Understanding Neuropathic Pain: What You Need to Know
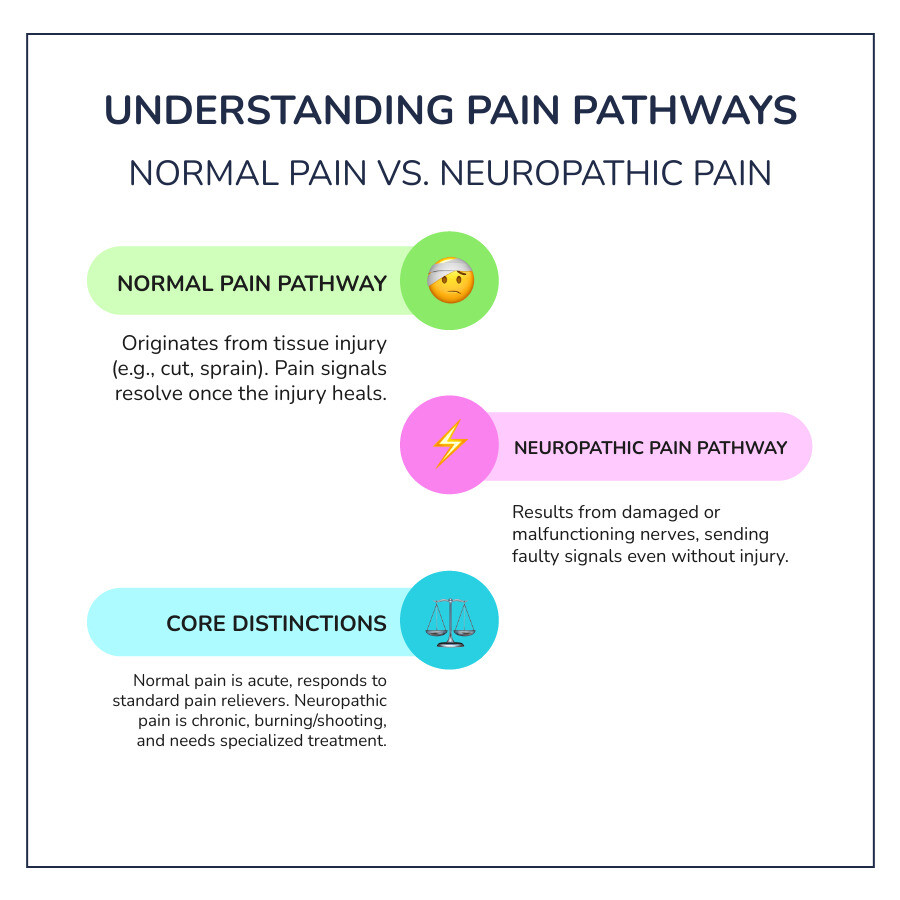
What is neuropathic pain? It's pain caused by damage or disease to the somatosensory nervous system—the network of nerves that sends sensory information from your body to your brain. Unlike regular pain from an injury like a cut or bruise, neuropathic pain comes from damaged nerves that send faulty signals, making your brain perceive pain even when there's no obvious injury.
Key Facts About Neuropathic Pain:
- Affects 7-10% of the general population, according to systematic reviews of population studies—that's millions of people experiencing nerve pain every day.
- Feels different from other pain types: burning, shooting, stabbing, or electric shock-like sensations.
- Can be chronic, lasting more than three to six months.
- Results from nerve damage in either the peripheral nervous system (nerves throughout your body) or central nervous system (brain and spinal cord).
- Common causes include diabetes, shingles, injuries, chemotherapy, stroke, and multiple sclerosis.
If you've ever felt a burning sensation in your feet, sharp shooting pain down your leg, or tingling that won't go away, you might be experiencing neuropathic pain. It's not just uncomfortable—it can significantly impact your quality of life, affecting sleep, work, exercise, and daily activities.
The challenge with nerve pain is that it's often more difficult to treat than regular pain. Standard pain relievers like ibuprofen or acetaminophen typically don't work well for it. That's because the pain isn't coming from damaged tissue—it's coming from the damaged nerves themselves, which are essentially "misfiring" and sending incorrect pain signals to your brain.
Painful diabetic neuropathy is the most common cause, accounting for nearly 30% of cases. But hundreds of other conditions can trigger nerve pain, from viral infections like shingles to physical trauma, vitamin deficiencies, and autoimmune diseases.
I'm Tony Enrico, and I've dedicated my work to helping people understand and manage what is neuropathic pain through effective, natural relief solutions. At Neuropasil, we've helped thousands of people find comfort and reclaim their active lives from persistent nerve pain.
What is Neuropathic Pain? A Deep Dive into Causes and Symptoms
What is neuropathic pain? It's a complex condition that arises when nerves themselves are damaged or dysfunctional. Instead of alerting your brain to a new injury, these compromised nerves send mixed, exaggerated, or outright false pain signals. Imagine a faulty alarm system that constantly blares, even when there's no fire. That's essentially what happens with neuropathic pain.
Our nervous system is divided into two main parts: the central nervous system (CNS), which includes your brain and spinal cord, and the peripheral nervous system (PNS), which consists of all the nerves extending from your spinal cord to the rest of your body—your limbs, organs, and skin. Damage to either of these systems can lead to neuropathic pain. When nerve fibers are damaged, they can change their function, becoming unusually sensitive and developing spontaneous, pathological activity. This can even lead to changes in your central nervous system, a phenomenon known as central sensitization, where your brain and spinal cord become hypersensitive to pain signals.
Common Causes and Risk Factors
Neuropathic pain isn't a disease itself, but rather a symptom of an underlying issue affecting the nerves. Many conditions and factors can lead to nerve damage, and unfortunately, some of them are quite common. Here are some of the most frequent culprits:
- Diabetes (Diabetic Neuropathy): This is by far the most common cause, accounting for nearly 30% of all neuropathic pain cases. High blood sugar levels over time can damage nerve fibers, especially in the feet and legs. Managing blood sugar is crucial for preventing and slowing the progression of diabetic neuropathy.
- Postherpetic Neuralgia (Shingles): After a shingles outbreak, some individuals experience persistent, severe nerve pain in the area where the rash occurred. This is due to damage to the nerves by the varicella-zoster virus.
- Trigeminal Neuralgia: This condition causes intense, sudden, and often debilitating facial pain, typically described as electric shock-like. It usually affects the trigeminal nerve in the face.
- Alcoholism: Chronic, heavy alcohol use can lead to alcoholic neuropathy, damaging peripheral nerves and causing pain, numbness, and weakness.
- Traumatic Injury: Direct physical trauma to a nerve, such as from an accident, surgery, or even repetitive strain, can result in neuropathic pain. Nerve impingement from disc herniation or carpal tunnel syndrome are common examples.
- Stroke: Damage to the brain from a stroke can sometimes lead to central post-stroke pain, a type of neuropathic pain originating in the central nervous system.
- Multiple Sclerosis (MS): This autoimmune disease affects the brain and spinal cord, and nerve damage from MS lesions can cause various forms of neuropathic pain.
- HIV Infection: HIV can directly damage nerves or lead to neuropathic pain as a side effect of certain antiretroviral medications.
- Vitamin Deficiencies: Lack of essential vitamins, particularly B vitamins (like B12 and thiamine), can impair nerve function and lead to neuropathy.
- Chemotherapy and Radiation: Cancer treatments like chemotherapy can cause chemotherapy-induced peripheral neuropathy (CIPN), damaging nerves and resulting in pain, tingling, and numbness. You can learn more about this by exploring scientific research on chemotherapy-induced peripheral neuropathy.
Typical Symptoms and Sensations
The sensations associated with neuropathic pain are often distinct from the aching or throbbing of regular tissue pain. They can be unpredictable, intense, and deeply unsettling. Here are some of the typical symptoms and sensations our clients describe:
- Burning or Shooting Pain: Many describe it as a constant, intense burning sensation, or sudden, sharp, shooting pains that travel along a nerve pathway.
- Stabbing Sensations: Quick, piercing pains, as if being jabbed with a sharp object.
- Tingling (Pins and Needles): A sensation of prickling or "pins and needles," often accompanied by numbness.
- Numbness: A loss of sensation in the affected area, which can paradoxically exist alongside pain.
- Allodynia (Pain from Non-Painful Stimuli): This is a hallmark of neuropathic pain, where something that shouldn't hurt—like a light touch, a cool breeze, or even the weight of clothing—causes severe pain.
- Hyperalgesia (Exaggerated Pain Response): An extreme or disproportionate pain reaction to a stimulus that would normally be only mildly painful.
- Itching: Persistent, intense itching that can be very irritating.
- Electric Shock-like Feelings: Sudden, brief, and intense sensations resembling an electric shock.
These sensations can significantly impact daily life, making simple tasks challenging and leading to sleep disturbances, anxiety, and depression.
Here's a list of common descriptive words for nerve pain that we often hear:
- Fiery
- Searing
- Stinging
- Gnawing
- Throbbing
- Radiating
- Freezing
- Sensitive
- Tender
- Jumping
- Needles
- Crawling
- Buzzing
How Neuropathic Pain is Diagnosed and Differentiated
Diagnosing neuropathic pain is crucial for effective treatment, but it can be a bit like detective work. Because the pain originates from damaged nerves rather than direct tissue injury, healthcare professionals need to carefully piece together clues from your medical history, symptoms, and various tests. Our goal is always to pinpoint the underlying cause and the specific nerves involved.
The diagnostic process typically begins with a thorough patient history. We'll ask you to describe your symptoms in detail: what the pain feels like, where it's located, when it started, what makes it better or worse, and how it impacts your daily life. Your symptom description is incredibly valuable in understanding the nature of your pain. This is followed by a physical examination and a neurological exam to assess your reflexes, muscle strength, balance, and sensitivity to touch, temperature, and vibration.
To further investigate, doctors may order several tests:
- Blood Tests: These can help identify underlying conditions like diabetes, vitamin deficiencies, autoimmune disorders, or infections that might be causing nerve damage.
- Nerve Conduction Studies (NCS): These tests measure how fast electrical signals travel through your nerves. Slowed signals can indicate nerve damage.
- Electromyography (EMG): Often performed alongside NCS, EMG measures the electrical activity of muscles in response to nerve stimulation, revealing nerve or muscle dysfunction.
- Skin Biopsy: For diagnosing small fiber neuropathy, a skin biopsy is often considered the gold standard. It involves taking a small sample of skin to examine the density of nerve fibers.

How is Neuropathic Pain Diagnosed by Professionals?
Healthcare professionals in New York City and beyond use a multi-pronged approach to diagnose neuropathic pain accurately. This involves not only the tests mentioned above but also specialized assessments:
- Screening Tools (Questionnaires): Doctors often use validated questionnaires like the Douleur Neuropathique 4 Questions (DN4), Leeds Assessment of Neuropathic Symptoms and Signs (LANSS), or painDETECT. These tools help identify the characteristics of neuropathic pain and differentiate it from other pain types.
- Sensory Testing: Quantitative Sensory Testing (QST) assesses your ability to feel different sensations (cold, heat, pressure, vibration) and helps identify specific sensory deficits or hypersensitivities, which can be crucial for phenotyping the pain and guiding treatment.
- Imaging Tests (MRI, CT Scan): While these don't directly show nerve damage, they can reveal structural issues that might be compressing or affecting nerves, such as herniated discs, spinal stenosis, tumors, or lesions in the brain or spinal cord.
- Identifying Underlying Cause: A key step is always to identify and, if possible, treat the underlying condition causing the nerve damage. For example, controlling blood sugar in diabetes or treating an infection.
- Differential Diagnosis: Doctors must differentiate neuropathic pain from other types of pain, as treatment approaches vary significantly. Conditions like fibromyalgia, which can have neuropathic-like symptoms but a different underlying mechanism, require careful consideration.
When to seek medical attention: If you experience persistent numbness, tingling, muscle weakness, uncontrolled twitching, or frequently drop objects, it's time to call your healthcare provider. For severe pain, numbness, or weakness that is rapidly worsening, or if you experience a fast or irregular heart rate, changes in bathroom habits, dizziness, or fainting, please go to the emergency room immediately. Early diagnosis and intervention can make a significant difference in managing neuropathic pain effectively.
Neuropathic vs. Nociceptive Pain: Understanding the Difference
To truly grasp what is neuropathic pain, it helps to understand how it differs from nociceptive pain, which is the more common type of pain we all experience.
| Feature | Neuropathic Pain | Nociceptive Pain |
|---|---|---|
| Source of Pain | Damage or disease to the somatosensory nervous system (nerves themselves). | Damage to body tissue (e.g., skin, muscles, bones, organs). |
| Sensation Type | Burning, shooting, stabbing, electric shock, tingling, numbness, pins and needles, itching, allodynia, hyperalgesia. | Aching, throbbing, sharp, dull, sore, pressure. |
| Duration | Often chronic (long-lasting, >3-6 months), may persist even after initial injury heals. | Usually acute (short-term), resolves when tissue heals. |
| Examples | Diabetic neuropathy, postherpetic neuralgia, trigeminal neuralgia, sciatica (from nerve compression). | Sprained ankle, cut finger, broken bone, headache, muscle strain, arthritis. |
| Purpose | Maladaptive response; nerves sending faulty signals. | Warning signal of potential or actual tissue damage. |
| Treatment | Often requires specialized medications (antidepressants, anticonvulsants), topical treatments, nerve blocks, physical therapy, neuromodulation. | Responds well to conventional pain relievers (NSAIDs, acetaminophen), rest, ice, heat. |
While nociceptive pain is your body's alarm system telling you to remove your hand from a hot stove, neuropathic pain is like a broken alarm that keeps ringing even when there's no danger, or rings when a feather touches it. Understanding this distinction is vital for effective treatment.
A Comprehensive Guide to Neuropathic Pain Management
Managing neuropathic pain is often a journey that requires patience, persistence, and a multifaceted approach. Because it's a complex condition, there's rarely a single "magic bullet." Instead, we believe in a multidisciplinary approach, combining various strategies custom to your unique needs. Our primary goals are to provide significant pain relief, maintain or improve your functionality, and ultimately improve your overall quality of life. An individualized management plan, developed in collaboration with your healthcare provider, is key.
Topical Relief Creams for Nerve Pain
For many individuals experiencing neuropathic pain, especially when it's localized, topical relief creams can be a game-changer. These creams offer targeted relief directly to the affected area with minimal systemic side effects, making them a valuable part of a comprehensive management plan.
At Neuropasil, we specialize in natural, fast-acting topical creams designed for nerve pain and sore muscles. Our unique formulations harness the power of ingredients like:
- Aloe: Known for its soothing and anti-inflammatory properties.
- Urea: Helps improve the penetration of other ingredients, keeping the skin hydrated and healthy.
- Menthol: Provides a cooling sensation that can distract from pain and offer temporary relief.
These ingredients work together to calm irritated nerves and reduce discomfort, providing a welcome respite from burning, tingling, and shooting pains. Many of our loyal customers find Neuropasil particularly effective for conditions like neuropathy, sciatica, fibromyalgia, plantar fasciitis, and general nerve pain in the feet, hands, and other areas. The benefit of fast-acting, targeted relief means you can apply the cream exactly where it hurts and often feel relief quickly, allowing you to get back to your daily activities with greater comfort.
Topical treatments are recognized by medical professionals as effective options for localized neuropathic pain. Research supports their use in managing symptoms, as highlighted in various studies, including scientific research on topical treatments for neuropathic pain. These treatments work in various ways, such as by providing a numbing effect or desensitizing nerve endings over time.
Supportive Therapies and Lifestyle Approaches
Beyond medications and topical solutions, integrating supportive therapies and healthy lifestyle choices can significantly improve your quality of life with neuropathic pain.
- Physical Activity: Gentle, regular exercise is incredibly beneficial. Activities like walking, swimming, or cycling can improve blood flow to nerves, strengthen muscles, and release natural pain-relrelieving endorphins. Always start slowly and consult your doctor or a physical therapist before beginning any new exercise regimen.
- Occupational Adjustments: Sometimes, modifying daily tasks or work environments can reduce nerve irritation. This might involve ergonomic adjustments, assistive devices, or changing how you perform certain movements.
- Relaxation Techniques: Stress can exacerbate pain. Techniques like deep breathing, meditation, and yoga can help calm the nervous system, reduce stress, and improve your ability to cope with pain.
- Psychological Therapies: Cognitive Behavioral Therapy (CBT) and other forms of psychotherapy can help you reframe your relationship with pain, develop coping strategies, and address associated anxiety or depression. These therapies are crucial because chronic pain often has a significant psychological component.
- Support Groups and Community Resources: Connecting with others who understand your experience can be immensely helpful. Support groups provide a safe space to share experiences, learn coping mechanisms, and feel less alone. While specific resources vary by location, seeking out local pain management clinics or community health centers in New York City can help you find appropriate support.
What is the Prognosis for Individuals with Neuropathic Pain?
The outlook for individuals living with neuropathic pain is highly variable. While a complete "cure" might not always be possible, especially if the underlying nerve damage is permanent, effective management is often achievable. Our focus is on significantly reducing symptoms and improving your daily functioning.
Neuropathic pain is generally not life-threatening, but its impact on quality of life can be profound. The best results often come from a combination of rehabilitation, medical interventions, and strong support for emotional, social, and mental well-being. By actively engaging in your treatment plan and making consistent lifestyle adjustments, many individuals can find substantial relief and lead fulfilling lives. Long-term management strategies typically involve ongoing monitoring, medication adjustments, and continued engagement with supportive therapies.
Lifestyle Changes and Self-Management Strategies
Taking an active role in managing your neuropathic pain through lifestyle changes can be incredibly empowering and effective. These strategies complement medical treatments and contribute significantly to your overall well-being.
- Regular Exercise: As mentioned, gentle physical activity is vital. Walking, stretching, and low-impact aerobics can improve circulation, reduce inflammation, and release natural pain relievers. Consistency is key, even if it's just a short walk each day.
- Balanced Diet: Eating a nutrient-rich diet with plenty of fresh fruits, vegetables, whole grains, and lean proteins supports nerve health and overall bodily function. Focus on anti-inflammatory foods.
- Blood Sugar Control (for Diabetics): If your neuropathic pain is diabetes-related, meticulous blood sugar management is paramount. Keeping blood glucose levels within a healthy range can prevent further nerve damage and may even improve existing symptoms.
- Stress Management Techniques: Chronic pain is a major stressor, and stress can intensify pain signals. Incorporate practices like meditation, deep breathing exercises, mindfulness, or yoga into your daily routine. These techniques can help calm your nervous system and improve your pain tolerance.
- Limiting Alcohol: Alcohol can be toxic to nerves and exacerbate neuropathic symptoms. Reducing or eliminating alcohol intake can significantly benefit nerve health.
- Quitting Smoking: Smoking impairs circulation, which can reduce blood flow to nerves and worsen nerve damage. Quitting smoking is one of the most impactful steps you can take for your nerve health.
- Protecting Affected Areas: If you have numbness or reduced sensation, especially in your feet, be extra vigilant to prevent injuries. Check your skin regularly for cuts, blisters, or sores, and wear protective footwear.
Potential Complications of Untreated Nerve Pain
Ignoring or inadequately treating neuropathic pain can lead to a cascade of negative consequences that extend far beyond physical discomfort.
- Impact on Quality of Life: Persistent pain can severely limit daily activities, hobbies, and social interactions, leading to a diminished sense of enjoyment and fulfillment.
- Depression and Anxiety: The constant, unpredictable nature of neuropathic pain can take a heavy toll on mental health. Many individuals with chronic pain experience high rates of depression and anxiety, and there's a bidirectional relationship where mental health issues can also worsen pain perception. Scientific research on chronic pain and mental health highlights this significant comorbidity.
- Sleep Disturbances: Pain often interferes with sleep, leading to insomnia and chronic fatigue. Poor sleep, in turn, can lower your pain threshold and exacerbate symptoms.
- Reduced Mobility: Pain and muscle weakness can make movement difficult and discourage physical activity, leading to a sedentary lifestyle, further deconditioning, and increased disability.
- Increased Risk of Injury Due to Numbness: Areas with numbness or reduced sensation are more vulnerable to unnoticed injuries, cuts, burns, or pressure sores, which can lead to infections or more serious complications.
Addressing neuropathic pain early and comprehensively is not just about relieving discomfort; it's about safeguarding your physical and mental health and preserving your ability to live a full and active life.
Frequently Asked Questions about Neuropathic Pain
We often hear similar questions from individuals seeking to understand and manage their nerve pain. Here are some of the most common ones:
Can neuropathic pain be cured?
For many forms of neuropathic pain, especially when nerve damage is extensive or long-standing, a complete "cure" in the sense of eliminating all pain permanently might not always be possible. However, this doesn't mean you have to live with severe, debilitating pain. The focus of modern treatment is on effective management: significantly reducing your symptoms, improving your functionality, and enhancing your overall quality of life. Sometimes, treating the underlying cause (like controlling diabetes) can lead to significant improvement or even remission of symptoms. With a comprehensive, individualized plan, many individuals achieve substantial relief.
Is walking good for neuropathic pain?
Yes, for most people, gentle walking and other forms of regular, low-impact exercise can be very beneficial for neuropathic pain. It helps improve circulation, which is vital for nerve health, strengthens muscles, and releases natural pain-relieving chemicals in your body. However, it's crucial to:
- Start slowly: Begin with short durations and gradually increase as tolerated.
- Listen to your body: Don't push through pain that feels sharp or worsening.
- Wear appropriate footwear: Especially if you have foot neuropathy, choose comfortable, supportive shoes.
- Consult a doctor or physical therapist: They can help design a safe and effective exercise program custom to your specific condition.
What does neuropathic pain feel like in the feet?
Neuropathic pain in the feet is one of the most common presentations, particularly with diabetic peripheral neuropathy. People often describe a range of distinct sensations:
- Burning: A constant, intense heat or searing sensation.
- Tingling: The classic "pins and needles" feeling.
- Numbness: A loss of sensation, often described as a "dead" or "heavy" feeling.
- Shooting or Stabbing Pains: Sudden, sharp pains that can feel like electric shocks.
- "Walking on Glass" Sensation: A common description for the feeling of extreme tenderness or sensitivity on the soles of the feet.
- Increased Sensitivity: Even light touch, like a bedsheet, can cause excruciating pain (allodynia).
These symptoms can vary in intensity and may be worse at night, significantly disrupting sleep and daily activities.
Conclusion
Understanding what is neuropathic pain is the first step toward effective management and reclaiming your quality of life. Unlike typical pain, it stems from damaged or dysfunctional nerves, sending confusing and often agonizing signals to your brain. While challenging, we've learned that a proactive, multimodal approach combining medical treatments, supportive therapies, and lifestyle adjustments can lead to significant relief.
At Neuropasil, we're dedicated to empowering you with knowledge and providing effective solutions. For those exploring topical relief options as part of their management plan, Neuropasil offers a natural, fast-acting cream designed to provide targeted, soothing relief for nerve pain. Don't let neuropathic pain define your life. By working closely with healthcare professionals in New York City and exploring all available tools, including advanced therapies and high-quality topical solutions, you can take control of your health and move towards a more comfortable, active future.













