When a Pulled Calf Muscle Stops You in Your Tracks
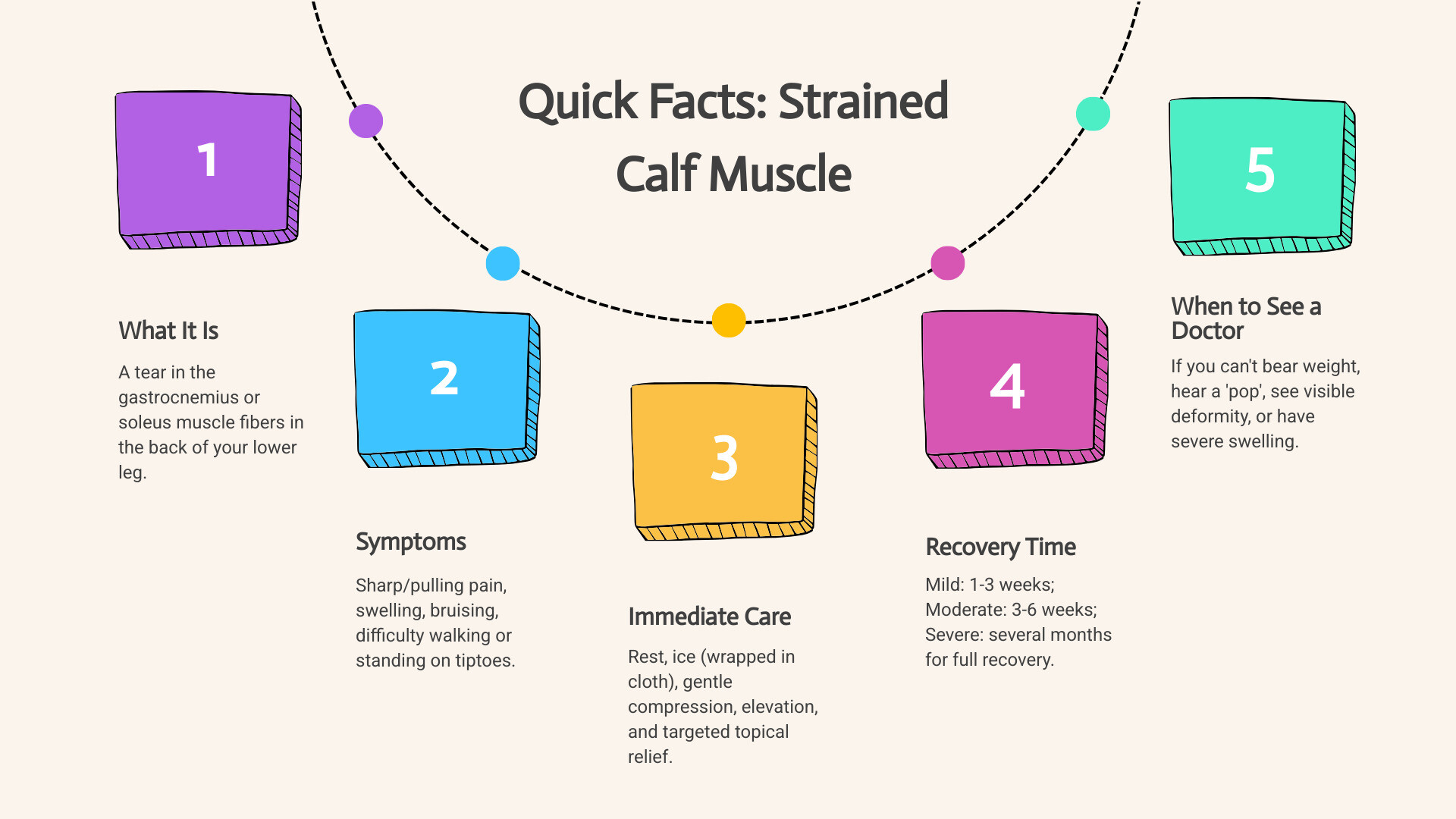
A strained calf muscle is a tear in the muscle fibers in the back of your lower leg (the gastrocnemius or soleus), causing pain that can limit your ability to walk, run, or play sports. Whether you pushed off too hard during a sprint or felt a sudden snap, a calf strain can derail your daily activities. The good news is that most heal well with the right care.
Common symptoms include sharp pain, swelling, bruising, and difficulty standing on your tiptoes. Immediate treatment involves rest, ice, compression, and elevation (RICE), along with targeted topical relief. Recovery can range from 1-3 weeks for mild strains to several months for severe tears. You should see a doctor if you can't bear weight, hear a "pop," or have severe swelling.
This guide walks you through everything from understanding the injury to getting back to full activity safely. You'll learn proven treatment steps, realistic recovery timelines, and how to prevent future injuries so you can stay active and pain-free.
Understanding Your Calf Strain: Symptoms, Causes, and Risk Factors
Understanding what's happening inside your leg is the first step toward recovery. Let's explore the anatomy, severity levels, and causes of this common injury.
What is a Strained Calf Muscle and What are the Types?
Your calf is a powerful duo of muscles: the gastrocnemius, the larger, visible muscle, and the soleus, a flatter muscle underneath. Together, they help you point your toes and push off the ground when walking, running, or jumping. A strained calf muscle occurs when these muscle fibers are overstretched or torn.
Medical professionals classify calf strains into three grades:
| Grade | Severity | Fiber Damage | Pain Level | Loss of Function |
|---|---|---|---|---|
| Grade 1 | Mild | Few fibers torn (less than 5% structural disruption) | Mild pulling sensation or dull ache, often tolerable | Minimal—you can still function, but with discomfort |
| Grade 2 | Moderate | Significant number of fibers torn (partial muscle tear) | Moderate to sharp pain, especially with movement; limping likely | Noticeable loss of strength and mobility, daily activities become challenging |
| Grade 3 | Severe | Complete tearing of the muscle-tendon unit (rupture) | Intense, sudden, sharp pain; often described as a "pop" or "snap" | Significant—unable to bear weight or move the leg; visible deformity possible |
This grading system helps set realistic expectations for recovery. For a deeper dive, see our guide on muscle strain treatment.
Common Symptoms by Severity
The symptoms of a strained calf muscle vary by severity:
- Grade 1 (mild): You'll feel a manageable pulling sensation or dull ache during or after activity. The area is tender, but swelling and bruising are minimal.
- Grade 2 (moderate): This brings sharp pain that makes continuing activity difficult. You'll likely limp, and the muscle may spasm. Swelling and bruising often appear within a day or two.
- Grade 3 (severe): You'll feel a sudden, intense, sharp pain, often with an audible "pop" or "snap." Walking is extremely difficult or impossible. Significant swelling and bruising develop quickly, and you may see a visible indentation where the muscle has torn.
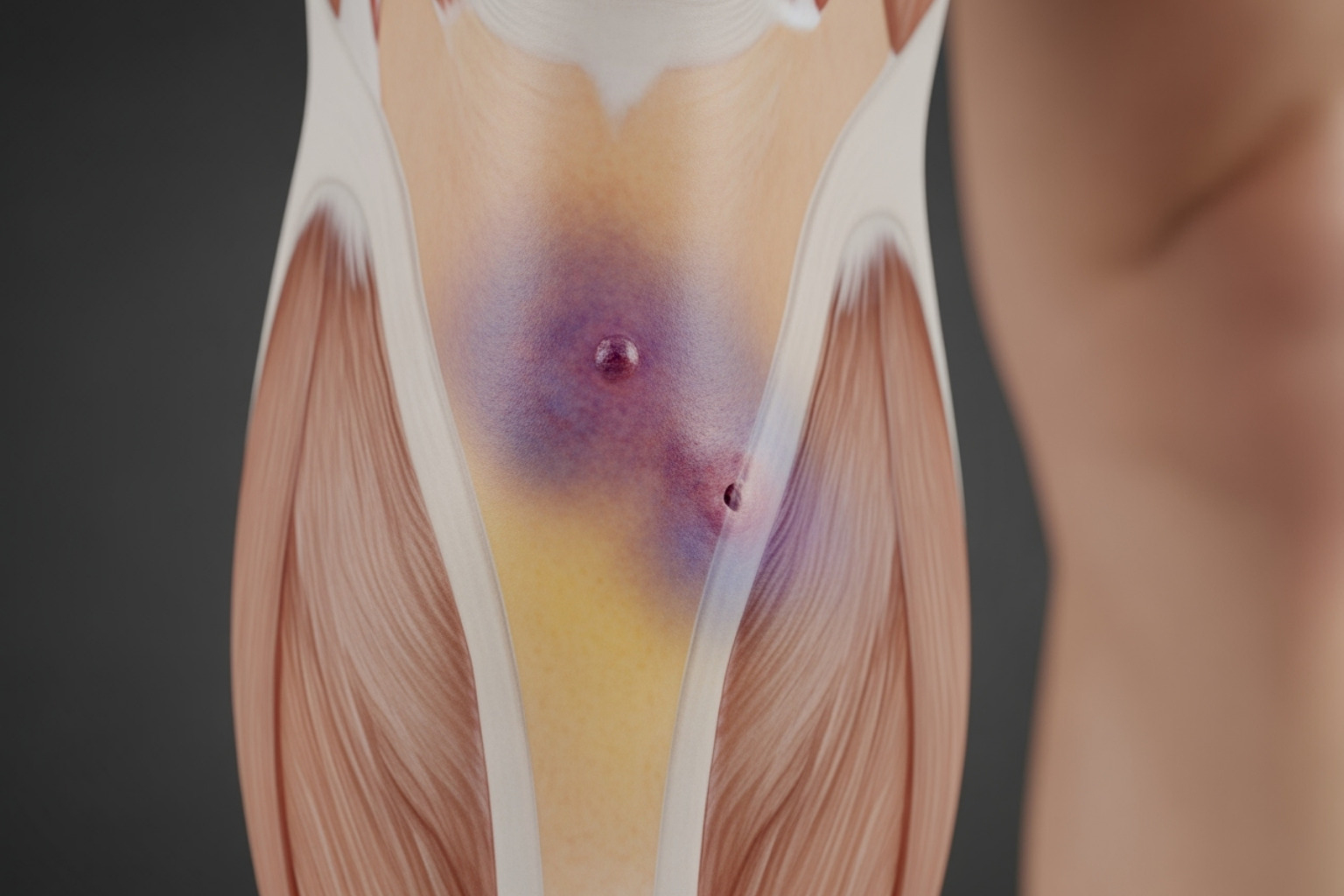
Bruising indicates internal bleeding from damaged blood vessels, a clear sign of a more significant tear.
What Causes Calf Strains and Who is at Risk?
Most calf strains happen during sudden, powerful movements like sprinting, jumping, or pivoting. This is why it's often called "tennis leg." However, overuse from repetitive activities like long-distance running can also cause gradual damage.
Several factors increase your risk:
- Poor conditioning: Muscles that aren't strong or flexible enough for the activity.
- Muscle fatigue: Tired muscles absorb shock less effectively.
- Skipping warm-ups: Cold, stiff muscles are more vulnerable.
- Age: Muscles lose elasticity and strength after 40.
- Previous injuries: A past strain weakens the area.
Research on risk factors for calf injuries confirms that tight calf muscles and a history of previous strains are significant contributors. Understanding these causes empowers you to make smarter choices to protect your calves.
Diagnosis and When to See a Doctor
While many mild calf strains can be managed at home, an accurate diagnosis is key to preventing complications and ensuring a smooth recovery.
How a Strained Calf Muscle is Diagnosed
A healthcare provider will diagnose a strained calf muscle through a combination of methods:
- Physical Examination: The provider will check for swelling, discoloration, and tenderness. They will also assess your range of motion and strength by asking you to move your ankle and push against resistance.
- Medical History: You'll be asked about how the injury occurred, whether you heard a "pop," and any previous leg injuries.
- Imaging Tests: For more severe injuries, an ultrasound can show muscle tears and fluid. An MRI may be used for a more detailed view of severe tears or complete ruptures, helping to confirm the grade of your strain. If you need a specialist, you can find a specialist for muscle strains in your area.
When to Seek Immediate Medical Attention
Trust your gut. If something feels seriously wrong, seek professional help immediately. Watch for these red flags:
- Inability to bear weight on the injured leg.
- Severe, rapidly worsening pain and swelling.
- A "pop" or "snap" sensation at the moment of injury.
- A visible deformity, gap, or lump in the muscle.
- Signs of a blood clot (DVT): Increasing calf pain not relieved by rest, progressive swelling, tenderness, unusual warmth, or redness. DVT is a medical emergency. Research shows that up to 10% of people with calf pull symptoms may actually have DVT.
Potential Complications of a Calf Injury
Proper care helps avoid complications, but it's important to be aware of the risks:
- Re-injury: Returning to activity too soon can cause another, often worse, tear.
- Chronic Pain: Lingering pain can result from incomplete rehabilitation or nerve involvement.
- Excessive Scar Tissue: Improperly healed scar tissue can reduce flexibility and strength.
- Compartment Syndrome: A rare but serious condition where severe swelling cuts off blood flow and nerve function, requiring emergency treatment.
- Deep Vein Thrombosis (DVT): A blood clot in the leg that can travel to the lungs, which is life-threatening.
Taking your recovery seriously is the best way to avoid these issues. For more on calf pain, read our article on How to Stop Calf Muscles Hurting: Causes and Relief.
Your Step-by-Step Guide to Treating a Strained Calf Muscle
Once you've identified a strained calf muscle, the actions you take in the first few days can dramatically influence your recovery. Here are the most effective treatment approaches.
Immediate Home Care: The Neuropasil Approach to Relief
In the first 48-72 hours, thoughtful home care is crucial. The goal is to protect the muscle and manage inflammation.

- Rest: Stop the activity that caused the pain. If walking hurts, use crutches to keep weight off the leg. Protection is paramount in the first 24-72 hours.
- Ice: Apply a cold pack wrapped in a towel for 15-20 minutes every 1-2 hours. This reduces pain, swelling, and inflammation.
- Compression: Use an elastic bandage or compression sleeve to control swelling. Ensure it's snug but not tight enough to cause numbness or tingling.
- Elevation: Prop your leg on pillows so your calf is above heart level. This helps drain excess fluid.
For targeted comfort, gently massage a small amount of Neuropasil Nerve Pain Relief Cream onto the affected area. Its blend of Aloe, Urea, and Menthol provides soothing relief directly at the source, calming irritated muscle fibers. Learn more about using Neuropasil for muscle pain relief. During this initial phase, avoid heat and deep massage, as they can increase swelling.
Managing Pain and Inflammation Naturally
Beyond the initial steps, natural solutions can support your body's healing process. Our Neuropasil cream, with its cooling menthol, helps interrupt pain signals and is gentle enough for regular use. You can compare it to other options in our guide to The 7 Best Muscle Creams Compared.
Additionally, focus on these supportive habits:
- Hydration: Water is essential for delivering nutrients to your injured muscle and flushing out waste. Stay well-hydrated.
- Nutrition: Eat a balanced diet rich in lean proteins for muscle repair and fruits and vegetables for their anti-inflammatory antioxidants.
- Gentle Movement: After the first few days, simple ankle pumps (slowly pointing and flexing your foot) can promote blood flow and prevent stiffness without stressing the muscle.
For more expert-approved ideas, see our list of the best creams for sore muscles.
Medical and Professional Interventions
While home care is effective for mild strains, moderate to severe injuries often require professional help.
- Physical Therapy: A physical therapist is essential for anything beyond a mild strain. They will create a custom rehabilitation program to restore strength, flexibility, and function, guiding you back to activity safely.
- Mobility Aids: For more severe strains, crutches or a walking boot may be recommended to protect the healing muscle from weight-bearing stress.
- Supportive Taping: Kinesiology tape, applied by a professional, can support the muscle and help reduce swelling and pain during recovery.
- Surgery: This is rare and typically reserved for complete ruptures in active individuals, where the muscle is surgically reattached to the tendon.
These interventions create the optimal conditions for your body to heal. For a complete overview, check out our Top 7 Muscle Strain Treatment Tips.
Recovery and Prevention: Getting Back on Your Feet and Staying There
Healing a strained calf muscle requires patience. Rushing the process can lead to re-injury, but a smart approach to rehabilitation will help you recover fully.
The Road to Recovery: Timeline and Rehabilitation
Recovery times vary by the severity of the strain:
- Grade 1 (mild): 1 to 3 weeks
- Grade 2 (moderate): 3 to 6 weeks
- Grade 3 (severe): 3 to 6 months, often with intensive rehabilitation
Your rehabilitation will progress through several phases. The golden rule is gradual progression—if an activity causes pain, scale back.
- Early Stage (First few days): Focus on rest, ice, compression, elevation, and managing pain. Applying Neuropasil Nerve Pain Relief Cream can provide soothing comfort. Gentle, pain-free movements like ankle pumps (10-15 reps, several times a day) help maintain circulation.
- Mid-Stage (Pain and swelling decrease): Begin very gentle, pain-free stretches. With your leg straight, softly pull your toes toward you, holding for 15-20 seconds. This encourages the muscle to regain its normal range of motion.
- Late Stage (Strength building): Introduce progressive strengthening exercises like calf raises (both with straight and bent knees). Start with body weight and gradually add resistance as you get stronger.
- Return to Activity: Reintroduce sport-specific movements like running or jumping drills, always pain-free and ideally under the guidance of a physical therapist.
For more strategies, see our guide to Recover Like a Pro: Strategies for Faster Muscle Healing.
How to Prevent Future Calf Muscle Injuries
Once you've recovered, preventing a repeat injury is crucial. Most calf strains are preventable with the right habits.

- Warm-Up Properly: Always perform a 5-10 minute dynamic warm-up (e.g., light jogging, leg swings) before activity.
- Stretch Consistently: After workouts, perform static stretches, holding each for 20-30 seconds. Include both the straight-leg and bent-knee wall stretches for your calves. Regular stretching improves flexibility and reduces injury risk.
- Strengthen Your Calves: Regularly perform calf raises to build muscle resilience.
- Wear Proper Footwear: Replace worn-out shoes that no longer provide adequate support.
- Stay Hydrated: Dehydrated muscles are stiff and more prone to tearing.
- Progress Gradually: Don't increase training intensity or duration by more than 10% per week.
- Listen to Your Body: Pay attention to tightness or nagging pain. It's an early warning to rest or adjust your training.
- Cross-Train: Vary your activities to avoid repetitive stress on the same muscle groups.
Conclusion: A Proactive Approach to Calf Health
You now have a roadmap to understand, treat, and prevent a strained calf muscle. From immediate home care with rest and ice to professional intervention and structured rehabilitation, you are equipped to guide your recovery.
The key takeaways are clear: respect the healing process, don't rush back to activity, and prioritize prevention. Consistent habits like proper warm-ups, stretching, and strengthening are your best defense against re-injury. Listening to your body's signals is crucial for long-term calf health.
As you manage the discomfort of a healing muscle, Neuropasil Nerve Pain Relief Cream can provide targeted, soothing comfort. The blend of Aloe, Urea, and Menthol works with your body to help you stay comfortable as your muscle repairs itself.
We're here to support you. Explore our natural pain relief solutions and visit our blog for more health tips to stay informed, empowered, and pain-free.
References
- Pulled Calf Muscle - Cleveland Clinic
- Risk factors for calf muscle strain injury in elite Australian footballers - British Journal of Sports Medicine
- Ultrasound in the evaluation of "tennis leg" - Journal of the American Academy of Orthopaedic Surgeons
- Find a Doctor for Muscle Strain - NYU Langone Health
- The importance of stretching - Harvard Health Publishing














