Understanding Sternocleidomastoid Muscle Pain: Why It Matters
Sternocleidomastoid muscle pain is a common but often misunderstood source of neck discomfort that can radiate to your head, face, shoulders, and even cause dizziness. This large muscle on each side of your neck plays a crucial role in head movement and stability—but when it's strained, overused, or develops trigger points, it can create a wide range of frustrating symptoms that interfere with daily life.
Quick Relief Guide for SCM Pain:
- Rest the affected muscle and avoid aggravating movements
- Apply ice (first 48 hours) or heat (after 48 hours) for 15-20 minutes
- Perform gentle stretches like side-bending your head away from the painful side
- Use topical pain relief cream with menthol for fast, targeted comfort
- Correct poor posture, especially "text neck" from looking down at phones
- Try self-massage along the muscle from behind your ear to your collarbone
- See a doctor if pain persists beyond 2 weeks or includes numbness/weakness
The good news? Most cases of SCM pain respond well to simple at-home treatments combined with posture awareness and targeted stretches. Understanding what causes this pain and how to address it puts you back in control.
I'm Tony Enrico, and I've spent years helping athletes and active adults find relief from stubborn muscle and nerve pain, including the complex referred pain patterns that sternocleidomastoid muscle pain can create. Through Neuropasil, I've worked with thousands who've struggled with neck tension, headaches, and the cascade of symptoms that SCM dysfunction triggers—and I've seen how the right combination of knowledge, self-care, and targeted topical relief can restore comfort and movement.
In this guide, we'll walk through everything you need to know: the anatomy and function of your SCM muscle, what causes it to hurt, how to recognize the symptoms (including those surprising referred pain patterns), and most importantly, the proven strategies to find relief and prevent future flare-ups.
Learn more about sternocleidomastoid muscle pain:
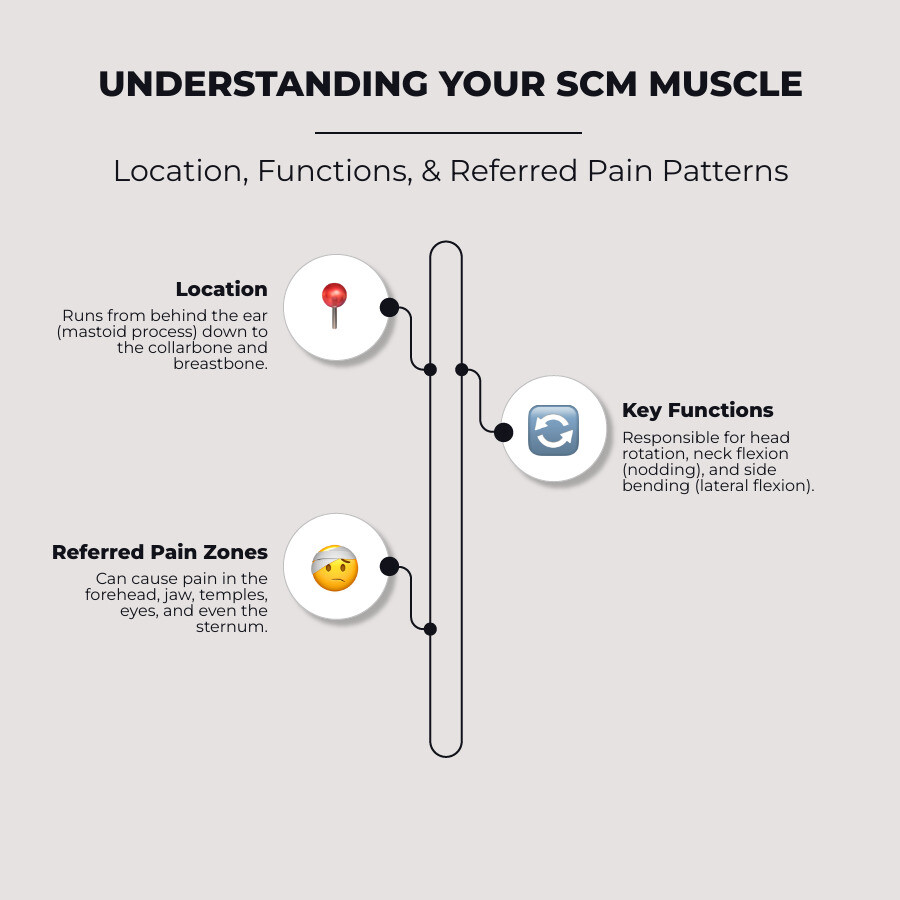
What is the Sternocleidomastoid (SCM) Muscle and What Does It Do?
The sternocleidomastoid (SCM) muscle is truly a marvel of engineering, playing a pivotal role in our daily movements and overall neck health. If you've ever felt the strong cords in the front of your neck when you turn your head, you've likely felt your SCM in action! It's the largest and most superficial muscle in the front of your neck, making it a critical anatomical landmark for healthcare professionals.

SCM Muscle Anatomy Explained
The SCM muscle gets its rather long name from its attachment points: the sternum (breastbone), clavicle (collarbone), and mastoid process (the bony lump behind your ear, at the base of your skull). It's a paired muscle, meaning you have one on each side of your neck, and each SCM has two distinct heads:
- Sternal Head: Originating from the top of your breastbone.
- Clavicular Head: Originating from the inner portion of your collarbone.
Both heads then merge and insert onto the mastoid process. This unique two-headed structure allows for a wide range of movements.
Innervation for the SCM primarily comes from the Accessory Nerve (Cranial Nerve XI), which is essential for its function. The muscle also receives its blood supply from branches of the external carotid artery, specifically the occipital and superior thyroid arteries.
A fun fact about the SCM's composition: our SCM muscle consists of parallel rows of muscular fibers, with about 60% being white anaerobic fibers and 40% red aerobic fibers. White fibers are powerful and tire quickly, while red fibers are less powerful but have greater endurance. Interestingly, the percentage of red fibers tends to increase with age, reflecting potential changes in muscle function over time. You can explore more about the Anatomy of the neck muscles.
Key Functions in Daily Movement
The SCM muscle is a multi-tasker, involved in several essential movements and functions:
- Turning Your Head: When one SCM contracts, it rotates your head to the opposite side. For example, your right SCM turns your head to the left.
- Nodding and Tilting: When both SCMs contract together, they can flex your neck forward (like nodding "yes"). If one contracts, it can tilt your head to the same side (lateral flexion).
- Stabilizing the Head: It helps maintain good posture and balance, especially when we're moving or performing tasks that require head stability.
- Role in Chewing and Swallowing: The SCM plays a supportive role in temporomandibular joint (TMJ) function. During chewing, the SCM muscles are stimulated, helping to stabilize the head for optimal jaw movement.
- Assisting Breathing: During strenuous activity or when we're having difficulty breathing, the SCM acts as an accessory muscle of respiration, helping to lift the breastbone and collarbone to facilitate inhalation. This is why issues like hyperventilation can sometimes lead to SCM strain.
Given its constant involvement in so many actions, it's no surprise that the SCM muscle can easily become a source of pain and discomfort when overused or stressed.
Understanding the Causes and Symptoms of Sternocleidomastoid Muscle Pain
Just like any other muscle in our body, the SCM isn't immune to pain. In fact, because of its central role in head and neck movement, it's particularly susceptible to strain and dysfunction. When we talk about sternocleidomastoid muscle pain, we're often looking at a combination of lifestyle factors, injuries, and even referred pain from tight spots called trigger points.

Common Causes of SCM Strain
Our modern lifestyles, unfortunately, are ripe with opportunities to strain our SCM muscles. Here are some of the usual suspects:
- Poor Posture: This is a big one. Think about "text neck" – constantly looking down at our phones or hunching over a computer. This forward head posture puts immense strain on the SCM, forcing it to work harder to keep our heads upright.
- Awkward Sleeping Positions: Waking up with a stiff neck? Sleeping on your stomach with your head turned to one side, or using an unsupportive pillow, can lead to prolonged SCM contraction and subsequent pain.
- Whiplash Injuries: Sudden, forceful movements of the head, such as those experienced in car accidents, can cause significant trauma to the SCM, leading to whiplash.
- Heavy Lifting: Improper lifting techniques, especially those that involve straining the neck, can overexert the SCM.
- Repetitive Head Turning: Activities like certain swimming styles (e.g., the crawl stroke), prolonged driving, or even occupations like violinists or painters who hold their head in awkward positions for extended periods, can lead to SCM overuse.
- Respiratory Issues: Chronic coughing from conditions like asthma, or acute respiratory infections like sinusitis or the flu, can cause the SCM to overwork as an accessory breathing muscle, leading to tension and pain.
- Jaw Clenching (Bruxism): The SCM is connected to TMJ function, and persistent jaw clenching or grinding can create tension that refers to or exacerbates SCM pain.
Understanding these common causes is the first step in prevention and relief. You can learn more about general muscle strain causes.
Typical Symptoms of Sternocleidomastoid Muscle Pain
The symptoms of SCM pain can be quite varied and sometimes surprising, as the pain often refers to other areas beyond the neck itself. We commonly see:
- Dull, Aching Pain in the Neck: This can be localized directly in the muscle, often described as a deep ache or a constant pressure.
- Tenderness: The SCM muscle can feel sensitive to touch or pressure, especially when palpated.
- Muscle Tightness or Stiffness: This is a classic sign, often resulting in reduced range of motion, making it difficult to turn or tilt your head.
- Headaches: SCM pain is a frequent contributor to tension-type headaches, often felt in the temples, forehead, or behind the eyes.
- Dizziness or Vertigo: This can be one of the more unsettling symptoms, as SCM dysfunction can affect our balance and spatial awareness.
- Nausea: Sometimes accompanying dizziness, nausea can be a referred symptom from SCM trigger points.
- Referred Pain: Pain can radiate to the ear, jaw, face, sinuses, and even the throat, making swallowing uncomfortable.
- Visual Disturbances: Blurred vision, watery eyes, or even eyelid drooping can be linked to SCM issues.
- Tingling or Numbness: While less common, nerve irritation from a severely tight SCM can sometimes lead to tingling in the face or head.
For more on how neck issues can impact your overall comfort, check out our guide on From Ache to Ease: Navigating Back and Neck Pain.
How SCM Trigger Points Cause Referred Pain
One of the most fascinating—and sometimes confusing—aspects of SCM pain is its ability to cause referred pain. This means the actual source of the pain (the SCM muscle) is felt in a completely different part of the body. This phenomenon is often due to myofascial pain syndrome, where highly irritable spots called trigger points develop within the muscle fibers.
The SCM has two main divisions, and trigger points in each can cause distinct referred pain patterns:
- Sternal Division Trigger Points: These are often responsible for a wide array of symptoms, including pain felt in the cheek, around the eye, in the jaw, at the sternum, or deep in the throat. They can also cause autonomic symptoms such as watery eyes, eye reddening, nasal congestion, or even sinusitis-like symptoms. We've even seen cases where trigger points here manifest as facial numbness or tingling.
- Clavicular Division Trigger Points: These tend to refer pain to the forehead, ear, and the area behind the ear (mastoid process). They are also strongly linked to balance problems, postural dizziness, and vertigo. A classic triad of dizziness, frontal headache, and dysmetria (lack of coordination) can be associated with trigger points in this area.
It's truly incredible how a muscle in your neck can impact so many seemingly unrelated areas! This is why a thorough understanding of SCM anatomy and its well-documented referred pain patterns is crucial for accurate diagnosis and effective treatment (Missaghi, 2004).
How to Find Relief: Treatments and Management Strategies
Once we understand the SCM muscle and the various ways it can cause pain, the next logical step is to explore how to find relief. The good news is that most cases of sternocleidomastoid muscle pain respond very well to a combination of at-home care and professional treatments. Our goal is always to reduce pain, restore mobility, and prevent future flare-ups.
At-Home and Self-Care Strategies
Many effective strategies for managing SCM pain can be implemented right from the comfort of your home. Consistency is key here!
- Rest: First and foremost, give your muscle a break. Avoid activities that aggravate your pain.
- Ice and Heat Therapy: For acute pain or inflammation (within the first 48 hours), apply ice packs for 15-20 minutes at a time. After 48 hours, or for chronic tightness, moist heat (like a warm shower or heating pad) can help relax the muscle and improve blood flow. Alternating between the two, ending with cold, can be particularly effective.
- Gentle Self-Massage: Using your fingertips, gently massage the SCM muscle from behind your ear down to your collarbone. You can pinch and release taut bands, or use gentle circular motions. A 2021 study revealed that massage and stretching of the sternocleidomastoid muscle significantly reduced pain and disability, while increasing range of motion and muscle endurance in individuals with chronic neck pain.
- Posture Correction: We can't stress this enough! Be mindful of your posture, especially when using digital devices. Hold your smartphone at eye level and set reminders to take breaks from prolonged computer use. Ensure your workstation is ergonomically set up.
- Ergonomic Adjustments: In your car, adjust your headrest to support your neck. At your desk, ensure your monitor is at eye level and your chair provides good lumbar support.
- Supportive Pillows: Choose a pillow that supports the natural curve of your neck. Sleeping on your back with a supportive, low-profile pillow, or on your side with a pillow that keeps your head and neck aligned, is generally recommended. Avoid sleeping on your stomach, as this forces your neck into a rotated position.
- Topical Pain Relief: For targeted, fast-acting relief, consider a high-quality topical cream designed for muscle aches. Products containing menthol, like Neuropasil, can provide a soothing, cooling sensation that helps alleviate discomfort. Menthol works by creating a cooling sensation that distracts from pain and can help relax muscles. Our Expert Guide to Topical Treatments for Muscle Aches and Why Does Menthol Help With Pain Relief? offer more insights.
Effective Stretches for Sternocleidomastoid Muscle Pain Relief
Stretching is a cornerstone of SCM pain relief, helping to lengthen tight muscles and improve flexibility. Always perform these gently and never push into pain.
-
SCM Side-Bend Stretch:
- Sit or stand tall, keeping your shoulders relaxed and down.
- Gently tilt your head to one side, bringing your ear towards your shoulder (e.g., right ear to right shoulder).
- Use the hand on the same side (e.g., right hand) to gently pull your head a little further, deepening the stretch on the opposite SCM (left SCM).
- For a deeper stretch, you can also gently rotate your head slightly upward towards the ceiling while tilted.
- Hold for 20-30 seconds, breathe deeply, and repeat 2-3 times on each side.
-
Chin-Tuck Exercise (Cervical Retraction):
- Sit or stand tall, looking straight ahead.
- Gently pull your chin straight back, as if making a double chin, keeping your head level. You should feel a stretch at the back of your neck.
- This helps improve forward head posture and strengthens deep neck flexors.
- Hold for 5-10 seconds, repeat 10-15 times.
-
Upper Trapezius Stretch:
- This muscle often works in conjunction with the SCM and can contribute to neck pain.
- Sit or stand, gently drop your left ear towards your left shoulder.
- Place your left hand on your head and gently assist the stretch.
- Place your right hand behind your back or hold onto the bottom of your chair to anchor your shoulder down.
- Hold for 20-30 seconds, repeat on the other side.
- For more details, see our guide on How to Do Upper Trap Stretches: The Right Way.
A 2021 study highlighted the effectiveness of combined SCM stretching and massage in reducing pain and disability, and increasing range of motion in chronic neck pain sufferers.
Professional Treatment Options
While self-care is important, sometimes professional help is needed, especially if pain is persistent or severe.
- Physical Therapy: A physical therapist can provide a comprehensive assessment, identify underlying causes, and design a personalized treatment plan. This may include manual therapy (hands-on techniques), therapeutic exercises to strengthen weak muscles and stretch tight ones, and modalities like ultrasound or electrical stimulation.
- Massage Therapy: Professional massage can release muscle tension, break up trigger points, and improve circulation in the SCM and surrounding neck muscles.
- Trigger Point Therapy: This specialized approach focuses directly on deactivating trigger points through techniques like ischemic compression (sustained pressure), pincer-grip massage, or even dry needling, which involves inserting a thin needle into the trigger point. A 2013 study published in the Journal of Orthopaedic & Sports Physical Therapy found that trigger point manual therapy provided significant reductions in neck pain and disability, highlighting its effectiveness (Llamas-Hernández et al., 2013).
- Chiropractic Care: Chiropractors focus on spinal alignment and nervous system function. They may use spinal adjustments, particularly in the cervical spine, to address SCM pain and improve overall neck mechanics.
- Medications: Over-the-counter pain relievers like NSAIDs (ibuprofen, naproxen) can help manage pain and inflammation. In some cases, a doctor might prescribe muscle relaxants for severe spasms.
For more comprehensive muscle strain treatment tips, check out our Top 7 Muscle Strain Treatment Tips.
When to See a Doctor for Neck Pain
While many cases of sternocleidomastoid muscle pain can be managed with self-care, it's crucial to know when to seek professional medical attention. Ignoring certain symptoms could lead to more serious complications.
Red Flag Symptoms You Shouldn't Ignore
We recommend consulting a healthcare provider if you experience any of the following red flag symptoms (Mayo Clinic, n.d.):
- Pain Following a Significant Injury: If your neck pain started after a fall, car accident (whiplash), or any other traumatic event.
- Numbness, Weakness, or Tingling in Arms: These symptoms could indicate nerve compression or damage, which needs immediate evaluation.
- Severe Headache with a Stiff Neck: Especially if accompanied by fever, this could be a sign of meningitis, a serious infection.
- Fever or Chills, Unexplained Weight Loss: These are systemic symptoms that could point to an underlying infection or other serious medical condition.
- Difficulty Swallowing or Breathing: While SCM pain can sometimes cause throat discomfort, persistent difficulty swallowing or breathing warrants urgent medical assessment.
- Persistent or Worsening Pain: If your pain doesn't improve with self-care after a week or two, or if it gets progressively worse.
- Loss of Sensation or Balance Issues: Any changes in sensation, coordination, or balance should be evaluated by a doctor.
While these aren't always direct signs of SCM issues, they are red flags that require a medical professional's diagnosis. For concerns about nerve-related pain, you might find our article on Pinched Nerve in the Lower Back helpful, as it touches on the importance of nerve health.
Conditions That Can Mimic SCM Pain
Because the SCM can refer pain so broadly, its symptoms can sometimes be mistaken for other conditions. A healthcare professional will consider these in a differential diagnosis:
- Cervical Radiculopathy (Pinched Nerve): Nerve compression in the neck can cause pain, numbness, or tingling that radiates down the arm, which can sometimes be confused with SCM referred pain.
- Carotid Artery Dissection: This is a rare but serious condition involving a tear in the wall of the carotid artery, often presenting with sudden, severe neck pain and headache.
- Lymph Node Swelling (Lymphadenopathy): Enlarged lymph nodes in the neck can cause localized pain and tenderness that might be confused with muscle pain.
- Torticollis: While SCM dysfunction can cause torticollis (wryneck), other forms of torticollis exist, including congenital, spasmodic, or ocular types, each with different causes.
- Thoracic Outlet Syndrome: This condition involves compression of nerves or blood vessels in the space between your collarbone and first rib, causing pain in the neck, shoulder, and arm.
- Temporomandibular Joint (TMJ) Disorder: As mentioned, SCM and TMJ are linked. TMJ disorders can cause jaw pain, headaches, and ear pain that overlap with SCM referred pain.
A proper diagnosis from a doctor or physical therapist is essential to rule out these other conditions, which are part of a standard differential diagnosis for neck pain, and ensure you receive the most appropriate treatment (Kallmes, 2022).
Frequently Asked Questions about SCM Pain
How long does it take for SCM pain to go away?
The recovery time for sternocleidomastoid muscle pain can vary significantly depending on the cause and severity. Minor muscle strains or tension from poor posture might resolve within a few days to a couple of weeks with consistent self-care. Moderate cases, especially those involving significant trigger points or minor injuries, could take a few months to fully recover, requiring dedicated treatment and rehabilitation. More severe cases, such as whiplash or chronic SCM syndrome, might take even longer, emphasizing the importance of addressing the root cause and adhering to a comprehensive treatment plan. With appropriate treatment, SCM pain usually goes away, but consistency in care and preventative measures is key.
Can SCM pain cause dizziness?
Yes, absolutely! SCM tension and trigger points are well-known culprits for causing dizziness, vertigo, and balance problems. The SCM muscle plays a role in our proprioception (our body's sense of position and movement) and its dysfunction can disrupt this delicate system. Specifically, trigger points in the clavicular head of the SCM are often linked to symptoms like postural dizziness, unsteadiness, and even a triad of dizziness, frontal headache, and dysmetria (lack of coordination). The link between the clavicular division of the SCM and these balance-related issues is well-established (Missaghi, 2004). If you're experiencing persistent dizziness along with neck pain, it's definitely something to discuss with a healthcare professional.
What is the best sleeping position for SCM pain?
The way we sleep can have a huge impact on our SCM muscles. To minimize strain and promote healing, we recommend:
- Sleeping on your back: This is often considered the best position as it maintains a neutral spinal alignment. Use a supportive, low-profile pillow that cradles your neck without propping your head too high.
- Sleeping on your side: If you're a side sleeper, use a pillow that keeps your head and neck aligned with your spine, preventing your head from tilting too far down or up.
- Avoid sleeping on your stomach: This position forces your neck into a rotated and extended position for hours, which is a major contributor to SCM pain and stiffness. If you absolutely cannot avoid stomach sleeping, try placing a thin pillow under your forehead to allow for some neutral head positioning.
Ensuring your pillow is adequate and your sleeping position is optimized can make a significant difference in preventing and relieving SCM pain.
Conclusion
Understanding and addressing sternocleidomastoid muscle pain is crucial for anyone experiencing persistent neck discomfort, headaches, dizziness, or referred pain to the face and shoulders. We've explored how this powerful neck muscle works, the many ways it can become strained or develop painful trigger points, and the diverse symptoms it can produce.
The good news is that proactive management, combining self-care strategies with professional treatments when needed, can lead to significant relief and improved quality of life. Prioritizing good posture, incorporating regular stretching into your routine, and being mindful of ergonomic adjustments in your daily environment are powerful preventative steps.
For targeted, fast-acting relief from muscle aches and pains, including those stemming from your SCM, we encourage you to explore topical solutions like Neuropasil. Our natural, menthol-infused creams are designed to soothe discomfort and support your body's healing process.
Don't let SCM pain dictate your comfort or limit your daily activities. Take charge of your neck health, listen to your body, and seek the right support to achieve lasting relief. Learn more about how to find the right topical solution for your needs with The Ultimate Guide to Muscle Relief Cream.
References
Bordoni B, Varacallo M. Anatomy, Head and Neck, Sternocleidomastoid Muscle. [Updated 2023 Jul 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532881/
Büyükturan B, et al. The effects of combined sternocleidomastoid muscle stretching and massage on pain, disability, endurance, kinesiophobia, and range of motion in individuals with chronic neck pain: A randomized, single-blind study. Musculoskelet Sci Pract. 2021 Oct;55:102415. Available from: https://pubmed.ncbi.nlm.nih.gov/34147954/
Cleveland Clinic. Sternocleidomastoid (SCM) Muscle. Last reviewed: 2023. Available at: https://my.clevelandclinic.org/health/body/24939-sternocleidomastoid-scm-muscle
Healthline. Sternocleidomastoid Pain: Causes, Treatment & Pain Relief. Available at: https://www.healthline.com/health/sternocleidomastoid-pain
Kallmes DF, et al. Neck Pain (Cervicalgia). [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557557/
Llamas-Hernández R, et al. Comparison of the short-term outcomes between trigger point dry needling and trigger point manual therapy for the management of chronic mechanical neck pain: a randomized clinical trial. J Orthop Sports Phys Ther. 2013 Nov;43(11):852-61. Available from: https://pubmed.ncbi.nlm.nih.gov/24175578/
Mayo Clinic. Neck pain. Available at: https://www.mayoclinic.org/symptoms/neck-pain/basics/when-to-see-doctor/sym-20050882
Medical News Today. Sternocleidomastoid (SCM) Muscle Pain: Causes, Symptoms, and Treatments. Available at: https://www.medicalnewstoday.com/articles/sternocleidomastoid-pain
Missaghi B. Sternocleidomastoid syndrome: a case study. J Can Chiropr Assoc. 2004 Jun;48(2):150-5. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1769463/
Necksolutions. SCM Muscle Treatment - Sternocleidomastoid Muscle. Available at: https://www.necksolutions.com/scm-muscle/
Verywell Health. Sternocleidomastoid Pain: Exploring Potential Causes and Relief Strategies. Available at: https://www.verywellhealth.com/sternocleidomastoid-pain-7104868













