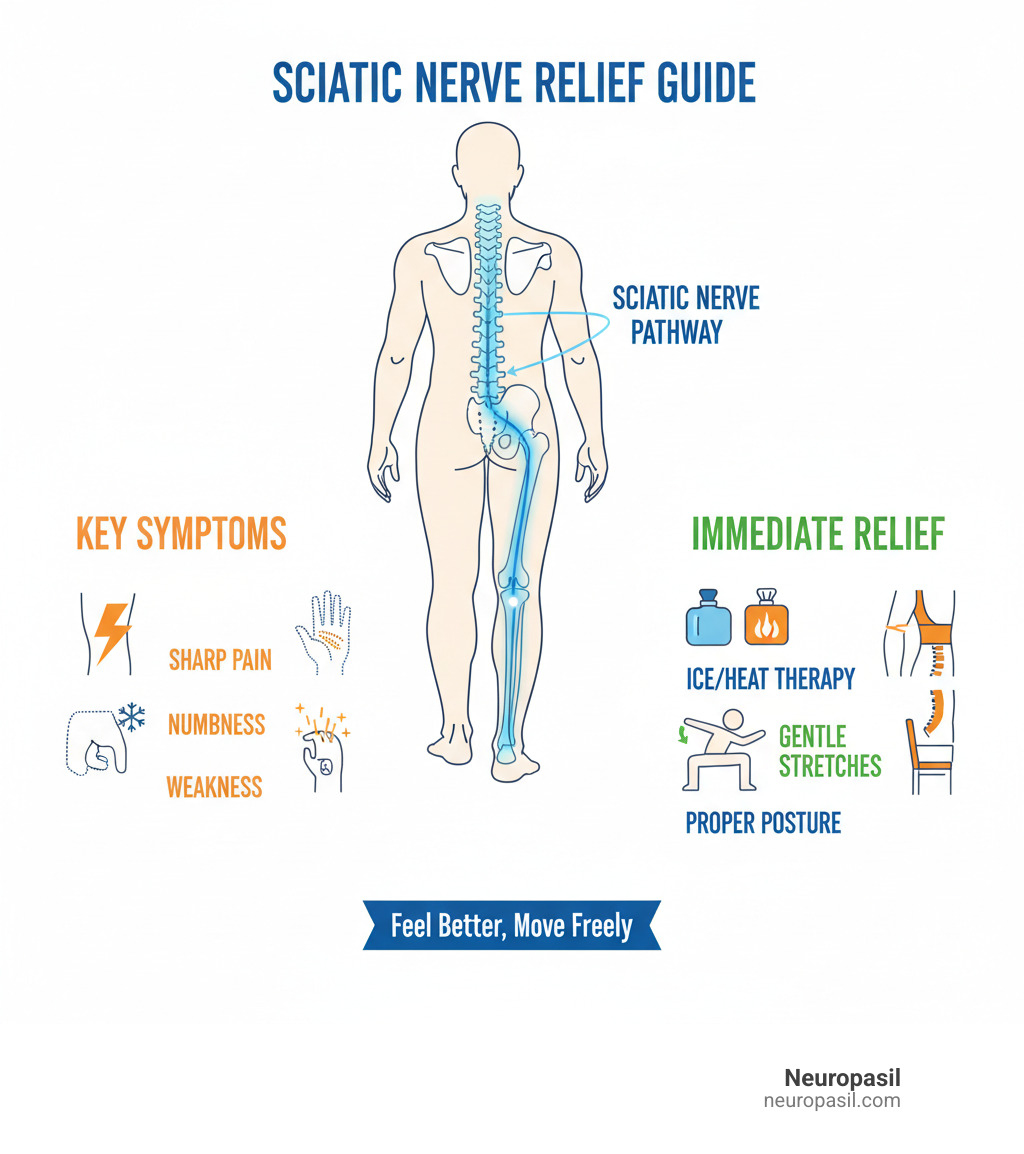
Sciatica happens when your sciatic nerve - the longest nerve in your body - gets irritated or compressed. This nerve runs from your lower back through your buttocks and down each leg. When something presses on it, like a herniated disc or tight muscles, you feel that unmistakable pain.
The pain can feel like being "stabbed with a knife" or getting an "electrical shock," as many people describe it. It might start in your lower back and shoot down one leg, sometimes reaching your foot. You might also feel numbness, tingling, or weakness.
But here's what matters most: sciatica often doesn't last longer than six weeks. Most cases resolve on their own with simple, at-home care. You don't need to suffer through it or worry that it's permanent.
The key is knowing which strategies actually work and how to use them safely. Some approaches provide immediate relief, while others help prevent future flare-ups. Understanding both gives you the best chance of getting back to your active lifestyle quickly.
Understanding Sciatica: Symptoms and Common Causes
To effectively relieve sciatic nerve pain, it helps to understand the cause. Sciatica isn't a disease, but a symptom that your sciatic nerve—the thickest and longest nerve in your body—is being compressed or irritated. This nerve runs from your lower back down to your toes.
Sciatica usually affects just one side of the body. The pain typically follows the nerve's path, starting in the lower back or buttock and shooting down the leg. While radiating pain is the main symptom, you might also experience numbness, tingling (pins and needles), or weakness in the affected leg. This can sometimes lead to "foot drop," making it hard to lift the front of your foot. Our guide on Sciatica Pain Symptoms offers more detail.
Common causes of sciatic nerve compression include:
- Herniated disc: A spinal disc bulges and presses on the nerve. This is the most frequent cause.
- Spinal stenosis: The spinal canal narrows, squeezing the nerve.
- Piriformis syndrome: A deep buttock muscle spasms and irritates the sciatic nerve. It can mimic disc-related sciatica. Learn more from this research on Piriformis Syndrome.
- Spondylolisthesis: One vertebra slips over another, pinching the nerve.
- Back injury: Trauma from a fall or accident can also trigger sciatica.
For more on related issues, see our article on Lower Back Pain Causes.
What Sciatic Pain Feels Like
Sciatic pain is distinct from a typical backache. It's often described as:
- A burning sensation or a sharp, shooting pain.
- An electric shock that is sudden and intense.
- A constant dull ache in the buttock or thigh.
Movement often makes things worse, such as standing up, bending, or walking. Even coughing and sneezing can trigger sharp pain by increasing pressure in the spine.
Common Triggers and Risk Factors
Certain factors increase your risk of developing sciatica:
- Age-related changes: Natural wear and tear on the spine, like disc degeneration, makes nerve compression more likely.
- Obesity: Excess weight puts significant stress on your spine.
- Occupation: Jobs that involve prolonged sitting, heavy lifting, or frequent twisting can trigger sciatica.
- Diabetes: High blood sugar can lead to nerve damage, increasing your risk.
- Poor posture: Slouching or improper body mechanics puts strain on your lower back.
Understanding these risks is the first step to making changes that can help relieve sciatic nerve pain and prevent it from returning.
Immediate At-Home Strategies to Relieve Sciatic Nerve Pain
When sciatica strikes, your first goal is immediate relief. Fortunately, many simple self-care measures can be done at home for effective pain management and inflammation reduction. Knowing what to do—and what to avoid—is key to calming an irritated sciatic nerve.

Do:
- Apply hot or cold packs.
- Keep moving gently.
- Maintain good posture.
- Consider over-the-counter pain relievers (if safe for you).
- Try gentle self-massage.
Avoid:
- Prolonged bed rest.
- Forcing painful stretches.
- Ignoring serious warning signs (like loss of bladder control).
- Sitting for long periods without breaks.
Hot and Cold Therapy
Hot and cold therapy is a simple, effective way to relieve sciatic nerve pain.
- Ice packs: Use for the first 48 hours of a flare-up to reduce inflammation. Wrap an ice pack in a towel and apply it to the painful area for 15-20 minutes at a time, several times a day.
- Heat packs: After 48 hours, switch to heat. Heat relaxes tight muscles and improves blood flow. As evidence on heat for muscle stiffness confirms, it's useful for muscle tightness contributing to pain.
- Alternating therapy: Many people find switching between hot and cold provides the most relief. Always protect your skin and limit applications to 15-20 minutes.
The Role of Rest and Gentle Movement
While it's tempting to stay in bed, avoiding prolonged bed rest is crucial for recovery. Too much inactivity can weaken muscles and stiffen joints, making pain worse. Harvard Health on limited bed rest confirms that excessive rest can be counterproductive.
The key is gentle activity. As soon as you can, start with short walks (5-10 minutes) to keep your muscles from stiffening. Maintaining mobility is vital, but listen to your body. Stop any movement that causes sharp, shooting pain. Mild discomfort that eases with movement is a good sign to continue gently.
Posture and Supportive Habits
Your daily habits for sitting, standing, and sleeping significantly impact your sciatic nerve. Small adjustments can make a big difference.
- Proper posture: When sitting, use ergonomic seating with lumbar support, keep feet flat on the floor, and avoid crossing your legs.
- Sleeping positions: If you're a side sleeper, place a pillow between your knees. If you're a back sleeper, put a pillow under your knees. Avoid sleeping on your stomach.
- Mindful movement: Take breaks every 30-60 minutes to stand, walk, and stretch gently.
- Supportive cushions: Use a lumbar cushion in your chair or car seat for extra back support.
Targeted Exercises and Lifestyle Changes for Lasting Relief
While immediate relief is important, long-term recovery comes from physical activity, building core strength, and improving flexibility. This proactive approach addresses root causes and builds resilience against future flare-ups. For more context on nerve pain, see our guide on Sciatic Nerve Pain.

Stretches to Relieve Sciatic Nerve Pain and Improve Mobility
Gentle stretching can target tight muscles that compress the sciatic nerve. Focus on stretches that externally rotate the hip, holding each for 30 seconds and repeating 3 times per side. Avoid bouncing or forcing any movement.

- Knee-to-chest stretch: Lie on your back, bend your knees, and gently pull one knee to your chest to lengthen lower back muscles.
- Seated glute stretch: While seated, cross one ankle over the opposite knee and lean forward gently to target deep gluteal muscles.
- Standing hamstring stretch: Place one foot on a step with the leg straight. Lean forward from your hips. This helps because tight hamstrings can contribute to lower back tension.
- Piriformis stretch (figure-4): Lie on your back, cross one ankle over the opposite thigh, and pull both legs toward your chest. This directly targets the muscle that often compresses the sciatic nerve.
Research on self-mobilization techniques shows these targeted movements can significantly improve physical function while reducing pain.
Lifestyle Adjustments for Prevention
Simple lifestyle adjustments can prevent future sciatica episodes:
- Weight management: Maintaining a healthy weight reduces pressure on your spine.
- Quitting smoking: Nicotine impairs blood flow to spinal discs, weakening them and increasing risk.
- Safe lifting techniques: Always lift with your legs, not your back, and avoid twisting while lifting.
- Regular low-impact exercise: Activities like swimming, yoga, and walking strengthen your core, improve flexibility, and support spinal health without high impact.
These changes support overall nerve health. For more on this topic, see our article on Peripheral Neuropathy Symptoms.
The beauty of this approach is that small, consistent changes often yield the biggest results. You're not just trying to relieve sciatic nerve pain - you're building a stronger, more resilient you.
When to Seek Professional Help: Medical Evaluation for Sciatica
Most people who need to relieve sciatic nerve pain can do so successfully at home. But sometimes, your body sends signals that it's time to get professional help. Knowing when to make that call can save you from unnecessary suffering and, in rare cases, prevent serious complications.
There are certain "red flag" symptoms that mean you need immediate medical attention - we're talking emergency room, don't-wait-until-Monday kind of urgent. These symptoms could indicate cauda equina syndrome, a rare but serious condition where the nerves at the bottom of your spinal cord get severely compressed.
Get emergency medical help right away if you experience: loss of bladder or bowel control, severe weakness in one or both legs that's getting worse, numbness around your genitals or buttocks (called "saddle anesthesia"), sciatica pain on both sides of your body, or sudden severe pain after an injury.
For less urgent but still concerning symptoms, schedule an appointment with your doctor if your pain hasn't improved after a few weeks of home care, is actually getting worse, or is preventing you from doing your normal daily activities. Your GP can evaluate what's going on and guide you toward the right treatment. For a complete picture of symptoms that warrant medical attention, check out our detailed guide on Sciatica Symptoms.
Supportive Professional Approaches
When you visit a healthcare professional, they'll start with a thorough physical examination. Don't be surprised if they ask you to do things that might seem a bit odd - like walking on your toes, rising from a squat, or lifting your legs while lying down. These simple tests help them understand how your nerves and muscles are functioning.
Diagnostic tests aren't always necessary, especially for mild cases that are improving. But if your pain is severe, persistent, or comes with those red flag symptoms we mentioned, your doctor might recommend imaging studies. X-rays can spot bone spurs or other structural changes, while MRI scans provide detailed pictures of soft tissues like discs and nerves. Sometimes a CT scan is used instead, and in certain cases, an EMG test measures how well your nerves are conducting electrical signals.
Healthcare professionals offer guidance from healthcare professionals through several approaches. Physical therapy is often the first recommendation - a skilled therapist can design a personalized movement and posture education program just for you. They'll teach you exercises to strengthen your core, improve your posture, and reduce pressure on that angry sciatic nerve.
If over-the-counter medications aren't cutting it, your doctor might prescribe stronger anti-inflammatory drugs, muscle relaxers, or even medications originally designed for other conditions (like certain antidepressants or anti-seizure drugs) that happen to be very effective for nerve pain. Corticosteroid injections delivered directly to the affected area can provide targeted relief for up to three months.
Surgery is typically reserved for severe cases where monitoring progress shows that conservative treatments aren't working after 6-12 weeks, or when further evaluation is needed for serious symptoms like significant weakness or loss of bowel/bladder control.
What to Expect from Recovery
Here's some encouraging news: the outlook for sciatica is genuinely positive. Most people (80-90%) recover without invasive procedures, and many see significant improvement within just a few weeks. Time itself is often the best medicine, especially when combined with active self-care.
Typical recovery timelines vary, but sciatica often resolves within six weeks. Some people feel better in just a few days, while others might need a few months. Your body has an amazing ability to heal itself, and most herniated discs that cause sciatica actually shrink on their own over time.
When symptoms may persist beyond the typical timeframe, it doesn't mean you're stuck with pain forever. It simply means you might benefit from a more comprehensive approach with specialist care. There's also possibility of recurrence - sciatica can come back, especially if the underlying causes (like poor posture, weak core muscles, or lifestyle factors) haven't been addressed.
The key is staying optimistic while being realistic. Your long-term outlook is excellent, especially when you combine professional guidance with the self-care strategies we've discussed. Most people not only recover but learn valuable skills for preventing future episodes.
Frequently Asked Questions about Sciatica Relief
When you're dealing with sciatica, questions seem to multiply faster than the pain itself. And honestly, that's completely understandable—this condition can be both mysterious and frustrating. Let's explore the most common concerns we hear, so you can feel more confident about your path to recovery.
How long does sciatica typically last?
Ah, the question that keeps everyone up at night! Here's the reassuring truth: most cases of acute sciatica resolve within 4 to 6 weeks with proper self-care. Your body is remarkably good at healing itself when given the right support.
However, sciatica doesn't always follow a neat timeline. Some people bounce back in a few days, while others might deal with symptoms for a few months. If your pain hangs around beyond 6 weeks, doctors consider it chronic—but that doesn't mean you're stuck with it forever.
The long-term outlook is genuinely positive. 80-90% recovery rate we mentioned earlier? That holds true even for cases that take longer to resolve. The key is staying patient with your body while remaining consistent with your care routine.
One thing to keep in mind: sciatica can recur, especially if you return to old habits or don't address the underlying causes. Think of recovery as building a foundation—the stronger you make it, the less likely you'll have to deal with this pain again.
What is the fastest way to relieve sciatic nerve pain?
We get it—when you're in agony, you want relief yesterday. While there's no single "magic bullet" for sciatica, the fastest relief usually comes from a combination approach that attacks the problem from multiple angles.
Your best bet for quick relief starts with gentle movement and targeted stretches. It might seem counterintuitive when you're hurting, but getting your body moving (carefully!) often provides faster relief than staying still. Those knee-to-chest and piriformis stretches we discussed earlier can work surprisingly quickly.
Hot and cold therapy deserves a special mention here. Many people find that alternating between ice and heat provides rapid symptomatic relief—sometimes within minutes. The cold tackles inflammation while the heat relaxes those angry muscles.
Don't overlook self-massage either. Using a tennis ball or foam roller to gently work those tight glute and piriformis muscles can offer quick relief by releasing built-up tension. Just remember to be gentle—you're trying to relieve sciatic nerve pain, not create more of it.
Over-the-counter pain relievers like ibuprofen can help reduce inflammation and pain, though the evidence for super-fast relief varies from person to person. The real secret is starting these interventions as soon as possible and being consistent with them.
Can stretching make sciatica worse?
Unfortunately, yes—stretching can absolutely make sciatica worse if done incorrectly. But don't let that scare you away from this powerful tool! The key is understanding how to stretch safely and listening to what your body tells you.
Proper form is everything. A poorly executed stretch can put more strain on your nerve rather than relieving it. If you're unsure about your technique, consider watching instructional videos or consulting a physical therapist. It's worth getting it right from the start.
Here's a golden rule: a stretch should feel like a gentle pull, never sharp pain. If you feel shooting pain, increased numbness, or tingling during a stretch, stop immediately. Your body is sending you a clear message that something isn't right.
Know when to stop. If your symptoms worsen during or after stretching, take a step back. The stretch might be too intense for your current condition, or it might not be the right one for your specific type of sciatica.
Working with a healthcare professional can be incredibly valuable here. A physical therapist can teach you proper technique, help you identify which stretches work best for your situation, and guide you in building a safe, effective routine. They can also help you distinguish between the discomfort of a good stretch and the warning signs of potential harm.
The goal is to relieve sciatic nerve pain, not create more problems. When done correctly, stretching can be one of your most powerful allies in recovery.
Conclusion: Taking Control of Your Sciatic Nerve Health
You've made it through what might feel like a crash course in sciatica management, and hopefully, you're feeling more confident about tackling this challenging condition. The truth is, while sciatica can be incredibly painful and disruptive, you have more power over it than you might think.
The journey to relieve sciatic nerve pain isn't always straightforward, but it's absolutely achievable for most people. 80-90% of people with sciatica improve within a few weeks when they take the right approach. That's not just a statistic—that's hope backed by real outcomes.
Your toolkit for recovery is now well-stocked. You understand how hot and cold therapy can provide immediate relief during those tough first 48 hours. You know that gentle movement beats bed rest every time, even when your body is screaming for you to stay still. You've learned specific stretches like the piriformis stretch and knee-to-chest that can help free up that compressed nerve.
But perhaps most importantly, you now recognize that managing sciatica isn't just about the immediate pain—it's about building habits that prevent future flare-ups. Whether that's maintaining good posture at your desk, taking regular movement breaks, or strengthening your core muscles, these lifestyle changes are your best defense against sciatica's return.
Of course, knowing when to seek professional help is just as crucial as self-care. Those red flag symptoms we discussed—like loss of bladder control or severe weakness—are your body's way of saying it needs more than home remedies. Don't ignore these signals.
The beautiful thing about sciatica recovery is that it often teaches us to be more mindful of our bodies. Many people find that after working through sciatica, they're actually stronger and more aware of their physical health than before. It's like your body is giving you a wake-up call to treat it better.
For those looking to support their nerve health journey with natural solutions, Neuropasil offers complementary approaches that work alongside the strategies we've discussed. Find natural solutions for nerve pain relief with Neuropasil and find how targeted nutrition can support your path to wellness.
Healing isn't always linear. Some days will be better than others, and that's completely normal. The key is staying consistent with your self-care routine and being patient with your body as it heals. You've got the knowledge, you've got the tools, and most importantly, you've got the determination to take control of your sciatic nerve health.














