Understanding What Is Neuropathy: A Condition Affecting Millions
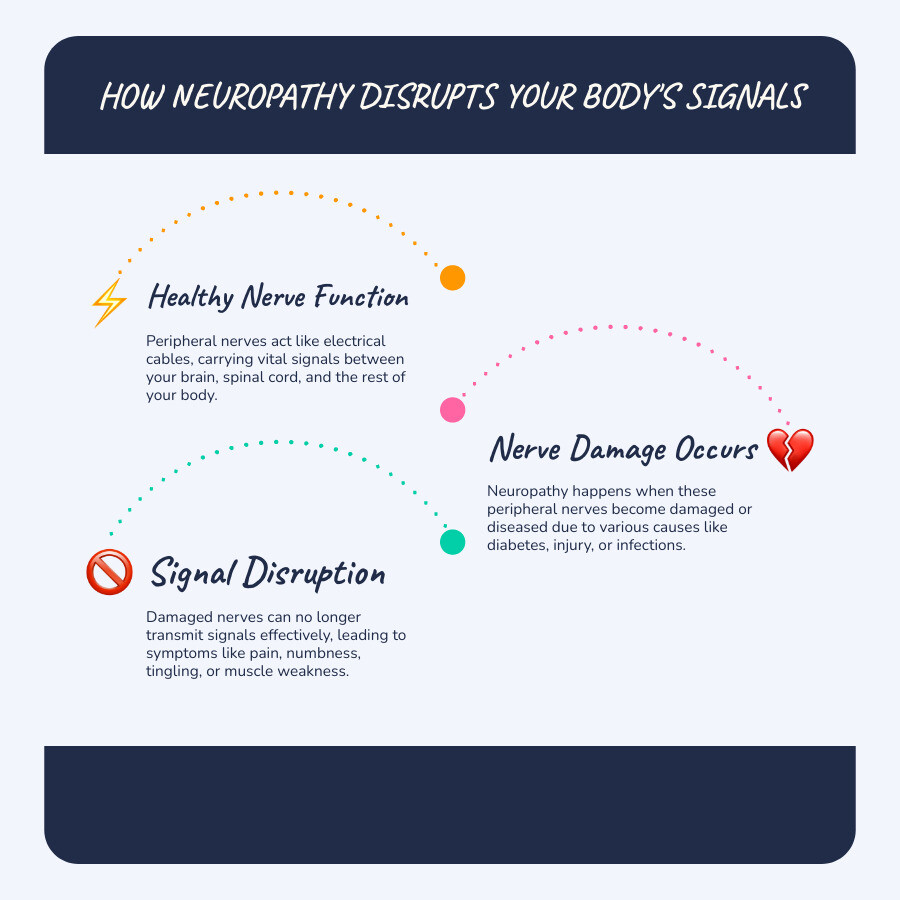
What is neuropathy? It's a condition that occurs when nerves outside your brain and spinal cord—your peripheral nervous system—become damaged or diseased [1]. This damage disrupts the normal communication between your brain and the rest of your body, leading to pain, numbness, tingling, or weakness, most commonly in your hands and feet.
Quick Answer:
- Definition: Nerve damage affecting the peripheral nervous system [2]
- Who it affects: An estimated 20 million Americans [2]
- Common symptoms: Burning pain, tingling, numbness, muscle weakness [3]
- Main causes: Diabetes, injury, infections, vitamin deficiencies, toxins [3]
- Types: Can affect sensory nerves (feeling), motor nerves (movement), or autonomic nerves (involuntary functions) [2]
If you're an athlete pushing through training, or someone dealing with persistent discomfort in your feet, legs, hands, or arms, understanding neuropathy is the first step toward finding relief. The condition isn't just one disease—it's an umbrella term covering over 100 different types of nerve disorders, each with its own causes and characteristics [2].
Your peripheral nerves act like electrical cables, carrying signals from your brain to every part of your body and back again. When these nerves are damaged, those signals get disrupted. You might feel pain when there shouldn't be any, lose sensation when you need it most, or experience weakness that affects your daily activities and athletic performance.
The good news? While neuropathy can be challenging, it's not a life sentence of suffering. Many forms are treatable, and with the right approach—from managing underlying conditions to finding effective symptom relief—you can regain control and get back to doing what you love.
I'm Tony Enrico, founder of Neuropasil, and I've dedicated my work to helping people understand what is neuropathy and find real relief from nerve pain. After seeing countless individuals struggle with this condition, I created Neuropasil to offer a natural, fast-acting solution that addresses nerve discomfort where it happens.
Common neuropathy vocab:
Understanding Neuropathy: What It Is and How It Feels
Think of your peripheral nervous system as your body's internal internet—a vast network of nerves branching out from your brain and spinal cord, constantly sending and receiving messages to keep you moving, feeling, and functioning. These nerves are the communication highways that let you feel the warmth of your morning coffee, walk without thinking about each step, and even regulate your heartbeat without conscious effort.
When we explore neuropathy more deeply, we're really talking about what happens when these communication lines get damaged. It's like having a phone line with static—messages might not get through at all, they might arrive garbled, or they might send false signals when nothing's actually happening. This nerve damage disrupts the smooth flow of information between your central nervous system and the rest of your body, leading to symptoms that can range from mildly annoying to seriously debilitating [1].
Neuropathy doesn't always show up the same way for everyone. Acute neuropathy comes on suddenly and progresses rapidly, while chronic neuropathy develops slowly over months or years, often so gradually that you might not notice it at first. The silver lining? Depending on what caused the damage and how severe it is, some forms of neuropathy can be reversible with proper treatment. However, it's important to understand that in many cases, especially when nerve damage is extensive, the condition may be permanent—making early detection and management absolutely crucial [2].

What is peripheral neuropathy and how does it affect the body?
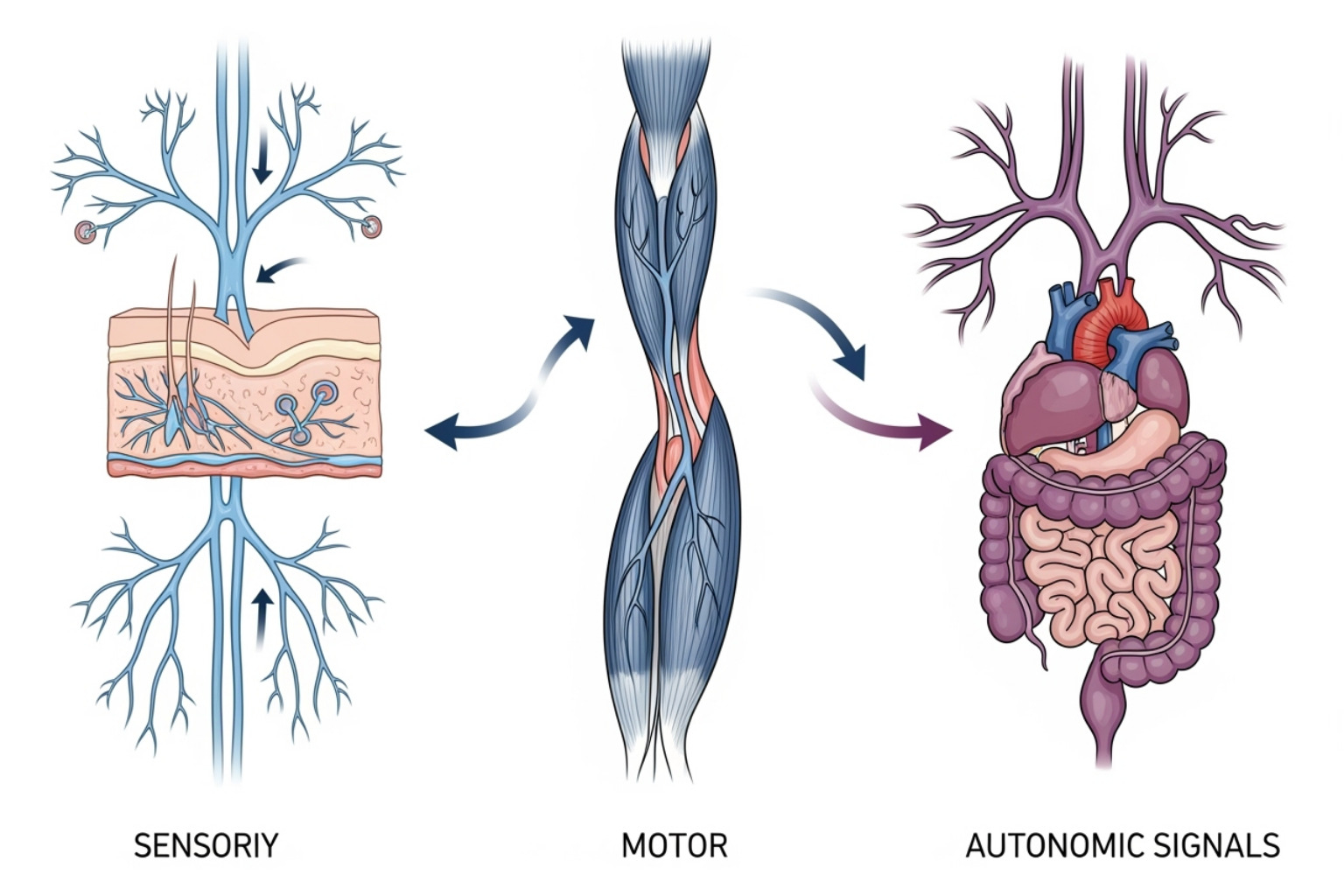
Your nerves aren't just simple wires—they're sophisticated messengers with different specialties. When peripheral neuropathy strikes, it can affect any of these three main nerve types, each with its own set of consequences [3].
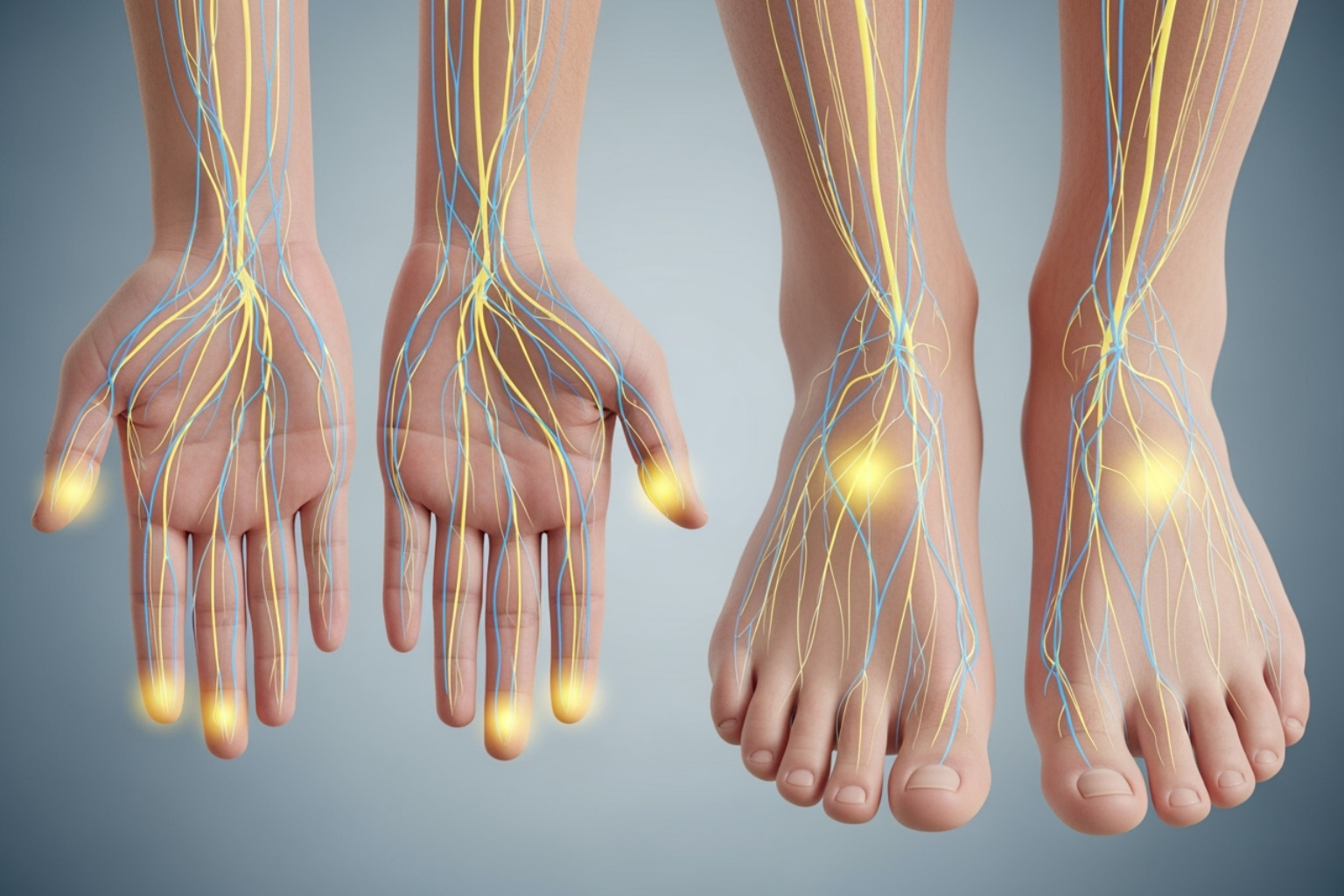
Sensory nerves are your body's information gatherers. They tell your brain about temperature, touch, pain, and vibration. When these nerves are damaged, the world literally feels different. You might lose the ability to feel hot or cold, making it dangerously easy to burn yourself on a stove or develop frostbite without realizing it. Some people describe it as wearing invisible gloves or socks—there's a barrier between them and the world they're trying to touch. Others experience the opposite problem: impaired sensation that makes even the lightest touch feel painful or uncomfortable. This loss of feeling is particularly risky in your feet, where you might not notice a cut, blister, or infection until it becomes serious [1, 2].
Motor nerves are the command center for movement. These nerves carry signals from your brain to your muscles, telling them when and how to move. When motor nerve damage occurs, you might notice your muscles feeling weak or unresponsive. Everyday tasks like climbing stairs, opening jars, or even maintaining your balance become challenging. Your muscles might cramp unexpectedly, or you might experience muscle wasting where your muscles actually shrink from lack of proper nerve signals. Some people develop "foot drop," where they can't lift the front part of their foot properly, causing them to shuffle or trip [2, 3].
Autonomic nerves are the behind-the-scenes operators, controlling all the body functions you don't consciously think about—your heart rate, blood pressure, digestion, sweating, and bladder control. When these nerves malfunction, the effects can be both uncomfortable and concerning. You might feel dizzy when you stand up too quickly because your blood pressure drops unexpectedly. Your digestive system might slow down, causing constipation or making you feel full after just a few bites. You might sweat excessively or not at all, struggle with bladder control, or experience other involuntary function problems that significantly impact your daily life [1, 3].
Understanding which nerve functions are affected helps you and your healthcare provider develop the right treatment approach for your specific situation.
Common Symptoms of Neuropathy
The symptoms of neuropathy are as individual as fingerprints—what you experience depends largely on which nerves are damaged and how severely. But certain warning signs appear frequently enough that they're worth knowing [1, 2, 3].
Numbness is often one of the first red flags. Many people describe feeling like their hands or feet have "fallen asleep" and never quite woken up. It's that "dead" sensation where you can't quite feel what you're touching or where your feet are on the ground.
Tingling sensations—often called "pins and needles"—can range from mildly irritating to genuinely distracting. Some describe it as a prickling or buzzing feeling, while others say it feels like insects crawling on their skin.
Burning pain is particularly common and often intensifies at night, making sleep difficult. This persistent, searing sensation can vary from mild warmth to severe, relentless fire-like discomfort that affects your quality of life.
Sharp or jabbing pain strikes suddenly and without warning, like electric shocks shooting through your limbs. These intense, stabbing sensations can make you freeze mid-movement.
Many people develop extreme sensitivity to touch, a condition called allodynia, where even the weight of bedsheets or the brush of clothing causes significant pain. It's a cruel irony—losing sensation in some ways while becoming hypersensitive in others.
Muscle weakness often creeps in gradually. You might find yourself dropping things more often, struggling with buttons or zippers, or feeling unsteady on your feet. This weakness can progress to lack of coordination, making you feel clumsy or increasing your risk of falls, especially in low light.
Foot problems deserve special attention because loss of sensation means injuries can go unnoticed. A small blister or cut that you don't feel can quickly become infected, leading to serious complications. This is why healthcare providers stress the importance of daily foot inspections for anyone with neuropathy.
Beyond these common symptoms, you might experience heat intolerance, abnormal sweating patterns, digestive issues like feeling full too quickly or experiencing constipation, and even bladder or bowel control problems when autonomic nerves are involved.
The bottom line? Neuropathy symptoms are more than just uncomfortable—they can genuinely interfere with your daily activities, your independence, and your overall quality of life. Recognizing these symptoms early and seeking proper treatment can make all the difference in managing the condition effectively.
The Many Faces of Neuropathy: Types and Classifications
When you're trying to understand what neuropathy is, one of the most eye-opening findies is just how many different forms this condition can take. We're not talking about a handful of variations—medical experts have identified over 100 distinct types of neuropathy [2]. That's a staggering number, but don't let it overwhelm you. The good news is that doctors have developed clear classification methods that help make sense of this complexity.
Think of these classification systems as helpful organizing tools. They group neuropathies based on which nerves are affected and how the damage manifests in your body. This isn't just academic—understanding the specific type of neuropathy you're dealing with often points directly to the underlying cause and helps guide the most effective treatment approach.
Types Based on Nerve Function
Your peripheral nervous system contains three distinct types of nerve fibers, each with its own specialized job. Neuropathy can target just one type or affect several simultaneously, which explains why symptoms vary so dramatically from person to person [3].
Sensory neuropathy affects the nerves that connect you to the world around you. These are your sensory nerves—the ones responsible for feeling touch, sensing temperature changes, detecting vibration, and registering pain. When these nerves are damaged, you might experience burning sensations, tingling that feels like pins and needles, numbness that makes your feet feel like blocks of wood, or even extreme sensitivity where the lightest touch becomes unbearable. The loss of protective sensations is particularly concerning because you might not notice when you've stepped on something sharp or burned your hand on a hot surface [1].
Motor neuropathy targets the nerves that control your muscles and movement. These motor nerves carry commands from your brain to your muscles, telling them when and how to contract. When they're damaged, the results can be frustrating and sometimes frightening—muscle weakness that makes climbing stairs exhausting, difficulty gripping objects firmly, cramps that strike without warning, visible muscle wasting, or involuntary twitching. Some people develop foot drop, where the front of the foot drags on the ground while walking because the muscles can't lift it properly [2].
Autonomic neuropathy is often the most unsettling type because it affects functions you normally don't think about. Your autonomic nerves run on autopilot, controlling your heart rate, blood pressure, digestion, sweating, bladder function, and sexual response. When these nerves malfunction, the consequences can range from annoying to dangerous. You might feel dizzy when standing up as your blood pressure drops suddenly, experience digestive issues like feeling full after just a few bites, have trouble controlling your bladder, notice your heart racing or beating irregularly, or find that you're sweating far too much or not at all. Because these nerves control vital body functions, autonomic neuropathy requires careful medical attention [3].
Many people experience combination neuropathy, where damage affects more than one nerve type simultaneously. This is actually quite common, particularly in conditions like diabetes, where you might have both sensory symptoms (numbness and pain) and motor symptoms (weakness and coordination problems) affecting the same areas [26].
Types Based on Nerves Affected
Another way to classify neuropathy is by looking at the pattern and distribution of nerve damage. This classification helps doctors understand whether you're dealing with isolated nerve compression or a more widespread condition.
Mononeuropathy means that just one single nerve has been damaged. This often happens when a nerve gets compressed, trapped, or injured in a specific location. If you've ever heard of Carpal Tunnel Syndrome, that's a perfect example of mononeuropathy—the median nerve running through your wrist gets squeezed in the narrow carpal tunnel, causing numbness, tingling, and pain in your thumb, index, middle, and part of your ring finger [29]. Ulnar neuropathy is another common mononeuropathy, affecting the ulnar nerve that runs from your neck down through your elbow to your hand. You might know this as "hitting your funny bone," though chronic ulnar nerve compression is no laughing matter [24]. These localized nerve problems often respond well to treatment once the source of compression is identified and addressed.
Polyneuropathy is the most widespread form of neuropathy and affects multiple nerves throughout your body. What makes polyneuropathy distinctive is its symmetrical pattern—if your right foot is affected, your left foot typically is too. The symptoms usually follow what doctors call a "stocking-and-glove" distribution because they start in your feet and hands—the areas farthest from your spinal cord where the nerves are longest. As the condition progresses, symptoms gradually move upward, like pulling on stockings or gloves. This length-dependent pattern happens because longer nerve fibers are more vulnerable to damage. Diabetic neuropathy is the most common type of polyneuropathy, affecting more than half of people living with diabetes [26].
Understanding which type of neuropathy you're dealing with isn't just about putting a label on your symptoms. It's about creating a roadmap for your treatment journey, whether that involves managing an underlying condition like diabetes, addressing a physical compression issue, or finding effective symptom relief through options like physical therapy, lifestyle changes, or topical nerve pain relief cream that can provide soothing comfort right where you need it most.
Uncovering the Roots: Causes and Risk Factors of Neuropathy
Here's something that can be both frustrating and enlightening about what is neuropathy: sometimes, despite every test and examination, doctors simply can't pinpoint what's causing it. This is called idiopathic neuropathy, and it happens more often than you might think. But in most cases, there's a clear culprit—or sometimes several—behind the nerve damage [2].
Neuropathy generally falls into two broad categories. There's acquired neuropathy, which develops during your lifetime due to illness, injury, or exposure to harmful substances. Then there's hereditary neuropathy, which is passed down through families in your genes. Understanding which category you fall into can make a significant difference in how your neuropathy is managed [19].
If you're looking for a comprehensive breakdown of all the possible causes and risk factors, the Peripheral Neuropathy Fact Sheet from NIH offers an excellent, trustworthy resource [2].
The Critical Role of Diabetes in Neuropathy
When we talk about the causes of neuropathy, one condition towers above all others: diabetes. In fact, diabetic neuropathy is the single most common form of nerve damage, affecting a staggering number of people. The statistics tell a sobering story—more than half of all people with diabetes will eventually develop some type of neuropathy [26].
So why does diabetes wreak such havoc on our nerves? The answer lies primarily in prolonged exposure to high blood sugar levels, also called hyperglycemia. When glucose levels remain elevated over time, several damaging processes kick into gear. First, excess sugar damages the tiny blood vessels that supply oxygen and vital nutrients to your nerves. Starved of what they need to survive, these nerves begin to malfunction and eventually die [27].
But there's more to the story. High blood sugar also triggers something called glycation—a process where sugar molecules latch onto proteins and fats in your body, forming harmful compounds known as advanced glycation end products, or AGEs. These AGEs accumulate in nerve tissues and blood vessel walls, causing inflammation and further damage. Scientific research has shown just how significant these AGEs are in the development and progression of diabetic neuropathy [4, 5].
The damage typically shows up first in the longest nerves—those reaching your feet and hands. This creates the classic "stocking-glove" pattern of symptoms, where numbness, tingling, and burning pain start in your toes and fingers before potentially spreading upward. Diabetic neuropathy can also attack your autonomic nerves, leading to problems with digestion, blood pressure regulation, and sexual function [26].
Here's the good news: blood sugar control is your most powerful weapon against diabetic neuropathy. Keeping your glucose levels within target ranges can prevent nerve damage from starting and slow its progression if it's already begun. It's not always easy, but it's absolutely worth the effort [26].
What are the other underlying causes of neuropathy?
While diabetes takes the spotlight, it's far from the only cause of nerve damage. Your nerves can be affected by a surprisingly wide range of factors, each with its own story [2, 3].
Physical injury or trauma can damage nerves in obvious ways—a car accident, a bad fall, or a sports injury can directly tear or crush nerve fibers. But damage can also happen more gradually. Repetitive motions, like typing for hours each day, can lead to conditions like Carpal Tunnel Syndrome [29]. Even something as simple as sitting in an awkward position for too long can compress nerves enough to cause problems.
Your diet matters more than you might think. Vitamin deficiencies can starve your nerves of what they need to function properly. Vitamin B12 is particularly crucial—it helps maintain the protective coating around nerve fibers called myelin. Without enough B12, that coating breaks down, and nerve signals get scrambled. Deficiencies in vitamins B1, B6, and E, as well as copper, can all contribute to nerve damage. This is one reason why chronic alcohol abuse often leads to neuropathy—not just from alcohol's direct toxic effects, but also because it interferes with nutrient absorption [2].
Sometimes, your own immune system becomes the problem. In autoimmune diseases like Lupus, Rheumatoid Arthritis, Sjögren's syndrome, and Guillain-Barré syndrome, your body's defense system mistakenly identifies nerve tissue as a threat and attacks it. Chronic Inflammatory Demyelinating Polyneuropathy (CIDP) and vasculitis (inflammation of blood vessels that reduces blood flow to nerves) work the same way, creating nerve damage through friendly fire [2, 3].
Infections can also target your nerves directly or trigger immune responses that cause collateral damage. Shingles, caused by the reactivation of the chickenpox virus, can lead to postherpetic neuralgia—a particularly painful form of nerve damage. HIV/AIDS, Lyme disease, Hepatitis B and C, leprosy, and diphtheria can all cause various types of neuropathy [2, 28].
When your kidneys or liver aren't working properly, toxins that should be filtered out of your blood start to accumulate. These toxins can poison your nerves, and the metabolic imbalances that come with organ disease can impair nerve function in multiple ways [3].
Speaking of toxins, exposure to heavy metals like lead, mercury, and arsenic can directly harm nerve tissue. Industrial chemicals and certain environmental toxins (Agent Orange is a notorious example) can do the same. Even some medications that are meant to help you can inadvertently damage nerves. Chemotherapy drugs are particularly notorious for causing chemotherapy-induced peripheral neuropathy (CIPN), which can be a debilitating side effect of cancer treatment [30]. Fluoroquinolone antibiotics have also been linked to peripheral neuropathy in some patients.
Chronic alcohol abuse creates a perfect storm for nerve damage—the alcohol itself is toxic to nerves, and heavy drinking typically comes with poor nutrition and vitamin deficiencies that make things worse [2].
For some people, neuropathy is written into their genes. Hereditary disorders like Charcot-Marie-Tooth disease (the most common inherited neurological disorder) are passed down through families, affecting sensory and motor nerves in the arms and legs [2].
Even tumors—both cancerous and benign—can cause neuropathy, either by physically pressing on nerves or by triggering something called paraneoplastic syndromes, where your immune system's reaction to the tumor ends up attacking nerve tissue. And hypothyroidism (an underactive thyroid) can also contribute to nerve problems [3].
The sheer variety of causes behind what is neuropathy shows why getting a proper diagnosis is so important. Identifying the specific trigger in your case isn't just about satisfying curiosity—it's the key to finding the right treatment approach and preventing further damage.
What is Neuropathy Diagnosis and Treatment?
Once you understand what is neuropathy and recognize its symptoms, the next crucial step is getting an accurate diagnosis and finding effective ways to manage it. The journey toward relief focuses on two essential goals: identifying and treating the root cause when possible, and managing the often-challenging symptoms that interfere with daily life. Whether you're an athlete dealing with nerve pain or someone struggling with persistent discomfort, know that there are paths forward to reclaim your quality of life.
How is Neuropathy Diagnosed?
Getting to the bottom of neuropathy requires detective work. Because nerve pain symptoms can mimic other conditions and stem from so many different causes, your doctor will take a thorough, systematic approach to figure out exactly what's happening in your body [6].
Your appointment will likely start with a detailed conversation about your medical history. Your doctor will want to know when your symptoms began, what they feel like, what makes them better or worse, and whether they've changed over time. They'll ask about your overall health, any existing conditions like diabetes, medications you're taking, your family's health history (since some neuropathies run in families), your diet, and lifestyle factors like alcohol use or exposure to chemicals or toxins at work.
Next comes the physical and neurological exam. Your doctor will check your reflexes, test your muscle strength and tone, assess your balance and coordination, and evaluate your ability to feel different sensations—light touch, temperature changes, and vibration. This hands-on examination helps pinpoint which nerves might be affected and reveals the pattern of nerve damage, which can be a valuable clue.
Blood tests are usually next on the list. These simple tests can uncover many underlying causes of neuropathy. Your doctor might check your blood sugar levels to screen for diabetes, look for vitamin deficiencies (especially B12, B6, and E), test for markers of autoimmune diseases, evaluate your kidney and liver function, check thyroid hormone levels, and even screen for exposure to heavy metals or other toxins [2, 3].
When it comes to nerve function tests, two often work together. An Electromyography (EMG) measures the electrical activity in your muscles when they respond to nerve signals, helping determine whether muscle weakness comes from nerve damage or a muscle problem. A Nerve Conduction Study (NCS) measures how quickly electrical signals travel through your nerves. If signals are traveling slowly, it might indicate damage to the protective myelin sheath around nerves. If the signal strength is reduced, it suggests the nerve fibers themselves are damaged [1].
In some cases, your doctor might recommend a nerve biopsy, where a tiny sample of nerve tissue is removed and examined under a microscope. This can reveal the specific type of nerve damage and sometimes point to the underlying cause. A skin biopsy offers another diagnostic option, particularly useful for detecting damage to small nerve fibers that standard EMG and NCS tests might miss. This is especially helpful for diagnosing small fiber neuropathies [2].
Sometimes imaging tests like MRI or CT scans help complete the picture, revealing nerve compression, tumors, or other structural problems affecting your nerves or spinal cord [18].
Early and accurate diagnosis makes all the difference. As highlighted in a practical approach to diagnosis, a thorough evaluation is the foundation of effective management [6]. When you identify the cause, you can target treatment to not only manage symptoms but potentially stop the progression—and sometimes even reverse the nerve damage.
Available Treatment Options for Managing Symptoms
Once you have a diagnosis, treatment becomes a two-pronged approach: addressing the underlying cause when possible, and managing the symptoms that are making your life difficult, particularly nerve pain.
Treating the underlying cause offers the best long-term results. For diabetic neuropathy, maintaining tight blood sugar control is absolutely essential [26]. If vitamin deficiencies are causing your neuropathy, supplements can make a remarkable difference. Autoimmune diseases might require immune-suppressing medications to stop your body from attacking its own nerves. If exposure to toxins or certain medications is the culprit, eliminating that exposure or switching medications can halt further damage. Infections need appropriate treatment with antibiotics or antivirals. And when nerve compression is the problem—like in carpal tunnel syndrome—physical therapy or sometimes surgery can relieve the pressure and restore function [29].
Managing neuropathic pain is often the most challenging part of treatment, because nerve pain doesn't respond well to regular pain relievers. However, you have several options. Certain antidepressants, including tricyclic antidepressants like amitriptyline and nortriptyline [7, 8], as well as SNRIs like duloxetine and venlafaxine [9], can relieve neuropathic pain even if you're not depressed. They work by changing how your brain processes pain signals.
Anticonvulsant medications, originally developed for epilepsy, have proven highly effective for many types of nerve pain. Gabapentin and pregabalin are the most commonly prescribed [10, 11], though others like oxcarbazepine and lamotrigine are also options. These medications calm overactive nerves that are sending pain signals when they shouldn't.
Opioids like tramadol or oxycodone can be effective for severe pain, but doctors typically reserve them for short-term use or truly intractable pain because of concerns about dependence and side effects [12].
Topical treatments offer another avenue for relief, delivering medication directly where you hurt. Lidocaine patches can numb the affected area, while capsaicin cream (made from chili peppers) can reduce pain signals over time, though it might cause an initial burning sensation [13].
For those seeking a natural, fast-acting solution, our Neuropasil Nerve Pain Relief Cream provides targeted relief right where you need it. We've formulated it with natural ingredients that work together: menthol for a cooling, soothing sensation, aloe for its anti-inflammatory properties, and urea to help the beneficial ingredients penetrate your skin and reach the inflamed nerves beneath. Athletes use it to recover from intense training, and people with conditions like sciatica and fibromyalgia rely on it for daily comfort. You can learn more about our Nerve Pain Relief Cream and how it might help you get back to doing what you love.
Physical therapy plays a vital role in managing neuropathy. A skilled therapist can help you improve strength, balance, flexibility, and coordination. They might also recommend braces, splints, or special orthopedic shoes to help you move safely and prevent injuries. Some people find relief with Transcutaneous Electrical Nerve Stimulation (TENS), which uses mild electrical currents to block pain signals, though the research on its effectiveness shows mixed results [14].
Living with chronic nerve pain affects more than just your body—it takes an emotional toll too. Psychological therapies like counseling, cognitive behavioral therapy, and stress management techniques can help you cope with pain and maintain a positive outlook. Some people also find complementary approaches like acupuncture, massage, or tai chi helpful, though the evidence for these varies.
Surgery becomes an option when nerve compression is the problem. Carpal tunnel release surgery, for example, can relieve pressure on the median nerve and restore function. However, surgery isn't helpful for most types of widespread neuropathy, where the nerve damage is scattered throughout the body rather than concentrated in one compressed area.
Finally, lifestyle modifications can make a real difference in how you feel day to day. Eating a balanced, nutritious diet supports nerve health (and if gluten sensitivity is causing your neuropathy, a strict gluten-free diet can be remarkably effective). Regular, gentle exercise improves circulation and often reduces pain. And avoiding smoking and excessive alcohol is crucial, as both can worsen nerve damage [1, 2].
The truth is, managing neuropathy usually requires combining several approaches—medications, topical treatments, physical therapy, and lifestyle changes—to get the best results. What works perfectly for one person might not work as well for another, so be patient as you and your healthcare team find the right combination for you.
Living With, Preventing, and Differentiating Neuropathy
When you're navigating life with neuropathy, it becomes clear pretty quickly that this isn't something you can just ignore and hope goes away. It requires attention, adjustments, and a proactive approach to managing your health. There's a lot you can actually do to minimize symptoms and prevent further damage. And while not every case of neuropathy can be prevented, especially those inherited forms that run in families, many acquired neuropathies can be avoided or at least slowed down significantly with the right strategies.
Can Neuropathy Be Prevented?
The honest answer is: sometimes yes, sometimes no. But even when prevention isn't entirely possible, you can often influence how quickly the condition progresses and how severe your symptoms become.
Managing your existing medical conditions is absolutely the most powerful tool in your prevention toolkit. If you have diabetes, keeping your blood sugar levels in a healthy range isn't just good advice, it's the single most effective way to prevent or delay diabetic neuropathy from developing or worsening [26]. Similarly, if you're dealing with kidney disease, liver disease, autoimmune conditions, or hormonal imbalances, effectively managing these conditions can stop them from progressing to the point where they damage your nerves [3].
What you eat matters more than you might think. A balanced diet rich in fruits, vegetables, whole grains, and lean protein provides the vitamins and nutrients your nerves desperately need to stay healthy. Specifically, ensuring you get enough B vitamins (especially B1, B6, and B12), vitamin E, and copper is crucial for nerve function [2]. If you're vegetarian or vegan, pay extra attention to your B12 intake, you might need fortified foods or supplements since B12 is primarily found in animal products.
Getting regular exercise doesn't just help with weight management and cardiovascular health, it directly benefits your nerves too. Moderate exercise for 30 minutes to an hour, at least three times a week, improves blood flow to your nerves, strengthens muscles, and can actually reduce pain [1]. Just check with your healthcare provider before starting any new exercise program, especially if you're already experiencing neuropathy symptoms.
Avoiding toxins is another critical step. This means minimizing your exposure to industrial chemicals, heavy metals like lead and mercury, and other environmental toxins that are known nerve damagers [2]. If you work in an environment where you're exposed to these substances, make sure you're following proper safety protocols.
Limiting alcohol consumption can make a real difference. Excessive drinking is a well-established cause of neuropathy, so reducing or eliminating alcohol from your life can prevent or slow nerve damage. There's no getting around this one, alcohol is genuinely toxic to nerves over time [2].
For anyone at risk of neuropathy, especially if you have diabetes, diligent foot care becomes non-negotiable. Inspect your feet every single day for cuts, blisters, or sores that you might not feel due to numbness. Wear comfortable, well-fitting, closed-toe shoes to protect your feet from injury. And treat even the smallest injuries promptly to prevent infection. What might seem like a minor scrape to someone else could become a serious problem when you have neuropathy [26].
Finally, staying current with vaccinations, like the shingles vaccine, can prevent infections that might lead to nerve damage. It's a simple step that can save you from a lot of potential pain down the road [2].
Potential Complications and Distinctions
Here's the reality: untreated or poorly managed neuropathy can lead to some serious complications that go way beyond discomfort. Understanding these risks isn't meant to scare you—it's meant to motivate you to take your condition seriously and work with your healthcare team to manage it effectively.
Foot ulcers and infections are perhaps the most common and dangerous complication, particularly for people with diabetes. When you lose sensation in your feet, you might not notice a small cut or blister. That minor injury can become infected, and because you still can't feel it, the infection can spread. In severe cases, this can lead to tissue damage, gangrene, and even amputation. This is why that daily foot inspection we mentioned earlier is so incredibly important [26].
Falls and injuries become much more likely when neuropathy affects your balance and coordination. Muscle weakness, lack of coordination, and loss of sensation in your feet can make you unsteady, greatly increasing your risk of falling. Falls can lead to fractures and other serious injuries, especially as we age. Simple home modifications, like installing handrails, ensuring rooms are well-lit, and removing tripping hazards, can help reduce this risk [1, 3].
Chronic pain from neuropathy can be absolutely debilitating. It's not just about the physical discomfort—persistent pain disrupts your sleep, contributes to anxiety and depression, and makes it difficult to participate in activities you once enjoyed. The cumulative effect on your mental health and overall well-being can be profound.
When autonomic nerves are severely affected, complications can become life-threatening. We're talking about dangerous heart rhythm disturbances, severe blood pressure fluctuations, and profound digestive issues. These aren't just inconveniences—they can require immediate medical attention [2, 3].
It's also worth understanding how neuropathy differs from other nerve-related conditions. People often confuse neuropathy, neuralgia, and radiculopathy because they all involve nerve problems, but they're actually distinct conditions:
| Feature | Neuropathy | Neuralgia | Radiculopathy |
|---|---|---|---|
| What it is | Damage to peripheral nerves throughout the body [1, 2, 3] | Severe, shooting pain along a specific nerve pathway | Nerve root compression near the spinal cord |
| Location | Usually affects hands and feet symmetrically | Follows the path of one specific nerve | Radiates along the nerve from the spine |
| Pain type | Burning, tingling, numbness, varied sensations | Sharp, shooting, electric shock-like pain | Sharp pain radiating down an arm or leg |
| Common causes | Diabetes, vitamin deficiencies, toxins, infections [2, 3] | Nerve irritation or damage, shingles [2] | Herniated disc, spinal stenosis, bone spurs |
| Examples | Diabetic neuropathy, chemotherapy-induced neuropathy [26, 30] | Trigeminal neuralgia, postherpetic neuralgia [2] | Sciatica, cervical radiculopathy [1] |
Understanding these distinctions helps you communicate more effectively with your healthcare provider and ensures you're getting the right treatment for your specific condition. What is neuropathy becomes clearer when you can distinguish it from these related but different nerve disorders.
The bottom line? Living with neuropathy requires vigilance, but it doesn't mean giving up on quality of life. With proper management, lifestyle adjustments, and the right support—including effective symptom relief options like Neuropasil Nerve Pain Relief Cream—you can maintain your independence and continue doing the things you love.
Understanding Neuropathy: What It Is and How It Feels
Think of your peripheral nervous system as the body's electrical wiring—a vast, intricate network branching out from your brain and spinal cord to every corner of your body. These nerves are constantly at work, carrying messages that let you feel a warm cup of coffee in your hands, walk without thinking about each step, and even digest your lunch without conscious effort. When we discuss what is neuropathy, we're talking about what happens when this essential wiring gets damaged.
When nerves are damaged, communication breaks down in ways that can feel deeply unsettling. Sometimes the signals simply don't get through—you might lose feeling in your feet or struggle to move your fingers with your usual dexterity. Other times, damaged nerves send false alarms, creating burning pain or tingling sensations when nothing is actually wrong. It's like having faulty wiring that either fails to turn on the lights or flickers constantly even when the switch is off.
Neuropathy can appear suddenly, developing over days or weeks (what we call acute neuropathy), or it might creep up slowly over months or years (chronic neuropathy). The progression often depends on what's causing the nerve damage in the first place. Here's something encouraging: depending on the underlying cause and how quickly it's addressed, some forms of neuropathy can actually improve or even reverse. However, if left untreated for too long, the damage can become permanent, which is why recognizing the signs early matters so much.
What is peripheral neuropathy and how does it affect the body?
To understand how peripheral neuropathy affects your body, it helps to know that your nerves aren't all the same—they're specialists, each with distinct jobs to do.
Sensory nerves act as your body's information gatherers. They're constantly reporting back to your brain about what's happening in the outside world: Is that surface hot or cold? Rough or smooth? Is there pressure on your foot? When these nerves are damaged, the world can feel muted or distorted. You might lose the ability to feel temperature changes, making it dangerously easy to burn yourself without realizing it. Or you might lose the protective sensation that normally warns you of an injury—many people with sensory neuropathy develop foot wounds without ever feeling the initial cut or blister. Paradoxically, damaged sensory nerves can also become hyperactive, sending intense pain signals even when there's nothing physically wrong. This creates that characteristic burning, tingling, or electric shock sensation that so many people with neuropathy describe.
Motor nerves are your body's action cables, carrying commands from your brain to your muscles for every voluntary movement you make. When motor nerve damage occurs, those commands get disrupted. Your muscles might not receive the signals they need, leading to weakness that makes gripping a coffee mug, climbing stairs, or even walking across a room feel exhausting. You might notice your muscles cramping or twitching involuntarily. Over time, muscles that aren't receiving proper nerve signals can actually begin to waste away (a process called atrophy), further compounding the weakness.
Autonomic nerves work quietly in the background, controlling all those bodily functions you never think about—your heartbeat, blood pressure, digestion, sweating, and bladder control. When these nerves are affected, your body's internal regulation can go haywire. You might feel dizzy when you stand up quickly because your blood pressure doesn't adjust properly. Your digestion might slow down, leaving you feeling uncomfortably full after eating very little. You might sweat excessively or hardly at all. Some people experience bladder control issues or sexual dysfunction. Because autonomic nerves control such vital functions, damage here can have particularly serious implications for your overall health.
Common Symptoms of Neuropathy
The symptoms you experience with neuropathy depend largely on which nerves are affected, but certain warning signs appear again and again. Recognizing these symptoms is the first step toward getting help.
Numbness is often one of the earliest signs—that peculiar sensation of your feet or hands feeling "asleep" or "dead," even when they're not. Many people describe it as feeling like they're wearing thick gloves or socks when they're actually barefoot or bare-handed. This typically starts in the toes or fingertips and can gradually spread.
Tingling, often called "pins and needles," creates that prickly, buzzing sensation that can range from mildly annoying to genuinely distressing. Some people describe it as feeling like insects crawling under their skin.
Burning pain is one of the most challenging symptoms to live with—a persistent, searing sensation that can feel like your feet or hands are on fire. This type of pain often intensifies at night, disrupting sleep and making rest nearly impossible.
Sharp, stabbing pain strikes suddenly and intensely, like being hit with an electric shock or jabbed with a needle. These pains can be brief but excruciating, appearing without warning.
Extreme sensitivity to touch, medically known as allodynia, is a particularly frustrating symptom. Something as gentle as bedsheets brushing against your feet or clothing touching your skin can cause significant pain. This can make sleeping and dressing feel like navigating a minefield.
Muscle weakness might first appear as clumsiness—dropping things more often, struggling with buttons, or finding it harder to open jars. As it progresses, weakness can affect your ability to walk normally or maintain your balance.
Coordination and balance problems make you feel unsteady on your feet, especially in low light or on uneven surfaces. This significantly increases your risk of falls and injuries.
Beyond these primary symptoms, you might notice muscle cramps or involuntary twitching, foot problems that develop because you can't feel minor injuries, digestive issues like feeling full too quickly or dealing with constipation, and temperature regulation problems where you can't sweat properly or feel overheated easily.
These symptoms aren't just uncomfortable—they can fundamentally change how you move through your day, affecting everything from your morning routine to your ability to exercise or work. The good news is that understanding these symptoms is the first step toward finding effective relief and regaining control of your life.
The Many Faces of Neuropathy: Types and Classifications
When we explore what is neuropathy more deeply, we find it's not just one condition—it's actually a family of over 100 different nerve disorders, each with its own characteristics and challenges. Think of it like an umbrella term that covers many related conditions. To make sense of this complexity and provide the right treatment, doctors classify neuropathy in different ways, primarily based on which type of nerve fibers are damaged and how many nerves are affected.
Types Based on Nerve Function
Our nerves are specialized workers, each with a specific job to do. When neuropathy strikes, it can target specific types of nerves, leading to very different experiences for different people.
Sensory neuropathy affects the nerves that act as your body's information gatherers—the ones that tell your brain about touch, temperature, pain, and vibration. When these nerves are damaged, the world can feel very different. You might experience numbness that makes your hands or feet feel like they belong to someone else, or tingling that feels like constant pins and needles. Sometimes, damaged sensory nerves send false alarm signals, creating burning sensations or sharp, stabbing pains when there's no actual injury. Perhaps most concerning is when these nerves stop sending signals altogether—you might not feel a cut on your foot, or notice that you've grabbed something dangerously hot until it's too late.
Motor neuropathy targets the nerves that control your muscles—your body's command center for movement. When these communication lines break down, your muscles don't get the messages they need. This can lead to weakness that makes once-simple tasks feel impossible, like struggling to open a jar or finding your legs won't quite cooperate when climbing stairs. You might also experience muscle cramps that strike without warning, or notice your muscles starting to shrink and waste away from lack of proper nerve signals. Some people develop a condition called foot drop, where they can't lift the front part of their foot properly when walking.
Autonomic neuropathy is perhaps the most unsettling type because it affects nerves you never think about—the ones running your body's autopilot systems. These nerves regulate your heart rate, blood pressure, digestion, sweating, and bladder function without any conscious effort on your part. When autonomic nerves are damaged, your body's internal thermostat and control systems can go haywire. You might feel dizzy when you stand up as your blood pressure drops suddenly, or find yourself sweating profusely in cool rooms while barely perspiring during exercise. Digestive issues are common too—feeling uncomfortably full after just a few bites, or dealing with unpredictable bowel habits. Because these nerves control vital functions, autonomic neuropathy requires careful medical attention.
Combination neuropathy is exactly what it sounds like—damage to multiple types of nerve fibers at once. Many people with neuropathy experience a mix of sensory and motor symptoms, dealing with both pain and weakness simultaneously. This broader pattern of nerve damage can make daily life particularly challenging, as you're managing several different types of symptoms at the same time.
Types Based on Nerves Affected
Another way to understand what is neuropathy is by looking at how many nerves are damaged and where they're located in your body.
Mononeuropathy means a single nerve has been damaged, usually from a specific injury, compression, or entrapment. The most famous example is probably Carpal Tunnel Syndrome, where the median nerve gets squeezed as it passes through the narrow tunnel in your wrist. If you've ever woken up with numb, tingling hands or felt shooting pains up your forearm while typing, you've experienced what median nerve compression feels like. Ulnar neuropathy is similar but affects the ulnar nerve—you might know this as hitting your "funny bone," though chronic ulnar nerve damage is anything but funny. These compression neuropathies are often treatable, especially when caught early.
Mononeuritis multiplex is a less common and somewhat puzzling pattern where two or more separate nerves in different parts of your body are damaged. Unlike the symmetrical pattern we see in other forms, this creates patchy, asymmetrical symptoms—maybe one hand and the opposite foot, for example. This pattern often points to specific underlying conditions that need investigation.
Polyneuropathy is by far the most common form of neuropathy, affecting multiple nerves throughout your body simultaneously. What makes polyneuropathy distinctive is its typical pattern of starting in the longest nerves first—which means your toes and feet usually feel symptoms before anywhere else. As the condition progresses, symptoms gradually move upward, eventually affecting your hands in a pattern doctors call "stocking-glove distribution." Imagine slowly pulling on stockings and gloves—that's how the numbness and pain typically spread. Diabetic neuropathy is the most well-known type of polyneuropathy, but many conditions can cause this widespread nerve damage pattern.
Understanding these classifications helps both you and your healthcare provider identify what type of neuropathy you're dealing with, which in turn guides treatment decisions and helps predict how the condition might progress. Whether you're experiencing the focused symptoms of a single compressed nerve or the widespread effects of polyneuropathy, knowing the specific pattern of your nerve damage is the first step toward finding relief.
Uncovering the Roots: Causes and Risk Factors of Neuropathy
When we explore what is neuropathy more deeply, we inevitably arrive at a fundamental question: what causes it? Sometimes, even after thorough medical testing, doctors can't pinpoint a specific cause. When this happens, it's called idiopathic neuropathy—essentially, nerve damage of unknown origin. But here's the encouraging part: in most cases, there is an identifiable cause. These causes generally fall into two broad categories: acquired neuropathy (conditions or exposures that develop during your lifetime) and hereditary neuropathy (genetic conditions passed down through families).
The truth is, neuropathy can stem from dozens of different sources. It might be a complication of a chronic disease you're managing, a side effect of medication, a nutritional deficiency, or even exposure to certain toxins. Understanding these potential triggers is crucial because identifying the root cause opens the door to targeted treatment—and often, the possibility of preventing further nerve damage.
For a comprehensive overview of the many factors that can lead to nerve damage, the Peripheral Neuropathy Fact Sheet from NIH is an excellent, trusted resource.
The Critical Role of Diabetes in Neuropathy
If we're talking about what is neuropathy and its causes, we absolutely must discuss diabetes. It's not just a cause—it's the most common cause of peripheral neuropathy in the United States and around the world. Diabetic neuropathy is a serious complication that affects millions of lives. The statistics are sobering: more than half of all people living with diabetes will eventually develop some form of neuropathy. That's over 50%. Currently, an estimated nine million Americans with diabetes are experiencing neuropathy symptoms right now.
So what's the connection? The primary villain is prolonged high blood sugar, also called hyperglycemia. When blood sugar levels remain liftd over time, they damage the tiny blood vessels that deliver oxygen and essential nutrients to your nerves. Without adequate blood flow, nerves begin to deteriorate—they're essentially being starved. But that's not the only mechanism at work. High blood sugar also accelerates a damaging chemical process called glycation. During glycation, excess sugar molecules attach themselves to proteins and fats in your body, forming harmful compounds called advanced glycation end products, or AGEs. These AGEs accumulate in nerve tissues and blood vessel walls, triggering inflammation and oxidative stress that further contribute to nerve damage. Scientific research on diabetic complications has extensively documented how these processes lead to the nerve damage we see in diabetic neuropathy.
The symptoms of diabetic neuropathy typically follow a predictable pattern. Most commonly, it affects the longest nerves first—those reaching your toes and feet. You might notice numbness, tingling, or burning sensations starting in your toes, gradually moving upward in a "stocking-glove" distribution that affects both sides of your body symmetrically. As it progresses, diabetic neuropathy can also affect motor nerves (causing weakness) and autonomic nerves (leading to digestive problems, blood pressure issues, and sexual dysfunction).
Here's the hopeful part: blood sugar control is incredibly powerful. Maintaining healthy blood sugar levels through diet, exercise, medication, and regular monitoring is the single most effective way to prevent diabetic neuropathy from developing in the first place—or to slow its progression if you already have it. This makes diligent diabetes management not just important, but absolutely critical.
What are the other underlying causes of neuropathy?
While diabetes takes center stage, it's far from the only cause of nerve damage. The peripheral nervous system can be affected by a surprisingly wide range of factors:
Physical injury or trauma can directly damage nerves through accidents, falls, sports injuries, or even something as simple as prolonged pressure on a nerve. Car accidents, for instance, can cause severe nerve trauma. Repetitive motions—like typing for hours or using vibrating tools—can lead to compression neuropathies like Carpal Tunnel Syndrome, where the median nerve in your wrist gets squeezed. Even sitting in an awkward position for too long can temporarily compress nerves.
Vitamin deficiencies are more common than many people realize, and they can wreak havoc on nerve health. Your nerves need specific nutrients to function properly. Deficiencies in B vitamins (especially B1, B6, and B12), vitamin E, and copper can severely impair nerve function. Vitamin B12, for example, is essential for maintaining the protective myelin sheath around nerve fibers. Vegetarians and vegans, older adults, and people with certain digestive conditions are at higher risk for B12 deficiency.
Autoimmune diseases occur when your body's immune system gets confused and attacks its own tissues—including nerves. Conditions like Lupus, Rheumatoid Arthritis, and Sjögren's syndrome can all cause neuropathy. Guillain-Barré syndrome is a particularly dramatic example where the immune system rapidly attacks the myelin sheath covering nerves, sometimes following an infection. Chronic Inflammatory Demyelinating Polyneuropathy (CIDP) is similar but develops more slowly. Vasculitis, which causes inflammation of blood vessels, can reduce blood flow to nerves, damaging them indirectly.
Infections can damage nerves either directly or by triggering immune responses. Shingles, caused by the reactivation of the chickenpox virus, is notorious for causing postherpetic neuralgia—persistent nerve pain that can last for months or years. HIV/AIDS can cause various forms of neuropathy. Lyme disease, transmitted by tick bites, can lead to neurological symptoms including neuropathy. Other infections like Hepatitis B and C, Leprosy (still a significant cause in developing countries), and Diphtheria can also affect nerves.
Kidney or liver disease can lead to a buildup of toxins in your bloodstream when these vital filtering organs aren't working properly. These accumulated toxins can poison nerve cells and create metabolic imbalances that impair nerve function.
Toxins from various sources can be directly harmful to nerves. Exposure to heavy metals like lead, mercury, and arsenic can cause significant nerve damage. Certain industrial chemicals and environmental toxins are also culprits. Veterans exposed to Agent Orange have higher rates of peripheral neuropathy, for instance.
Certain medications, while necessary for treating other conditions, can unfortunately damage nerves as a side effect. Chemotherapy drugs are perhaps the most well-known, with chemotherapy-induced peripheral neuropathy (CIPN) affecting many cancer patients and survivors. Some commonly prescribed antibiotics, particularly fluoroquinolones, have also been linked to peripheral neuropathy.
Alcohol abuse is a significant but preventable cause. Chronic, excessive alcohol consumption leads to alcoholic neuropathy through both the direct toxic effects of alcohol on nerve tissue and the nutritional deficiencies (especially B vitamins) that often accompany alcohol use disorder.
Hereditary disorders mean some people are born with a genetic predisposition to neuropathy. Charcot-Marie-Tooth disease is the most common inherited neurological disorder, causing progressive weakness and sensory loss, typically starting in the feet and lower legs.
Tumors, whether cancerous or benign, can cause neuropathy by directly pressing on nerves. In some cases, cancerous tumors can trigger paraneoplastic syndromes, where the immune system's reaction to cancer ends up attacking the nervous system.
Other metabolic conditions like hypothyroidism (an underactive thyroid gland) can also contribute to nerve damage by disrupting the body's normal metabolic processes.
The sheer variety of potential causes highlights something important: if you're experiencing symptoms of neuropathy, a thorough medical evaluation is essential. Finding the underlying cause isn't just about satisfying curiosity—it's the crucial first step toward effective treatment and preventing further nerve damage.
What is Neuropathy Diagnosis and Treatment?
When you're struggling with what is neuropathy and its often-challenging symptoms, understanding how doctors identify and treat this condition becomes crucial. The good news is that while neuropathy can be complex, modern medicine offers a range of diagnostic tools and treatment options aimed at pinpointing the cause, managing symptoms, and helping you reclaim your quality of life.
How is Neuropathy Diagnosed?
Diagnosing neuropathy is a bit like solving a medical mystery. Your doctor becomes a detective, piecing together clues from your symptoms, medical history, and a series of specialized tests. Because neuropathy has so many potential causes—from diabetes to vitamin deficiencies to autoimmune conditions—a thorough evaluation is essential.
Your medical history forms the foundation of diagnosis. Your doctor will want to know everything: When did your symptoms start? What do they feel like—burning, tingling, numbness? Do certain activities make them better or worse? They'll also ask about your overall health, any chronic conditions you have (especially diabetes), medications you're taking, your family's medical history, your diet, and lifestyle habits like alcohol use or workplace exposures to chemicals.
Next comes the physical and neurological examination. Your doctor will assess your reflexes by tapping your knees and ankles with that little rubber hammer. They'll test your muscle strength by having you push against their hands. They'll check your balance and coordination, and evaluate your ability to feel different sensations—a light touch with cotton, temperature with warm and cool objects, vibration with a tuning fork, and pinprick sensation. These simple tests reveal which nerves might be affected and help map out the pattern of damage.
Blood tests are incredibly valuable for uncovering underlying causes. A simple blood draw can check for diabetes, vitamin deficiencies (especially B12, B6, and E), signs of autoimmune diseases, kidney and liver function, thyroid problems, infections like HIV or Lyme disease, and even exposure to heavy metals or toxins.
Nerve function tests provide detailed information about how well your nerves are working. An electromyography (EMG) involves inserting a thin needle electrode into your muscles to measure their electrical activity. Yes, it sounds uncomfortable, but it's usually well-tolerated and provides crucial information about whether weakness stems from nerve damage or muscle disease. A nerve conduction study (NCS) typically accompanies the EMG. Small electrodes are placed on your skin, and mild electrical pulses are sent through your nerves to measure how quickly and strongly the signals travel. Slower speeds suggest damage to the protective myelin coating, while weaker signals indicate damage to the nerve fiber itself.
In some cases, your doctor might recommend a nerve biopsy, where a small piece of nerve tissue (usually from the lower leg) is removed and examined under a microscope. This can reveal the specific type of nerve damage and sometimes identify the cause. A skin biopsy is a less invasive option that examines small nerve fibers in the skin—particularly useful for diagnosing small fiber neuropathies that standard nerve tests might miss.
Imaging tests like MRI or CT scans help visualize the nerves and surrounding structures, identifying issues like nerve compression from a herniated disc, tumors pressing on nerves, or other structural problems.
Early and accurate diagnosis matters tremendously. As highlighted in "Peripheral Neuropathy: A Practical Approach to Diagnosis and Symptom Management", identifying the cause allows for targeted treatment that can often halt progression and sometimes even reverse damage.
Available Treatment Options for Managing Symptoms
Treating neuropathy requires a personalized, multi-pronged approach. The strategy always starts with addressing the underlying cause when possible, while simultaneously managing symptoms to help you feel better and function better in daily life.
Treating the root cause is the most effective long-term strategy. If you have diabetic neuropathy, strict blood sugar control through diet, exercise, and medication is paramount—it can prevent further damage and sometimes allow nerves to heal. Vitamin deficiencies are corrected with appropriate supplements. Autoimmune conditions might be treated with immunosuppressants or other specialized therapies. If a medication is causing your neuropathy, your doctor may adjust the dose or switch to an alternative. For nerve compression issues like carpal tunnel syndrome, physical therapy, bracing, or surgery can relieve the pressure.
Managing neuropathic pain often requires specialized medications because nerve pain doesn't respond well to standard pain relievers. Anticonvulsants like gabapentin and pregabalin have become go-to options for many people with neuropathic pain. Originally developed to treat seizures, these medications calm overactive nerves and can significantly reduce burning, shooting, and stabbing sensations. Antidepressants—particularly tricyclics like amitriptyline and SNRIs like duloxetine—also work well for nerve pain by affecting pain pathways in the brain and spinal cord, even if you're not depressed. Opioids like tramadol may be prescribed for severe pain, though doctors typically reserve these for short-term use or when other options haven't helped, given concerns about dependence and side effects.
Topical treatments offer relief right where you need it. Lidocaine patches or creams numb the affected area, while capsaicin cream (derived from chili peppers) can reduce pain signals over time, though it may cause an initial burning sensation.
For those seeking a natural, fast-acting option, our Neuropasil Nerve Pain Relief Cream was specifically formulated to address nerve pain. We've combined menthol for its cooling, soothing effect, aloe for its anti-inflammatory properties, and urea to help active ingredients penetrate deeply into the skin where they can reach damaged nerves. Many of our customers—from athletes managing training-related nerve irritation to individuals living with diabetic neuropathy, sciatica, or fibromyalgia—rely on Neuropasil as an essential part of their daily pain management routine. It provides targeted relief without the side effects of oral medications.
Physical therapy plays a vital role in maintaining function and preventing complications. A skilled physical therapist can design exercises to improve strength, flexibility, balance, and coordination—all of which may be compromised by neuropathy. They can also recommend helpful devices like braces, splints, or specialized footwear to improve mobility and prevent falls.
Transcutaneous electrical nerve stimulation (TENS) uses mild electrical currents delivered through skin electrodes to interrupt pain signals. Some people find it helpful, though the scientific evidence for its effectiveness varies. Psychological support through counseling or cognitive behavioral therapy can be invaluable—chronic pain takes a toll on mental health, and learning coping strategies can significantly improve quality of life.
Some individuals find relief through complementary approaches like acupuncture, massage therapy, or tai chi, though the scientific evidence supporting these treatments for neuropathy is still evolving.
Finally, lifestyle modifications form the foundation of good nerve health. Eating a balanced diet rich in vitamins and nutrients, exercising regularly (even gentle walking can improve circulation to nerves), avoiding smoking, and limiting alcohol consumption all support nerve function and improve the effectiveness of other treatments.
The key to successfully managing neuropathy is finding the right combination of treatments for your specific situation. What works beautifully for one person might not work as well for another, so patience and open communication with your healthcare team are essential. With the right approach, most people can find significant relief and get back to enjoying the activities they love.
Living With, Preventing, and Differentiating Neuropathy
Living with what is neuropathy means adapting to a new reality—one that often requires thoughtful lifestyle adjustments and proactive health management. But here's the encouraging news: many forms of neuropathy can be prevented, and even if you're already experiencing symptoms, there are concrete steps you can take to slow its progression and protect your nerve health.
Can Neuropathy Be Prevented?
While we can't prevent inherited forms of neuropathy, many acquired cases are within our control. Think of nerve health like maintaining a car—regular care and attention can prevent major breakdowns down the road.
Managing underlying medical conditions is your first line of defense. If you have diabetes, keeping your blood sugar levels in a healthy range isn't just about managing diabetes—it's about protecting your nerves from damage. The same goes for other chronic conditions like kidney disease, liver disease, or thyroid problems. When these conditions are well-controlled, your nerves have a much better chance of staying healthy.
Your diet plays a bigger role than you might think. Eating a balanced diet rich in fruits, vegetables, whole grains, and lean protein provides your nerves with the nutrients they need to function properly. Pay special attention to getting enough B vitamins (especially B1, B6, and B12), vitamin E, and copper. If you follow a vegetarian or vegan diet, talk with your doctor about B12 supplementation—this vitamin is crucial for nerve health and isn't readily available in plant-based foods.
Regular exercise is like a tonic for your nerves. When you move your body—even with gentle activities like walking, swimming, or cycling—you improve blood circulation, which delivers oxygen and nutrients to your nerve cells. Aim for 30 minutes to an hour of moderate exercise at least three times a week. Just check with your healthcare provider before starting any new exercise routine.
Protecting yourself from toxins means being mindful of your environment. Minimize exposure to industrial chemicals, heavy metals like lead and mercury, and certain pesticides. If your work involves these substances, make sure you're using proper protective equipment.
Here's a tough one, but it's important: limiting alcohol consumption. Excessive drinking doesn't just affect your liver—it directly damages your nerves. If you're struggling with alcohol use, reaching out for support can protect both your overall health and your nervous system.
For those already at risk or experiencing early symptoms, meticulous foot care becomes essential. Check your feet daily for any cuts, blisters, or sores that you might not feel due to reduced sensation. Wear comfortable, well-fitting, closed-toe shoes that protect your feet from injury. Even a small cut can turn into a serious problem if left untreated, especially if you have diabetes.
Don't forget about preventive healthcare measures like staying current with vaccinations. The shingles vaccine, for instance, can prevent an infection that often leads to prolonged nerve pain.
Potential Complications and Distinctions
When neuropathy isn't properly managed, it can lead to complications that significantly impact your daily life and overall health. Understanding these risks—and how neuropathy differs from related conditions—helps you stay vigilant and seek appropriate care.
Foot ulcers and infections are among the most serious complications. When you lose sensation in your feet, you might not notice a small cut, blister, or area of pressure. These seemingly minor issues can quickly develop into infected ulcers. In severe cases, particularly for people with diabetes, these infections can spread, potentially leading to gangrene and even amputation. This is why daily foot inspections and proper footwear are so critical.
Falls and injuries become more likely when neuropathy affects your balance and muscle strength. Reduced sensation in your feet, combined with muscle weakness, can make you unsteady—especially in dim lighting or on uneven surfaces. A fall can result in fractures or other injuries that complicate your condition further. Simple home modifications like removing tripping hazards, installing handrails, and ensuring good lighting can make a real difference.
Chronic pain from neuropathy can become a relentless companion, disrupting your sleep, triggering anxiety or depression, and limiting your ability to work, socialize, or enjoy activities you once loved. This persistent discomfort doesn't just affect your body—it takes a toll on your emotional well-being and overall quality of life.
When autonomic nerves are significantly damaged, complications can become life-threatening. These might include dangerous heart rhythm abnormalities, severe fluctuations in blood pressure, or profound digestive issues that prevent proper nutrient absorption.
It's also helpful to understand how what is neuropathy differs from other nerve-related conditions you might hear about:
Neuropathy refers to damage or disease of the peripheral nerves themselves, affecting how they function throughout your body. It typically causes numbness, tingling, burning pain, and weakness, often in a symmetrical pattern starting in the hands and feet.
Neuralgia, on the other hand, describes intense, sharp pain along a specific nerve pathway—think of it as nerve pain rather than nerve damage. Trigeminal neuralgia, for example, causes sudden, severe facial pain along the trigeminal nerve. While neuralgia can result from nerve damage, it can also occur without underlying neuropathy.
Radiculopathy happens when a nerve root near the spinal cord becomes compressed or irritated—often by a herniated disc or bone spur. This causes pain, numbness, or weakness that radiates along the nerve's path. Sciatica is a common example, where compression of nerve roots in the lower back sends pain down the leg. Unlike widespread neuropathy, radiculopathy typically affects one side of the body and stems from a specific structural problem near the spine.
Understanding these distinctions helps ensure you receive the right diagnosis and treatment approach. If you're experiencing nerve-related symptoms, don't hesitate to discuss them with your healthcare provider—early intervention can make all the difference in managing your condition and maintaining your quality of life.
Understanding Neuropathy: What It Is and How It Feels
Our peripheral nervous system is a vast and intricate communication network, acting as the bridge between our central nervous system (brain and spinal cord) and the rest of our body. It's responsible for transmitting a constant stream of information, enabling us to move, feel, and even regulate our internal organs without conscious thought. When we talk about what is neuropathy, we're referring to damage or disease within this crucial system.
Nerve damage disrupts this delicate communication in profound ways. Signals that should be sent might not make it through, leading to numbness or weakness. Conversely, signals might be sent when they shouldn't be, resulting in persistent pain or tingling. Sometimes, the messages themselves get garbled, causing sensations that don't match reality, like extreme sensitivity to a light touch. Neuropathy can manifest suddenly with rapid progression (acute neuropathy) or develop subtly over months or years (chronic neuropathy). Depending on the cause and extent of the damage, it can sometimes be reversible, but in many cases, especially if left untreated, it can lead to permanent changes.
What is peripheral neuropathy and how does it affect the body?
Peripheral neuropathy fundamentally alters how our body interacts with the world and itself. Our nerves are specialized to perform distinct roles:
- Sensory Nerves: These are our body's alert system, relaying information about touch, pain, temperature, and vibration back to the brain. When damaged, they can cause a range of distressing symptoms. We might experience a loss of feeling, making it hard to discern hot from cold, or a dull ache from a sharp cut. Ironically, these damaged nerves can also generate intense pain signals, resulting in burning, tingling, or electric shock-like sensations even without an external stimulus. This loss of protective sensation, particularly in the feet, can lead to unnoticed injuries and infections.
- Motor Nerves: These are the command lines from our brain to our muscles, controlling every voluntary movement. Damage here can lead to muscle weakness, making simple tasks like walking, gripping objects, or climbing stairs challenging. It can also cause muscle cramps, spasms, and even muscle wasting (atrophy).
- Autonomic Nerves: These silent workhorses control involuntary bodily functions that we don't consciously think about, such as heart rate, blood pressure, digestion, sweating, and bladder function. When autonomic nerves are affected, the body's internal regulation can go awry. Symptoms might include dizziness upon standing (due to sudden blood pressure drops), digestive problems (like feeling full quickly or irregular bowel movements), abnormal sweating (either excessive or too little), and issues with bladder control or sexual function. Autonomic neuropathy can be particularly serious due to its impact on vital systems.
Peripheral neuropathy can disconnect us from our own bodies and environment, making daily life a constant challenge.
Common Symptoms of Neuropathy
The symptoms we experience with neuropathy are as varied as its causes, often depending on which nerves are damaged. However, there are several common indicators that can help us recognize when something is amiss:
- Numbness: A pervasive loss of sensation, often described as a "dead" feeling, typically starting in the hands or feet. Many describe it as feeling like they're wearing invisible gloves or socks.
- Tingling (Pins and Needles): A prickly, buzzing, or "creepy-crawly" sensation that can be mildly irritating or profoundly uncomfortable.
- Burning Pain: A persistent, intense, and often deep-seated heat sensation that can range from a mild warmth to an agonizing blaze, frequently worsening at night.
- Sharp, Stabbing, or Jabbing Pain: Sudden, intense, and often fleeting pains that can feel like electric shocks or sudden, piercing sensations.
- Extreme Sensitivity to Touch (Allodynia): This is a peculiar symptom where even the lightest touch—like that of bedsheets, clothing, or a gentle breeze—can elicit excruciating pain.
- Muscle Weakness: Difficulty moving a limb, lifting objects, or maintaining grip strength. This can manifest as clumsiness or, in severe cases, partial paralysis, such as foot drop (difficulty lifting the front part of the foot).
- Lack of Coordination and Balance Issues: Feeling unsteady on your feet, especially when walking in the dark or on uneven surfaces, significantly increasing the risk of falls.
- Muscle Cramps and Fasciculations: Involuntary twitching of muscles or painful, sustained muscle spasms.
- Foot Problems: Due to diminished sensation, cuts, blisters, or sores on the feet may go unnoticed, leading to severe infections and potential complications if not treated promptly.
- Digestive Issues: Feeling full quickly after eating, nausea, vomiting, constipation, or diarrhea, often due to autonomic nerve involvement affecting the gastrointestinal tract.
- Heat Intolerance and Sweating Abnormalities: Difficulty regulating body temperature, either sweating excessively or not enough.
These symptoms can vary in intensity and frequency, but their presence often signals nerve damage that warrants medical attention.
The Many Faces of Neuropathy: Types and Classifications
Understanding what is neuropathy also means recognizing its diverse forms. With over 100 different types identified, classifying neuropathy helps us pinpoint the specific nerves affected and, often, the underlying cause. These classifications are typically based on the type of nerve fibers involved or the pattern of nerve damage.
Types Based on Nerve Function
Nerves are specialized for different tasks, and neuropathy can target these specific functions:
- Sensory Neuropathy: This type affects the nerves responsible for relaying sensory information to the brain. This includes touch, temperature, pain, and vibration. Individuals often experience numbness, tingling, burning, or sharp pains. A critical consequence can be the inability to feel extreme temperatures or injuries, leading to increased risk of burns, frostbite, or unnoticed wounds.
- Motor Neuropathy: Here, the nerves controlling voluntary muscle movements are damaged. Symptoms typically include muscle weakness, muscle cramps, and loss of muscle mass (atrophy). This can make daily activities like walking, writing, or lifting objects extremely difficult.
- Autonomic Neuropathy: This affects the nerves that regulate involuntary bodily functions. Symptoms are diverse and can include issues with blood pressure (e.g., dizziness when standing), heart rate, digestion (e.g., early fullness, constipation), bladder control, sexual function, and sweating. Autonomic neuropathy can lead to serious complications affecting vital bodily systems.
- Combination Neuropathy: Many individuals experience damage to more than one type of nerve fiber, often a mix of sensory and motor nerves. This results in a broader spectrum of symptoms affecting both sensation and movement.
Types Based on Nerves Affected
Neuropathy can also be classified by the number of nerves damaged and their distribution:
- Mononeuropathy (one nerve): This type affects a single nerve. It often occurs due to trauma, compression, or entrapment of a specific nerve. A common example is Carpal Tunnel Syndrome, where the median nerve in the wrist is compressed, leading to numbness, tingling, and pain in the hand. Another is Ulnar Neuropathy, which affects the ulnar nerve in the arm.
- Mononeuritis Multiplex: This is a less common pattern where two or more distinct nerves in different, separate areas of the body are damaged. Symptoms tend to be patchy and asymmetrical.
- Polyneuropathy (multiple nerves): This is the most prevalent form of neuropathy, involving damage to multiple peripheral nerves throughout the body. Symptoms typically appear symmetrically, often starting in the longest nerves first. This means the feet and hands are usually affected before other areas, a pattern known as "length-dependent" neuropathy. Diabetic neuropathy is a classic example of polyneuropathy.
Uncovering the Roots: Causes and Risk Factors of Neuropathy
Delving into what is neuropathy inevitably leads us to its complex origins. Sometimes, despite extensive medical evaluation, the cause remains elusive, leading to a diagnosis of idiopathic neuropathy. However, in many cases, neuropathy is a symptom or complication of an underlying health condition, an exposure to toxins, or a genetic predisposition. We broadly categorize these as acquired neuropathy (developing during a person's lifetime) and hereditary neuropathy (inherited genetically).
The Peripheral Neuropathy Fact Sheet from NIH offers valuable insights into the numerous factors at play.
The Critical Role of Diabetes in Neuropathy
Without a doubt, diabetes is the leading cause of neuropathy in the United States and globally. Diabetic neuropathy is a severe and common complication that impacts the lives of millions. Statistics reveal that more than half of all individuals living with diabetes will eventually develop some form of neuropathy. Furthermore, an estimated nine million people with diabetes actively experience symptoms of diabetic neuropathy, highlighting the widespread impact of this condition.
The primary culprit behind diabetic neuropathy is prolonged and uncontrolled high blood sugar levels, or hyperglycemia. Over time, this excess glucose in the bloodstream damages the tiny blood vessels that supply oxygen and nutrients to the nerves. This deprivation essentially starves the nerves, leading to their deterioration. Additionally, high blood sugar accelerates a damaging process called glycation. During glycation, sugar molecules irreversibly attach to proteins and fats, forming compounds known as advanced glycation end products (AGEs). These AGEs accumulate in nerve tissues and blood vessel walls, causing inflammation and oxidative stress, which further contribute to nerve damage. Research extensively documents the role of advanced glycation end products in diabetic neuropathy and other diabetic complications.
Diabetic neuropathy most commonly presents as a length-dependent polyneuropathy, meaning symptoms typically begin in the toes and feet, gradually progressing upwards, affecting both sides of the body symmetrically. It can also affect motor and autonomic nerves, leading to muscle weakness and issues with digestion, blood pressure, and sexual function. The good news is that rigorous blood sugar control is the most effective strategy to prevent the onset and slow the progression of diabetic neuropathy. This emphasizes the critical importance of diligent diabetes management.
What are the other underlying causes of neuropathy?
While diabetes is a significant player, many other factors contribute to nerve damage:
- Physical Injury or Trauma: Direct physical impact, accidents, sports injuries, or even prolonged pressure can sever, crush, or stretch nerves. Repetitive motions, such as those involved in certain occupations, can lead to nerve compression syndromes like Carpal Tunnel Syndrome, causing localized neuropathy.
- Vitamin Deficiencies: Nerves are hungry for specific nutrients. Deficiencies in crucial B vitamins (B1, B6, B12), vitamin E, and copper can severely compromise nerve health and function. For instance, vitamin B12 is essential for maintaining the myelin sheath that protects nerve fibers.
-
Autoimmune Diseases: In these conditions, the body's immune system, which normally protects us, mistakenly attacks its own healthy tissues, including nerves. Examples include:
- Lupus
- Rheumatoid Arthritis
- Sjögren's syndrome
- Guillain-Barré syndrome (a rapid-onset condition where the immune system attacks myelin)
- Chronic Inflammatory Demyelinating Polyneuropathy (CIDP)
- Vasculitis (inflammation of blood vessels, restricting blood flow to nerves)
-
Infections: Various infectious agents can directly damage nerves or trigger an immune response that harms them:
- Shingles (postherpetic neuralgia is a common complication)
- HIV/AIDS (can cause several forms of neuropathy)
- Lyme disease (can lead to a range of neuropathic symptoms)
- Hepatitis B and C
- Leprosy (a common cause of neuropathy in developing nations)
- Diphtheria
- Kidney or Liver Disease: When these organs don't function properly, toxins can accumulate in the bloodstream, poisoning nerve cells. They can also disrupt metabolic balances essential for nerve health.
-
Toxins: Exposure to certain substances can be directly neurotoxic:
- Heavy metals (e.g., lead, mercury, arsenic)
- Industrial chemicals
- Certain environmental agents (e.g., Agent Orange, linked to neuropathy in veterans)
- Certain Medications: A number of pharmaceutical drugs can have neuropathy as a side effect. Chemotherapy drugs are a well-known cause of chemotherapy-induced peripheral neuropathy (CIPN), a often disabling side effect of cancer treatment. Some commonly prescribed antibiotics, such as fluoroquinolones, have also been associated with peripheral neuropathy.
- Alcohol Abuse: Chronic and excessive alcohol consumption can lead to alcoholic neuropathy, primarily due to the direct toxic effects of alcohol on nerve tissue and the associated nutritional deficiencies (like B vitamin depletion) often seen in individuals with alcohol use disorder.
- Hereditary Disorders: Some neuropathies are genetic, passed down through families. Charcot-Marie-Tooth disease is the most common inherited neurological disorder, causing progressive weakness and sensory loss, particularly in the lower legs and hands.
- Tumors: Both cancerous and non-cancerous growths can cause neuropathy. They might directly press on nerves, or in some cases, cancerous tumors can trigger a paraneoplastic syndrome, where the immune system attacks the nervous system in response to the cancer.
- Other Metabolic Conditions: Conditions like hypothyroidism (an underactive thyroid) can also contribute to nerve damage.
The sheer number of potential causes underscores why a thorough medical investigation is crucial when experiencing symptoms of neuropathy. Identifying the root cause is the first step towards effective treatment and relief.
What is Neuropathy Diagnosis and Treatment?
When faced with the question of what is neuropathy, understanding how it's diagnosed and treated becomes paramount. Our primary goals are to identify the underlying cause, manage the often-debilitating symptoms, and ultimately improve an individual's quality of life.
How is Neuropathy Diagnosed?
Diagnosing neuropathy is a detective process that combines a detailed understanding of your symptoms with a range of medical tests. Since its causes are so varied, a thorough evaluation is essential.
- Medical History: This is often the starting point. Your doctor will ask comprehensive questions about your symptoms (onset, progression, triggers, characteristics of pain or numbness), your general health, any existing medical conditions (like diabetes or autoimmune disorders), current and past medications (including chemotherapy), family history of neurological conditions, dietary habits, and lifestyle factors (such as alcohol consumption or exposure to toxins).
- Physical and Neurological Exam: This hands-on assessment allows your doctor to evaluate your reflexes, muscle strength, muscle tone, balance, coordination, and sensory perception (your ability to feel light touch, temperature, pinprick, and vibration). The findings help to pinpoint which nerves are affected and the pattern of nerve damage.
-
Blood Tests: These are invaluable for uncovering many underlying causes. They can screen for:
- Diabetes (checking blood glucose and A1c levels)
- Vitamin deficiencies (e.g., B12, B6, E)
- Markers for autoimmune diseases (e.g., ANA, ESR)
- Kidney and liver function tests
- Thyroid hormone levels
- Infection markers (e.g., HIV, Lyme disease)
- Evidence of heavy metal poisoning or other toxins
-
Nerve Function Tests:
- Electromyography (EMG): This test involves inserting a thin needle electrode into various muscles to measure their electrical activity, both at rest and during contraction. It helps determine if muscle weakness is due to nerve damage or a primary muscle disorder.
- Nerve Conduction Study (NCS): Often performed in conjunction with EMG, this test places surface electrodes on the skin over a nerve. A mild electrical impulse is delivered, and the speed and strength of the nerve's response are measured. Slowed conduction can indicate damage to the myelin sheath, while reduced signal amplitude suggests damage to the nerve axon itself.
- Nerve Biopsy: In certain situations, a small piece of nerve tissue (usually from the calf) is surgically removed and examined under a microscope. This can provide detailed information about the type of nerve damage (e.g., demyelination, axonal degeneration) and sometimes reveal the specific cause.
- Skin Biopsy: This less invasive procedure takes a small skin sample to assess the density of small nerve fibers. It's particularly useful for diagnosing small fiber neuropathies, which may not show up on standard EMG/NCS.
- Imaging Tests: Magnetic Resonance Imaging (MRI) or Computed Tomography (CT) scans can visualize nerves and surrounding structures, helping to identify nerve compression, tumors, herniated discs, or other structural abnormalities that might be causing neuropathy.
As Watson and Dyck emphasize in "Peripheral Neuropathy: A Practical Approach to Diagnosis and Symptom Management" (Mayo Clinic Proceedings), accurate diagnosis is the cornerstone of effective treatment. Finding the cause allows for targeted treatment, which can often halt progression and sometimes even reverse nerve damage.
Available Treatment Options for Managing Symptoms
Treating neuropathy is a multi-faceted endeavor, often requiring a combination of approaches custom to the individual. The primary focus is always on addressing the underlying cause (if identifiable) and, if not, or while the underlying condition is being managed, symptom relief becomes paramount.
-
Addressing the Underlying Cause: This is the most effective long-term strategy for many neuropathies.
- Diabetes: Strict blood glucose control is non-negotiable.
- Vitamin Deficiencies: Supplementation is prescribed to restore healthy levels.
- Autoimmune Conditions: Immunosuppressants, steroids, intravenous immunoglobulin (IVIg), or plasmapheresis may be used.
- Medication-Induced: The offending medication may be adjusted or discontinued (under medical supervision).
- Compression: Physical therapy, splinting, or surgical decompression can relieve pressure on nerves.
-
Pain Management Strategies: Neuropathic pain can be notoriously difficult to treat, but several options are available:
-
Oral Medications:
- Anticonvulsants: Gabapentin and pregabalin are commonly prescribed and effective for many types of neuropathic pain. Other options include oxcarbazepine, carbamazepine, and lamotrigine.
- Antidepressants: Tricyclic antidepressants (e.g., amitriptyline, nortriptyline) and serotonin-norepinephrine reuptake inhibitors (SNRIs like duloxetine, venlafaxine, milnacipran) can help by affecting pain pathways in the brain.
- Opioids: While effective for severe pain, strong opioids are generally used with caution due to the risk of dependence and side effects. Tramadol is a weaker opioid sometimes used for neuropathic pain.
- NSAIDs and Acetaminophen: Generally less effective for neuropathic pain compared to other types of pain.
-
Topical Treatments: Creams, gels, or patches applied directly to the skin can provide localized relief:
- Lidocaine patches: Can numb the area.
- Capsaicin cream: Derived from chili peppers, it can reduce pain signals over time, though it may cause an initial burning sensation.
-
Oral Medications:
Neuropasil Nerve Pain Relief Cream: For immediate, targeted relief from the burning, tingling, and aching of neuropathy, we've developed Neuropasil Nerve Pain Relief Cream. Our unique formula leverages natural ingredients like menthol, which provides a cooling and soothing sensation, aloe for its anti-inflammatory properties, and urea to improve the penetration of active ingredients deep into the skin. This powerful combination works to soothe damaged and inflamed nerves, offering a natural option for managing nerve pain. Many of our loyal customers, including athletes and individuals with conditions like sciatica and fibromyalgia, find it invaluable for managing their daily discomfort. You can find more info about our Nerve Pain Relief Cream on our website.
-
Supportive Therapies:
- Physical Therapy: Custom exercises can improve muscle strength, flexibility, balance, and coordination. Physical therapists can also recommend assistive devices like braces, splints, or orthopedic shoes to aid mobility and prevent falls.
- Transcutaneous Electrical Nerve Stimulation (TENS): This non-invasive therapy uses mild electrical currents delivered through electrodes placed on the skin to interrupt pain signals. While some studies suggest it can offer relief, especially for diabetic peripheral neuropathy, the overall evidence for its effectiveness in general neuropathic pain is still considered low to moderate.
- Psychological Support: Living with chronic pain can be emotionally taxing. Counseling, cognitive behavioral therapy (CBT), and support groups can help individuals develop coping strategies and manage the psychological impact of neuropathy.
- Complementary Treatments: Some individuals explore acupuncture, massage, or tai chi for pain relief, though scientific evidence for their efficacy in neuropathy varies.
Surgery: For cases of nerve compression (like carpal tunnel syndrome) or tumors pressing on nerves, surgical decompression can relieve pressure and restore nerve function. While surgical decompression has shown promise for diabetic peripheral neuropathy in specific cases, it's generally not recommended for widespread neuropathy. Most neuropathies involve scattered nerve damage and are not helped by surgery.
Lifestyle Modifications: Maintaining a healthy lifestyle, including a balanced diet, regular exercise, avoiding smoking, and limiting alcohol, plays a crucial role in supporting nerve health and enhancing the effectiveness of other treatments.
A personalized treatment plan, often involving a combination of these strategies, is key to effectively managing neuropathy symptoms and improving overall well-being.
Living With, Preventing, and Differentiating Neuropathy
Living with neuropathy is a journey that often requires significant lifestyle adjustments and proactive health management. Understanding what is neuropathy also includes knowing how to prevent it and how it differs from other conditions with similar symptoms.
Can Neuropathy Be Prevented?
While not all forms of neuropathy are preventable, especially those with genetic causes, a significant number of acquired neuropathies can be avoided or their progression slowed through diligent lifestyle choices and medical management.
-
Managing Medical Conditions: This is arguably the most impactful preventive measure.
- Diabetes: Strict control of blood sugar levels is paramount. Maintaining target glucose levels through diet, exercise, and medication can prevent or significantly delay the onset and progression of diabetic neuropathy.
- Other Chronic Diseases: Effectively managing kidney disease, liver disease, autoimmune disorders, and hypothyroidism is crucial, as their uncontrolled progression can lead to nerve damage.
-
Healthy Diet: A balanced, nutrient-rich diet supports overall nerve health. Focus on:
- Fruits, Vegetables, and Whole Grains: Provide essential vitamins, minerals, and antioxidants.
- Lean Protein: Important for nerve repair and maintenance.
- Adequate Vitamins: Ensure sufficient intake of B vitamins (B1, B6, B12), vitamin E, and copper. Deficiencies in these are well-known causes of neuropathy. If you follow a vegetarian or vegan diet, discuss B12 supplementation with your doctor.
- Regular Exercise: Physical activity improves circulation, which is vital for delivering oxygen and nutrients to nerves. Aim for 30 minutes to one hour of moderate exercise, at least three times a week, after consulting your healthcare provider. This could include walking, swimming, or cycling.
- Avoiding Toxins: Minimize exposure to industrial chemicals, heavy metals (like lead and mercury), and certain pesticides, which are known neurotoxins.
- Limiting Alcohol: Excessive and chronic alcohol consumption is a direct cause of alcoholic neuropathy and can exacerbate other forms of nerve damage. Reducing or eliminating alcohol intake is a key preventive step.
-
Foot Care: For those at risk or already experiencing early symptoms, meticulous foot care is crucial.
- Inspect your feet daily for cuts, blisters, or sores, as reduced sensation might prevent you from feeling them.
- Wear comfortable, well-fitting, closed-toe shoes to protect your feet from injury.
- Treat even minor injuries promptly to prevent infection, especially if you have diabetes.
- Safety Measures: Use appropriate safety equipment during work or sports activities to prevent injuries that could damage nerves.
By embracing these proactive strategies, we can significantly reduce the risk of developing neuropathy or slow its progression, maintaining better nerve health for longer.
Potential Complications and Distinctions
Left untreated or poorly managed, neuropathy can lead to a cascade of serious complications that drastically affect quality of life:
- Foot Ulcers and Infections: Loss of sensation, particularly in the feet, means minor cuts, blisters, or pressure points can go unnoticed. These can quickly develop into ulcers and infections, which, if severe, may lead to gangrene and necessitate amputation, especially in individuals with diabetes.
- Falls and Injuries: Muscle weakness, impaired balance, and reduced sensation increase the risk of falls, leading to fractures, sprains, and other traumatic injuries. Simple home modifications like removing tripping hazards and installing handrails can help.
- Chronic Pain: Persistent neuropathic pain can be debilitating, causing sleep disturbances, anxiety, depression, and a significant reduction in daily activities and overall well-being.
- Decreased Quality of Life: The cumulative effect of pain, functional limitations, and emotional distress can severely impact an individual's ability to work, socialize, and enjoy life.
- Autonomic Complications: If autonomic nerves are significantly damaged, complications can be life-threatening, including severe heart rhythm abnormalities, dangerous fluctuations in blood pressure, and profound digestive issues that impair nutrient absorption.
It's also important to understand how neuropathy differs from other conditions that cause nerve-related symptoms:
| Feature | Neuropathy The following is a comprehensive research report for an article on the keyword "what is neuropathy", designed to provide an exhaustive guide.
Understanding Neuropathy: What It Is and How It Feels
Our peripheral nervous system is a vast and intricate communication network, acting as the bridge between our central nervous system (brain and spinal cord) and the rest of our body. It's responsible for transmitting a constant stream of information, enabling us to move, feel, and even regulate our internal organs without conscious thought. When we talk about what is neuropathy, we're referring to damage or disease within this crucial system.
Nerve damage disrupts this delicate communication in profound ways. Signals that should be sent might not make it through, leading to numbness or weakness. Conversely, signals might be sent when they shouldn't be, resulting in persistent pain or tingling. Sometimes, the messages themselves get garbled, causing sensations that don't match reality, like extreme sensitivity to a light touch. Neuropathy can manifest suddenly with rapid progression (acute neuropathy) or develop subtly over months or years (chronic neuropathy). Depending on the cause and extent of the damage, it can sometimes be reversible, but in many cases, especially if left untreated, it can lead to permanent changes.
What is peripheral neuropathy and how does it affect the body?
Peripheral neuropathy fundamentally alters how our body interacts with the world and itself. Our nerves are specialized to perform distinct roles:
- Sensory Nerves: These are our body's alert system, relaying information about touch, pain, temperature, and vibration back to the brain. When damaged, they can cause a range of distressing symptoms. We might experience a loss of feeling, making it hard to discern hot from cold, or a dull ache from a sharp cut. Ironically, these damaged nerves can also generate intense pain signals, resulting in burning, tingling, or electric shock-like sensations even without an external stimulus. This loss of protective sensation, particularly in the feet, can lead to unnoticed injuries and infections.
- Motor Nerves: These are the command lines from our brain to our muscles, controlling every voluntary movement. Damage here can lead to muscle weakness, making simple tasks like walking, gripping objects, or climbing stairs challenging. It can also cause muscle cramps, spasms, and even muscle wasting (atrophy).
- Autonomic Nerves: These silent workhorses control involuntary bodily functions that we don't consciously think about, such as heart rate, blood pressure, digestion, sweating, and bladder function. When autonomic nerves are affected, the body's internal regulation can go awry. Symptoms might include dizziness upon standing (due to sudden blood pressure drops), digestive problems (like feeling full quickly or irregular bowel movements), abnormal sweating (either excessive or too little), and issues with bladder control or sexual function. Autonomic neuropathy can be particularly serious due to its impact on vital systems.
Peripheral neuropathy can disconnect us from our own bodies and environment, making daily life a constant challenge.
Common Symptoms of Neuropathy
The symptoms we experience with neuropathy are as varied as its causes, often depending on which nerves are damaged. However, there are several common indicators that can help us recognize when something is amiss:
- Numbness: A pervasive loss of sensation, often described as a "dead" feeling, typically starting in the hands or feet. Many describe it as feeling like they're wearing invisible gloves or socks.
- Tingling (Pins and Needles): A prickly, buzzing, or "creepy-crawly" sensation that can be mildly irritating or profoundly uncomfortable.
- Burning Pain: A persistent, intense, and often deep-seated heat sensation that can range from a mild warmth to an agonizing blaze, frequently worsening at night.
- Sharp, Stabbing, or Jabbing Pain: Sudden, intense, and often fleeting pains that can feel like electric shocks or sudden, piercing sensations.
- Extreme Sensitivity to Touch (Allodynia): This is a peculiar symptom where even the lightest touch—like that of bedsheets, clothing, or a gentle breeze—can elicit excruciating pain.
- Muscle Weakness: Difficulty moving a limb, lifting objects, or maintaining grip strength. This can manifest as clumsiness or, in severe cases, partial paralysis, such as foot drop (difficulty lifting the front part of the foot).
- Lack of Coordination and Balance Issues: Feeling unsteady on your feet, especially when walking in the dark or on uneven surfaces, significantly increasing the risk of falls.
- Muscle Cramps and Fasciculations: Involuntary twitching of muscles or painful, sustained muscle spasms.
- Foot Problems: Due to diminished sensation, cuts, blisters, or sores on the feet may go unnoticed, leading to severe infections and potential complications if not treated promptly.
- Digestive Issues: Feeling full quickly after eating, nausea, vomiting, constipation, or diarrhea, often due to autonomic nerve involvement affecting the gastrointestinal tract.
- Heat Intolerance and Sweating Abnormalities: Difficulty regulating body temperature, either sweating excessively or not enough.
These symptoms can vary in intensity and frequency, but their presence often signals nerve damage that warrants medical attention.
The Many Faces of Neuropathy: Types and Classifications
Understanding what is neuropathy also means recognizing its diverse forms. With over 100 different types identified, classifying neuropathy helps us pinpoint the specific nerves affected and, often, the underlying cause. These classifications are typically based on the type of nerve fibers involved or the pattern of nerve damage.
Types Based on Nerve Function
Nerves are specialized for different tasks, and neuropathy can target these specific functions:
- Sensory Neuropathy: This type affects the nerves responsible for relaying sensory information to the brain. This includes touch, temperature, pain, and vibration. Individuals often experience numbness, tingling, burning, or sharp pains. A critical consequence can be the inability to feel extreme temperatures or injuries, leading to increased risk of burns, frostbite, or unnoticed wounds.
- Motor Neuropathy: Here, the nerves controlling voluntary muscle movements are damaged. Symptoms typically include muscle weakness, muscle cramps, and loss of muscle mass (atrophy). This can make daily activities like walking, writing, or lifting objects extremely difficult.
- Autonomic Neuropathy: This affects the nerves that regulate involuntary bodily functions. Symptoms are diverse and can include issues with blood pressure (e.g., dizziness when standing), heart rate, digestion (e.g., early fullness, constipation), bladder control, sexual function, and sweating. Autonomic neuropathy can lead to serious complications affecting vital bodily systems.
- Combination Neuropathy: Many individuals experience damage to more than one type of nerve fiber, often a mix of sensory and motor nerves. This results in a broader spectrum of symptoms affecting both sensation and movement.
Types Based on Nerves Affected
Neuropathy can also be classified by the number of nerves damaged and their distribution:
- Mononeuropathy (one nerve): This type affects a single nerve. It often occurs due to trauma, compression, or entrapment of a specific nerve. A common example is Carpal Tunnel Syndrome, where the median nerve in the wrist is compressed, leading to numbness, tingling, and pain in the hand. Another is Ulnar Neuropathy, which affects the ulnar nerve in the arm.
- Mononeuritis Multiplex: This is a less common pattern where two or more distinct nerves in different, separate areas of the body are damaged. Symptoms tend to be patchy and asymmetrical.
- Polyneuropathy (multiple nerves): This is the most prevalent form of neuropathy, involving damage to multiple peripheral nerves throughout the body. Symptoms typically appear symmetrically, often starting in the longest nerves first. This means the feet and hands are usually affected before other areas, a pattern known as "length-dependent" neuropathy. Diabetic neuropathy is a classic example of polyneuropathy.
Uncovering the Roots: Causes and Risk Factors of Neuropathy
Delving into what is neuropathy inevitably leads us to its complex origins. Sometimes, despite extensive medical evaluation, the cause remains elusive, leading to a diagnosis of idiopathic neuropathy. However, in many cases, neuropathy is a symptom or complication of an underlying health condition, an exposure to toxins, or a genetic predisposition. We broadly categorize these as acquired neuropathy (developing during a person's lifetime) and hereditary neuropathy (inherited genetically).
The Peripheral Neuropathy Fact Sheet from NIH offers valuable insights into the numerous factors at play.
The Critical Role of Diabetes in Neuropathy
Without a doubt, diabetes is the leading cause of neuropathy in the United States and globally. Diabetic neuropathy is a severe and common complication that impacts the lives of millions. Statistics reveal that more than half of all individuals living with diabetes will eventually develop some form of neuropathy. Furthermore, an estimated nine million people with diabetes actively experience symptoms of diabetic neuropathy, highlighting the widespread impact of this condition.
The primary culprit behind diabetic neuropathy is prolonged and uncontrolled high blood sugar levels, or hyperglycemia. Over time, this excess glucose in the bloodstream damages the tiny blood vessels that supply oxygen and nutrients to the nerves. This deprivation essentially starves the nerves, leading to their deterioration. Additionally, high blood sugar accelerates a damaging process called glycation. During glycation, sugar molecules irreversibly attach to proteins and fats, forming compounds known as advanced glycation end products (AGEs). These AGEs accumulate in nerve tissues and blood vessel walls, causing inflammation and oxidative stress, which further contribute to nerve damage. Research extensively documents the role of advanced glycation end products in diabetic neuropathy and other diabetic complications.
Diabetic neuropathy most commonly presents as a length-dependent polyneuropathy, meaning symptoms typically begin in the toes and feet, gradually progressing upwards, affecting both sides of the body symmetrically. It can also affect motor and autonomic nerves, leading to muscle weakness and issues with digestion, blood pressure, and sexual function. The good news is that rigorous blood sugar control is the most effective strategy to prevent the onset and slow the progression of diabetic neuropathy. This emphasizes the critical importance of diligent diabetes management.
What are the other underlying causes of neuropathy?
While diabetes is a significant player, many other factors contribute to nerve damage:
- Physical Injury or Trauma: Direct physical impact, accidents, sports injuries, or even prolonged pressure can sever, crush, or stretch nerves. Repetitive motions, such as those involved in certain occupations, can lead to nerve compression syndromes like Carpal Tunnel Syndrome, causing localized neuropathy.
- Vitamin Deficiencies: Nerves are hungry for specific nutrients. Deficiencies in crucial B vitamins (B1, B6, B12), vitamin E, and copper can severely compromise nerve health and function. For instance, vitamin B12 is essential for maintaining the myelin sheath that protects nerve fibers.
-
Autoimmune Diseases: In these conditions, the body's immune system, which normally protects us, mistakenly attacks its own healthy tissues, including nerves. Examples include:
- Lupus
- Rheumatoid Arthritis
- Sjögren's syndrome
- Guillain-Barré syndrome (a rapid-onset condition where the immune system attacks myelin)
- Chronic Inflammatory Demyelinating Polyneuropathy (CIDP)
- Vasculitis (inflammation of blood vessels, restricting blood flow to nerves)
-
Infections: Various infectious agents can directly damage nerves or trigger an immune response that harms them:
- Shingles (postherpetic neuralgia is a common complication)
- HIV/AIDS (can cause several forms of neuropathy)
- Lyme disease (can lead to a range of neuropathic symptoms)
- Hepatitis B and C
- Leprosy (a common cause of neuropathy in developing nations)
- Diphtheria
- Kidney or Liver Disease: When these organs don't function properly, toxins can accumulate in the bloodstream, poisoning nerve cells. They can also disrupt metabolic balances essential for nerve health.
-
Toxins: Exposure to certain substances can be directly neurotoxic:
- Heavy metals (e.g., lead, mercury, arsenic)
- Industrial chemicals
- Certain environmental agents (e.g., Agent Orange, linked to neuropathy in veterans)
- Certain Medications: A number of pharmaceutical drugs can have neuropathy as a side effect. Chemotherapy drugs are a well-known cause of chemotherapy-induced peripheral neuropathy (CIPN), a often disabling side effect of cancer treatment. Some commonly prescribed antibiotics, such as fluoroquinolones, have also been associated with peripheral neuropathy.
- Alcohol Abuse: Chronic and excessive alcohol consumption can lead to alcoholic neuropathy, primarily due to the direct toxic effects of alcohol on nerve tissue and the associated nutritional deficiencies (like B vitamin depletion) often seen in individuals with alcohol use disorder.
- Hereditary Disorders: Some neuropathies are genetic, passed down through families. Charcot-Marie-Tooth disease is the most common inherited neurological disorder, causing progressive weakness and sensory loss, particularly in the lower legs and hands.
- Tumors: Both cancerous and non-cancerous growths can cause neuropathy. They might directly press on nerves, or in some cases, cancerous tumors can trigger a paraneoplastic syndrome, where the immune system attacks the nervous system in response to the cancer.
- Other Metabolic Conditions: Conditions like hypothyroidism (an underactive thyroid) can also contribute to nerve damage.
The sheer number of potential causes underscores why a thorough medical investigation is crucial when experiencing symptoms of neuropathy. Identifying the root cause is the first step towards effective treatment and relief.
What is Neuropathy Diagnosis and Treatment?
When faced with the question of what is neuropathy, understanding how it's diagnosed and treated becomes paramount. Our primary goals are to identify the underlying cause, manage the often-debilitating symptoms, and ultimately improve an individual's quality of life.
How is Neuropathy Diagnosed?
Diagnosing neuropathy is a detective process that combines a detailed understanding of your symptoms with a range of medical tests. Since its causes are so varied, a thorough evaluation is essential.
- Medical History: This is often the starting point. Your doctor will ask comprehensive questions about your symptoms (onset, progression, triggers, characteristics of pain or numbness), your general health, any existing medical conditions (like diabetes or autoimmune disorders), current and past medications (including chemotherapy), family history of neurological conditions, dietary habits, and lifestyle factors (such as alcohol consumption or exposure to toxins).
- Physical and Neurological Exam: This hands-on assessment allows your doctor to evaluate your reflexes, muscle strength, muscle tone, balance, coordination, and sensory perception (your ability to feel light touch, temperature, pinprick, and vibration). The findings help to pinpoint which nerves are affected and the pattern of nerve damage.
-
Blood Tests: These are invaluable for uncovering many underlying causes. They can screen for:
- Diabetes (checking blood glucose and A1c levels)
- Vitamin deficiencies (e.g., B12, B6, E)
- Markers for autoimmune diseases (e.g., ANA, ESR)
- Kidney and liver function tests
- Thyroid hormone levels
- Infection markers (e.g., HIV, Lyme disease)
- Evidence of heavy metal poisoning or other toxins
-
Nerve Function Tests:
- Electromyography (EMG): This test involves inserting a thin needle electrode into various muscles to measure their electrical activity, both at rest and during contraction. It helps determine if muscle weakness is due to nerve damage or a primary muscle disorder.
- Nerve Conduction Study (NCS): Often performed in conjunction with EMG, this test places surface electrodes on the skin over a nerve. A mild electrical impulse is delivered, and the speed and strength of the nerve's response are measured. Slowed conduction can indicate damage to the myelin sheath, while reduced signal amplitude suggests damage to the nerve axon itself.
- Nerve Biopsy: In certain situations, a small piece of nerve tissue (usually from the calf) is surgically removed and examined under a microscope. This can provide detailed information about the type of nerve damage (e.g., demyelination, axonal degeneration) and sometimes reveal the specific cause.
- Skin Biopsy: This less invasive procedure takes a small skin sample to assess the density of small nerve fibers. It's particularly useful for diagnosing small fiber neuropathies, which may not show up on standard EMG/NCS.
- Imaging Tests: Magnetic Resonance Imaging (MRI) or Computed Tomography (CT) scans can visualize nerves and surrounding structures, helping to identify nerve compression, tumors, herniated discs, or other structural abnormalities that might be causing neuropathy.
As Watson and Dyck emphasize in "Peripheral Neuropathy: A Practical Approach to Diagnosis and Symptom Management" (Mayo Clinic Proceedings), accurate diagnosis is the cornerstone of effective treatment. Finding the cause allows for targeted treatment, which can often halt progression and sometimes even reverse nerve damage.
Available Treatment Options for Managing Symptoms
Treating neuropathy is a multi-faceted endeavor, often requiring a combination of approaches custom to the individual. The primary focus is always on addressing the underlying cause (if identifiable) and, if not, or while the underlying condition is being managed, symptom relief becomes paramount.
-
Addressing the Underlying Cause: This is the most effective long-term strategy for many neuropathies.
- Diabetes: Strict blood glucose control is non-negotiable.
- Vitamin Deficiencies: Supplementation is prescribed to restore healthy levels.
- Autoimmune Conditions: Immunosuppressants, steroids, intravenous immunoglobulin (IVIg), or plasmapheresis may be used.
- Medication-Induced: The offending medication may be adjusted or discontinued (under medical supervision).
- Compression: Physical therapy, splinting, or surgical decompression can relieve pressure on nerves.
-
Pain Management Strategies: Neuropathic pain can be persistent and severe, requiring specialized approaches:
-
Oral Medications:
- Anticonvulsants: Gabapentin and pregabalin are commonly prescribed and effective for many types of neuropathic pain. Other options include oxcarbazepine, carbamazepine, and lamotrigine.
- Antidepressants: Tricyclic antidepressants (e.g., amitriptyline, nortriptyline) and serotonin-norepinephrine reuptake inhibitors (SNRIs like duloxetine, venlafaxine, milnacipran) can help by affecting pain pathways in the brain.
- Opioids: While effective for severe pain, strong opioids are generally used with caution due to the risk of dependence and side effects. Tramadol is a weaker opioid sometimes used for neuropathic pain.
- NSAIDs and Acetaminophen: Generally less effective for neuropathic pain compared to other types of pain.
-
Topical Treatments: Creams, gels, or patches applied directly to the skin can provide localized relief:
- Lidocaine patches/creams: Provide localized numbing relief.
- Capsaicin cream: Derived from chili peppers, it can deplete pain-signaling chemicals in nerve endings, offering relief over time.
-
Oral Medications:
Neuropasil Nerve Pain Relief Cream: For immediate, targeted relief from the burning, tingling, and aching of neuropathy, we've developed Neuropasil Nerve Pain Relief Cream. Our unique formula leverages natural ingredients like menthol, which provides a cooling and soothing sensation, aloe for its anti-inflammatory properties, and urea to improve the penetration of active ingredients deep into the skin. This powerful combination works to soothe damaged and inflamed nerves, offering a natural option for managing nerve pain. Many of our loyal customers, including athletes and individuals with conditions like sciatica and fibromyalgia, find it invaluable for managing their daily discomfort. You can find more info about our Nerve Pain Relief Cream on our website.
-
Supportive Therapies:
- Physical Therapy: Custom exercises can improve muscle strength, flexibility, balance, and coordination. Physical therapists can also recommend assistive devices like braces, splints, or orthopedic shoes to aid mobility and prevent falls.
- Occupational Therapy: Helps individuals adapt daily tasks and environments to maintain independence despite nerve damage.
- Transcutaneous Electrical Nerve Stimulation (TENS): This non-invasive therapy uses mild electrical currents delivered through electrodes placed on the skin to interrupt pain signals. While some studies suggest it can offer relief, especially for diabetic peripheral neuropathy, the overall evidence for its effectiveness in general neuropathic pain is still considered low to moderate.
- Psychological Support: Living with chronic pain can be emotionally taxing. Counseling, cognitive behavioral therapy (CBT), and support groups can help individuals develop coping strategies and manage the psychological impact of neuropathy.
- Complementary Treatments: Some individuals explore acupuncture, massage, or tai chi for pain relief, though scientific evidence for their efficacy in neuropathy varies.
Surgery: For cases of nerve compression (like carpal tunnel syndrome) or tumors pressing on nerves, surgical decompression can relieve pressure and restore nerve function. While surgical decompression has shown promise for diabetic peripheral neuropathy in specific cases, it's generally not recommended for widespread neuropathy. Most neuropathies involve scattered nerve damage and are not helped by surgery.
Lifestyle Modifications: Maintaining a healthy lifestyle, including a balanced diet, regular exercise, avoiding smoking, and limiting alcohol, plays a crucial role in supporting nerve health and enhancing the effectiveness of other treatments.
A personalized treatment plan, often involving a combination of these strategies, is key to effectively managing neuropathy symptoms and improving overall well-being.
Living With, Preventing, and Differentiating Neuropathy
Living with neuropathy is a journey that often requires significant lifestyle adjustments and proactive health management. Understanding what is neuropathy also includes knowing how to prevent it and how it differs from other conditions with similar symptoms.
Can Neuropathy Be Prevented?
While not all forms of neuropathy are preventable, especially those with genetic causes, a significant number of acquired neuropathies can be avoided or their progression slowed through diligent lifestyle choices and medical management.
-
Managing Medical Conditions: This is arguably the most impactful preventive measure.
- Diabetes: Strict control of blood sugar levels is paramount. Maintaining target glucose levels through diet, exercise, and medication can prevent or significantly delay the onset and progression of diabetic neuropathy.
- Other Chronic Diseases: Effectively managing kidney disease, liver disease, autoimmune disorders, and hypothyroidism is crucial, as their uncontrolled progression can lead to nerve damage.
-
Healthy Diet: A balanced, nutrient-rich diet supports overall nerve health. Focus on:
- Fruits, Vegetables, and Whole Grains: Provide essential vitamins, minerals, and antioxidants.
- Lean Protein: Important for nerve repair and maintenance.
- Adequate Vitamins: Ensure sufficient intake of B vitamins (B1, B6, B12), vitamin E, and copper. Deficiencies in these are well-known causes of neuropathy. If you follow a vegetarian or vegan diet, discuss B12 supplementation with your doctor.
- Regular Exercise: Physical activity improves circulation, which is vital for delivering oxygen and nutrients to nerves. Aim for 30 minutes to one hour of moderate exercise, at least three times a week, after consulting your healthcare provider. This could include walking, swimming, or cycling.
- Avoiding Toxins: Minimize exposure to industrial chemicals, heavy metals (like lead and mercury), and certain pesticides, which are known neurotoxins.
- Limiting Alcohol: Excessive and chronic alcohol consumption is a direct cause of alcoholic neuropathy and can exacerbate other forms of nerve damage. Reducing or eliminating alcohol intake is a key preventive step.
-
Foot Care: For those at risk or already experiencing early symptoms, meticulous foot care is crucial.
- Inspect your feet daily for cuts, blisters, or sores, as reduced sensation might prevent you from feeling them.
- Wear comfortable, well-fitting, closed-toe shoes to protect your feet from injury.
- Treat even minor injuries promptly to prevent infection, especially if you have diabetes.
- Safety Measures: Use appropriate safety equipment during work or sports activities to prevent injuries that could damage nerves.
By embracing these proactive strategies, we can significantly reduce the risk of developing neuropathy or slow its progression, maintaining better nerve health for longer.
Potential Complications and Distinctions
Left untreated or poorly managed, neuropathy can lead to a cascade of serious complications that drastically affect quality of life:
- Foot Ulcers and Infections: Loss of sensation, particularly in the feet, means minor cuts, blisters, or pressure points can go unnoticed. These can quickly develop into ulcers and infections, which, if severe, may lead to gangrene and necessitate amputation, especially in individuals with diabetes.
- Falls and Injuries: Muscle weakness, impaired balance, and reduced sensation increase the risk of falls, leading to fractures, sprains, and other traumatic injuries. Simple home modifications like removing tripping hazards and installing handrails can help.
- Chronic Pain: Persistent neuropathic pain can be debilitating, causing sleep disturbances, anxiety, depression, and a significant reduction in daily activities and overall well-being.
- Decreased Quality of Life: The cumulative effect of pain, functional limitations, and emotional distress can severely impact an individual's ability to work, socialize, and enjoy life.
- Autonomic Complications: If autonomic nerves are significantly damaged, complications can be life-threatening, including severe heart rhythm abnormalities, dangerous fluctuations in blood pressure, and profound digestive issues that impair nutrient absorption.
It's also important to understand how neuropathy differs from other conditions that cause nerve-related symptoms:
| Feature | Neuropathy | Neuralgia Neuropathy is a complex condition affecting the peripheral nervous system, leading to varied symptoms like pain, numbness, and weakness. It's crucial to identify the underlying cause, whether it's diabetes, deficiencies, or other factors. While a full cure isn't always possible, effective management through medical treatments, lifestyle changes, and topical solutions like Neuropasil can significantly improve life quality. Early diagnosis and proactive care are our best tools against neuropathy's progression.
References
- Mayo Clinic. (n.d.). Peripheral neuropathy - Symptoms and causes. Retrieved from https://www.mayoclinic.org/diseases-conditions/peripheral-neuropathy/symptoms-causes/syc-20352061
- National Institute of Neurological Disorders and Stroke. (2023, August 16). Peripheral Neuropathy Fact Sheet. Retrieved from https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Peripheral-Neuropathy-Fact-Sheet
- Cleveland Clinic. (2023, April 20). Peripheral Neuropathy: What It Is, Symptoms & Treatment. Retrieved from https://my.clevelandclinic.org/health/diseases/14737-peripheral-neuropathy
- Singh, V. P., Bali, A., Singh, N., & Jaggi, A. S. (2014). Advanced glycation end products and diabetic complications. The Korean Journal of Physiology & Pharmacology, 18(1), 1–14. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3951818
- Sugimoto, K., Yasujima, M., & Yagihashi, S. (2008). Role of advanced glycation end products in diabetic neuropathy. Current Pharmaceutical Design, 14(10), 953–61. Retrieved from https://pubmed.ncbi.nlm.nih.gov/18473845
- Watson, J. C., & Dyck, P. J. (2015). Peripheral Neuropathy: A Practical Approach to Diagnosis and Symptom Management. Mayo Clinic Proceedings, 90(7), 940–51. Retrieved from https://pubmed.ncbi.nlm.nih.gov/26141332
- Derry, S., Wiffen, P. J., Aldington, D., & Moore, R. A. (2015). Nortriptyline for neuropathic pain in adults. The Cochrane Database of Systematic Reviews, 2015(1), CD011209. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6485407
- Moore, R. A., Derry, S., Aldington, D., Cole, P., & Wiffen, P. J. (2015). Amitriptyline for neuropathic pain in adults. The Cochrane Database of Systematic Reviews, 2015(7), CD008242. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6447238
- Lunn, M. P., Hughes, R. A., & Wiffen, P. J. (2014). Duloxetine for treating painful neuropathy, chronic pain or fibromyalgia. The Cochrane Database of Systematic Reviews, 2015(1), CD007115. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10711341
- Wiffen, P. J., Derry, S., Bell, R. F., Rice, A. S., Tölle, T. R., Phillips, T., & Moore, R. A. (2017). Gabapentin for chronic neuropathic pain in adults. The Cochrane Database of Systematic Reviews, 2017(6), CD007938. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6452908
- Derry, S., Bell, R. F., Straube, S., Wiffen, P. J., Aldington, D., & Moore, R. A. (2019). Pregabalin for neuropathic pain in adults. The Cochrane Database of Systematic Reviews, 2019(1), CD007076. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6353204
- McNicol, E. D., Midbari, A., & Eisenberg, E. (2013). Opioids for neuropathic pain. The Cochrane Database of Systematic Reviews, 2019(8), CD006146. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6353125
- Derry, S., Rice, A. S., Cole, P., Tan, T., & Moore, R. A. (2017). Topical capsaicin (high concentration) for chronic neuropathic pain in adults. The Cochrane Database of Systematic Reviews, 2017(1), CD007393. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6464756
- Gibson, W., Wand, B. M., & O'Connell, N. E. (2017). Transcutaneous electrical nerve stimulation (TENS) for neuropathic pain in adults. The Cochrane Database of Systematic Reviews, 2017(9), CD011976. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6426434
- Healthdirect. (n.d.). Neuropathy. Retrieved from https://www.healthdirect.gov.au/neuropathy
- NewYork-Presbyterian. (n.d.). Neuropathy: Symptoms & Causes. Retrieved from https://www.nyp.org/neuro/neuromuscular-disorders/neuropathy
- Mount Sinai. (n.d.). Peripheral neuropathy Information. Retrieved from https://www.mountsinai.org/health-library/diseases-conditions/peripheral-neuropathy
- NYU Langone Health. (n.d.). Peripheral Neuropathy. Retrieved from https://nyulangone.org/conditions/peripheral-neuropathy
- Yale Medicine. (n.d.). Neuropathy > Fact Sheets. Retrieved from https://www.yalemedicine.org/conditions/neuropathy
- Lift Chiropractic. (n.d.). What is Neuropathy?. Retrieved from https://www.elevatetolife.com/post/what-is-neuropathy
- Neighborhood Neuropathy. (n.d.). Neuropathy Explained. Retrieved from https://www.neighborhoodneuropathy.com/news/neuropathy-explained
- Citizens Hospitals. (n.d.). Understanding Neuropathy: Causes and Management of Chronic Nerve Pain. Retrieved from https://www.citizenshospitals.com/blogs/understanding-neuropathy-causes-and-management-of-chronic-nerve-pain
- Scott Zimmerman DPM. (n.d.). Jessie Holloway. Retrieved from https://www.scottzimmermandpm.com/health-issues
- MedlinePlus. (n.d.). Ulnar neuropathy. Retrieved from https://medlineplus.gov/ency/article/000789.htm
- MedlinePlus. (n.d.). Multiple mononeuropathy. Retrieved from https://medlineplus.gov/ency/article/000782.htm
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). (n.d.). Diabetic Neuropathy. Retrieved from https://www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems/nerve-damage-diabetic-neuropathies
- National Heart, Lung, and Blood Institute (NHLBI). (n.d.). Atherosclerosis. Retrieved from https://www.nhlbi.nih.gov/health/atherosclerosis
- National Institute of Allergy and Infectious Diseases (NIAID). (n.d.). Lyme disease. Retrieved from https://www.niaid.nih.gov/diseases-conditions/lyme-disease
- National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS). (n.d.). Carpal tunnel syndrome. Retrieved from https://www.niams.nih.gov/health-topics/carpal-tunnel-syndrome
- Cancer.gov. (n.d.). Chemotherapy-induced peripheral neuropathy (CIPN). Retrieved from https://www.cancer.gov/about-cancer/treatment/side-effects/nerve-problems
- Wiktionary. (n.d.). -pathy. Retrieved from https://en.wiktionary.org/wiki/-pathy#English
- Wiktionary. (n.d.). neuro-. Retrieved from https://en.wiktionary.org/wiki/neuro-#English
- Wiktionary. (n.d.). numb. Retrieved from https://en.wiktionary.org/wiki/numb
- Wiktionary. (n.d.). neuritis. Retrieved from https://web.archive.org/web/20090628224336/http://www.mercksource.com/pp/us/cns/cnshldorlands_split.jsp?pg=/ppdocs/us/common/dorlands/dorland/six/000071661.htm
- The Cochrane Database of Systematic Reviews. (n.d.). Cochrane Reviews for Neuropathic Pain. Retrieved from various links provided in research for specific medications (e.g., gabapentin, pregabalin, amitriptyline, duloxetine, opioids, capsaicin, TENS).
- Wikipedia. (n.d.). Peripheral neuropathy. Retrieved from https://en.wikipedia.org/wiki/Peripheral_neuropathy














