Understanding the Source of Your Radiating Pain
Nerve root pain occurs when pressure on nerve roots near the spine causes sharp, shooting sensations that radiate far from the source. Unlike localized muscle soreness, this pain travels along nerve pathways, often from your back into your arms or legs.
Quick Facts About Nerve Root Pain:
- Also called: Radiculopathy or pinched nerve
- Common locations: Neck (cervical), upper back (thoracic), or lower back (lumbar)
- Key symptom: Pain that radiates away from the spine
- Most common type: Sciatica (lumbar radiculopathy affecting the leg)
- Recovery rate: 75% of people with sciatica improve within 28 days
How It Differs From Regular Back Pain:
- Travels along specific nerve pathways (dermatomes)
- Often described as sharp, burning, or electric-like
- May include numbness, tingling, or weakness
- Usually affects one side of the body
- Pain is typically worse in the limb than the back
If you're dealing with radiating pain down your arm or leg, understanding the cause is crucial. It's your nervous system signaling that something needs attention.
The good news is that most nerve root pain resolves with proper care. About 90% of people who experience sciatica don't have a recurrence within ten years.
What is Nerve Root Pain and How Does it Feel?
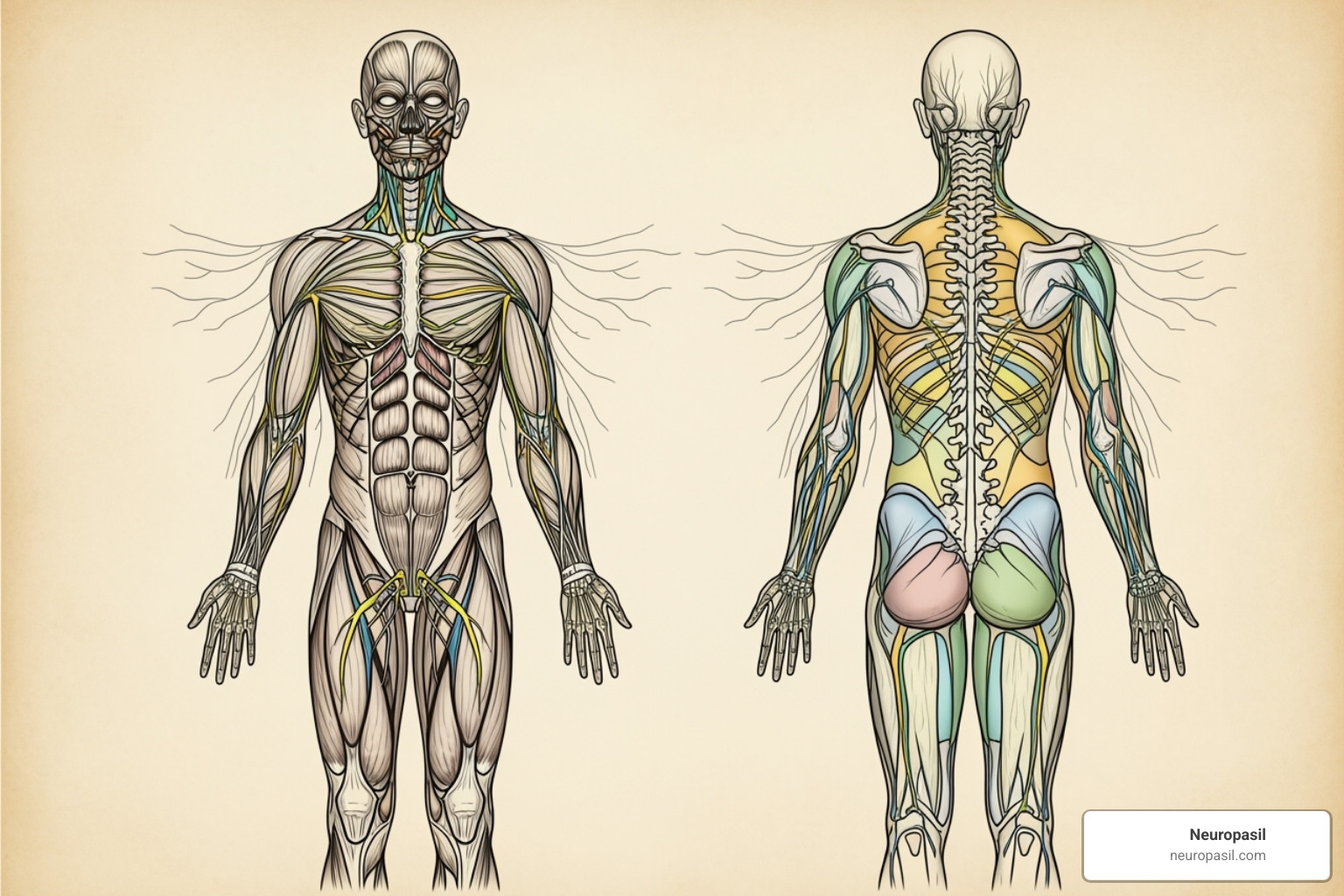
Think of nerve roots as electrical wires exiting your spinal cord. When one gets pinched or irritated, it causes nerve root pain. These spinal nerves carry messages between your brain and body, so when a nerve root is compressed, it can't function properly. The result is pain, tingling, numbness, or weakness that follows a specific pathway.
This is what makes nerve root pain so distinctive: it follows what doctors call "dermatomes." Each nerve root supplies sensation to a particular area of skin. When a nerve root in your lower back is pinched, you might feel pain shooting down to your toes because the nerve is following its predetermined path.
This predictable pattern separates nerve root pain from regular muscle soreness, which tends to be dull, achy, and localized. Nerve root pain, however, is often described as sharp, burning, or electric.
Understanding the Symptoms of Nerve Root Pain
When a nerve root is in distress, it sends clear warning signals that set it apart from other types of pain.
- Sharp, shooting pain can feel like a sudden electric shock.
- A burning sensation may travel along an arm or leg.
- Tingling or "pins and needles" occurs because the compressed nerve can't transmit normal sensation signals.
- Numbness can make parts of your body feel disconnected or "dead."
- Muscle weakness can make everyday tasks like gripping objects or lifting your arm difficult.
- Increased sensitivity can make even light touch feel painful.
These symptoms often worsen with movements that increase pressure around the spine, like coughing or sneezing. For more details, see our guide on Sciatica Pain Symptoms.
Pain Location: Cervical, Thoracic, and Lumbar Radiculopathy
Where you feel nerve root pain points directly to the source of the problem in your spine.
Cervical radiculopathy affects nerve roots in your neck, causing pain (also called brachial neuralgia) that travels down your arm and into your fingers. This can make simple tasks difficult and helps pinpoint the affected nerve root.
Thoracic radiculopathy is the rarest type, affecting the upper back. Pain can wrap around your chest or abdomen in a band-like pattern and is sometimes mistaken for heart or digestive issues, making a proper diagnosis crucial.
Lumbar radiculopathy is the most common type, with sciatica being its most famous form. When a nerve root in your lower back is compressed, pain shoots from your lower back, through your buttock, and down your leg, often past the knee. The leg pain is usually much worse than any back pain. Your brain interprets these signals as coming from your leg because that's where the nerve provides sensation. For a deeper dive, read our article on Sciatic Nerve Pain.
Understanding these types of nerve root pain helps you communicate more effectively with your doctor.
Uncovering the Common Causes and Risk Factors
Nerve root pain is typically a symptom of an underlying condition putting pressure on a spinal nerve root.
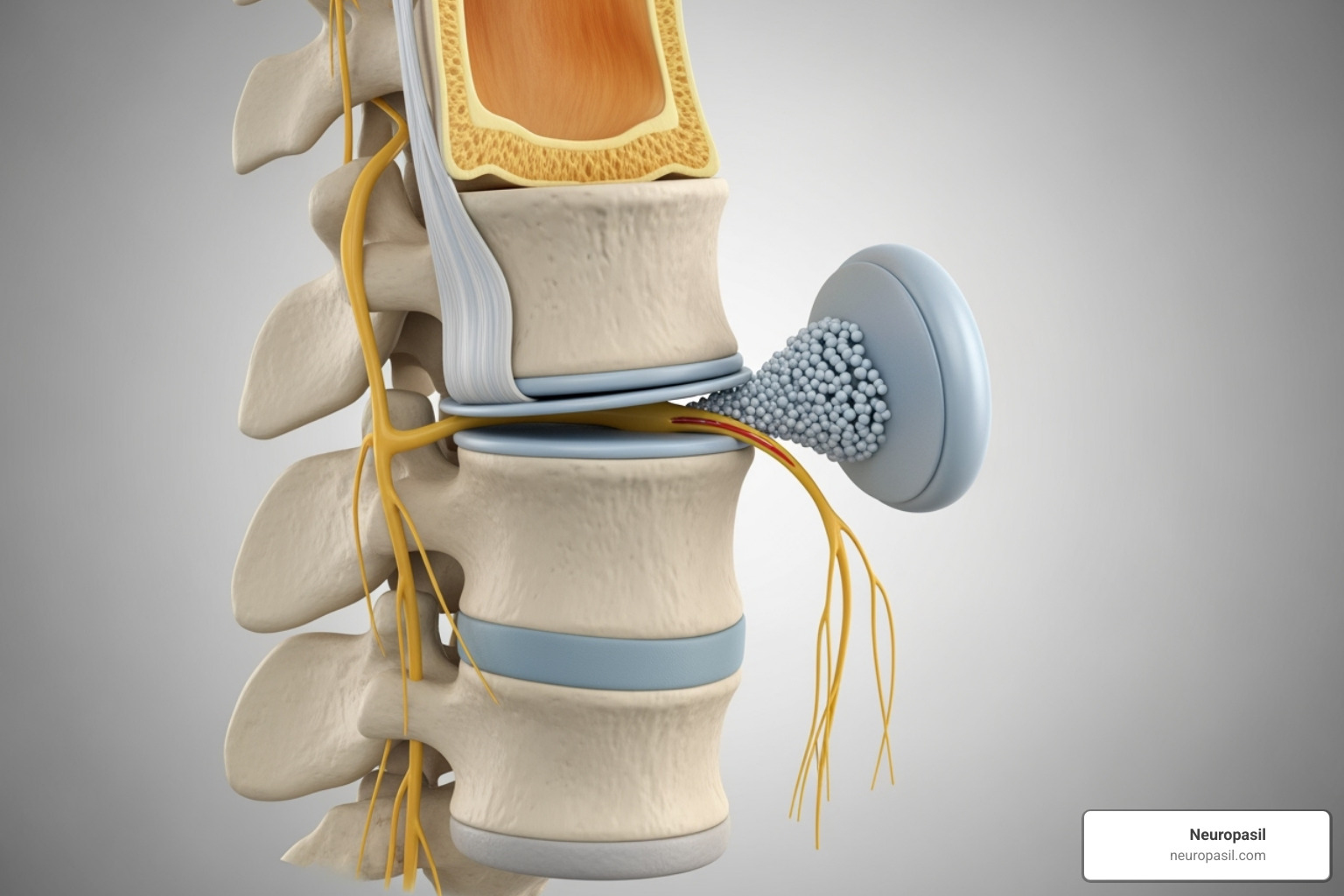
Common culprits include:
- Herniated Discs: Often called a "slipped disk," this occurs when the soft center of a spinal disc pushes through its outer layer, pressing on a nerve root. These often shrink over time, aiding natural recovery.
- Spinal Stenosis: A narrowing of spaces within the spine, which can be caused by bone spurs or thickened ligaments, putting pressure on the spinal cord and nerve roots.
- Bone Spurs (Osteophytes): Bony growths that can develop on vertebrae due to wear and tear (osteoarthritis) and impinge on nerves.
- Degenerative Disc Disease: Age-related water loss in spinal discs makes them less flexible, leading to bulging or tears that can cause nerve compression.
- Spondylosis: A general term for age-related wear and tear on the spine that can lead to bone spurs and disc degeneration.
- Spinal Injury or Trauma: Accidents or falls can cause disc herniation or fractures that impinge on nerve roots.
- Tumors or Cysts: Though less common, growths near the spine can press on nerve roots.
- Inflammatory Diseases: Conditions like rheumatoid arthritis can cause inflammation affecting spinal structures.
- Infections: Rare infections like tuberculosis, Lyme disease, or shingles can sometimes affect nerve roots.
- Diabetes Mellitus: This condition can damage nerves throughout the body, including nerve roots.
Several risk factors also increase the likelihood of developing nerve root pain:
- Aging: Natural changes like disc degeneration and bone spurs become more common. Radiculopathy is more frequent in people over 50, with sciatica peaking around age 35-40.
- Poor Posture: Places undue stress on the spine and discs over time.
- Sedentary Lifestyle: Can lead to weak core muscles and stiff spinal structures. Sedentary jobs pose a higher risk.
- Genetics: Some people may have a genetic predisposition to spinal conditions.
- Obesity: Excess weight adds strain to the spine, especially the lower back.
- Repetitive Activities: Certain jobs or hobbies can contribute to spinal wear and tear. (Note: heavy manual labor is not a clear risk factor for sciatica).
- Pregnancy: Weight gain and hormonal changes can put pressure on spinal nerves.
Diagnosing and Treating Nerve Root Pain
Getting the right diagnosis for nerve root pain involves your doctor piecing together clues from your history and a physical exam.
The process starts with a detailed medical history, where you'll describe your pain's onset, characteristics, and triggers. Your doctor will also ask about injuries and relevant family history.
Next is a physical examination to test nerve and muscle function. This includes muscle strength tests, reflex tests with a rubber hammer, and sensation tests using light touch to map out numbness. Your doctor will also observe your posture and how you walk and move to see what triggers your pain.
| Treatment Type | Approach | When it's used |
|---|---|---|
| Non-Surgical | Physical therapy, medication, injections, activity modification, lifestyle changes | First-line treatment for most cases, especially if symptoms are not severe or rapidly worsening |
| Surgical | Procedures to decompress nerves or stabilize the spine (e.g., discectomy, laminectomy, fusion) | When conservative treatments fail, for severe neurological deficits, or in emergencies (e.g., Cauda Equina Syndrome) |
How a Doctor Diagnoses the Problem
While a physical exam provides strong hints, imaging tests offer a clear window into your spine.
- MRI scans are the gold standard, providing detailed images of soft tissues like herniated discs, inflamed nerves, and spinal stenosis.
- CT scans excel at showing bone structures, making them helpful for spotting bone spurs or fractures. A CT myelogram uses dye for even better images of nerve compression.
- X-rays are valuable for seeing the overall alignment of your spine and checking for issues like severe disc narrowing.
- Electromyography (EMG) and nerve conduction studies measure electrical activity in nerves and muscles to confirm nerve damage and pinpoint the affected roots.
For more on diagnosis, the Cleveland Clinic's comprehensive guide offers excellent medical insights.
Non-Surgical Treatments for Nerve Root Pain
Most people with nerve root pain get better without surgery by supporting the body's natural healing process.
Physical therapy is key, with exercises to strengthen core muscles, improve flexibility, and relieve pressure on nerves. The McKenzie method, for example, helps centralize pain back toward the spine, a sign of improvement.
Activity modification involves smart adjustments to your daily routine, like improving your workstation setup or using proper lifting techniques.
For medication, NSAIDs (ibuprofen, naproxen) are often the first line of defense to reduce inflammation. For more stubborn cases, corticosteroid injections (epidural injections or nerve blocks) deliver powerful anti-inflammatory medicine directly to the problem area. Certain antidepressants and antiseizure medications (like gabapentin) can also be used to treat nerve pain by changing how the nervous system processes pain signals.
At-home management is also crucial. This includes ice therapy for acute pain, heat therapy for muscle tension, and gentle stretching as guided by a physical therapist. Staying active within your comfort zone is vital, as complete bed rest often makes things worse.
When Surgery is Considered
Surgery may be an option for persistent pain that hasn't improved after months of conservative treatment or for significant weakness suggesting ongoing nerve damage.
The most urgent situation is Cauda Equina Syndrome. If you experience numbness between your legs (saddle numbness) and loss of bowel or bladder control, this is a medical emergency requiring immediate surgery to prevent permanent damage.
Surgical procedures include discectomy (removing part of a herniated disc), laminectomy (creating more space for nerves), and spinal fusion (stabilizing vertebrae). Outcomes are generally good, with about 75% of patients feeling much better after sciatica surgery. Serious complications are rare. For more details, the British Association of Spine Surgeons provides excellent resources.
Recovery Outlook and Prevention Strategies
The encouraging news is that nerve root pain is rarely a life sentence. Your body is great at healing, and most people return to normal, active lives.
With the right care and patience, the body can reduce inflammation and even reabsorb problematic disc material on its own.
Key Recovery Statistics:
- 75% of people with sciatica improve within 28 days
- 90% won't experience another episode in the next 10 years after recovery
- Most cases resolve within weeks to months with proper care
The Typical Prognosis and Recovery Time
Time is on your side. Most people feel significantly better within a few days to weeks. For first-time sciatica, the 75% improvement rate within 28 days is a common benchmark, with most patients seeing major improvements by 13 weeks.
During recovery, the body can naturally reabsorb herniated disc material (a process called resorption), reducing pressure on the nerve.
Staying active is crucial. Gentle movement keeps your spine flexible, maintains muscle strength, and promotes healing blood flow. Think "motion is lotion" for your spine.
Recurrence rates are also encouraging. Once an episode of sciatica resolves, there's about a 90% chance it won't return within the next decade. For more on what to expect, see our guide: More on Sciatica Symptoms and recovery.
How to Prevent Nerve Root Pain
Prevention is the best medicine. While you can't control genetics or accidents, you can stack the odds in your favor with smart daily choices.
- Maintain good posture: Proper alignment while sitting, standing, and sleeping reduces unnecessary pressure on your nerve roots.
- Exercise regularly: Consistent movement keeps supporting muscles strong and discs healthy.
- Strengthen your core: Strong abdominal and back muscles act as a natural corset for your spine.
- Manage your weight: Excess weight, especially around your midsection, puts constant stress on your lower back.
- Create an ergonomic workspace: Adjust your chair, monitor, and keyboard to support a natural posture, and take frequent breaks to move.
- Use safe lifting techniques: Always lift with your legs, not your back, and avoid twisting while lifting.
- Stay hydrated: Your spinal discs are mostly water; proper hydration keeps them plump and resilient.
Frequently Asked Questions about Nerve Pain
Here are answers to the most common questions we hear about nerve root pain.
How long does nerve root pain typically last?
Most people feel better within a few days or weeks, though the exact timeline depends on the cause and severity. For first-time sciatica, 75% of people improve within 28 days, with most cases showing significant improvement within 6 to 13 weeks. Some mild symptoms may linger, but the intense pain usually fades much sooner with proper care.
Can nerve root pain go away on its own?
Yes, many cases of nerve root pain resolve on their own. The body has a remarkable ability to heal. For example, it can reabsorb herniated disc material over time, and inflammation around the nerve root can decrease naturally. This is why doctors usually recommend conservative treatments first, giving your body a chance to heal itself.
When is nerve root pain a medical emergency?
While most cases aren't an emergency, certain "red flag" symptoms require immediate medical attention to prevent permanent damage.
Seek emergency care if you experience:
- Loss of bladder or bowel control
- Numbness in the groin or saddle area (inner thighs, buttocks, genital region)
- Severe or rapidly worsening weakness in the legs, such as foot drop or trouble walking
These symptoms may indicate Cauda Equina Syndrome, a serious condition that requires immediate treatment. It's always better to be cautious when these symptoms appear.
Conclusion
You now have a solid understanding of nerve root pain (radiculopathy), which causes sharp, shooting sensations from the spine into the limbs.
The most important takeaway is that your body is remarkably good at healing itself. For sciatica, 75% of people feel significantly better within 28 days. Your nervous system is working hard to restore normal function.
Knowledge is power. Understanding the difference between nerve pain and muscle soreness, recognizing emergency symptoms, and knowing that most cases respond well to conservative care puts you in control. The path to recovery usually involves physical therapy, proper posture, and gentle movement, not surgery.
Early action makes a difference. Taking charge of your nerve health by adjusting your habits or seeking professional help can pay dividends.
At Neuropasil, we believe in supporting your body's capacity to heal. When you're ready to explore complementary approaches for your recovery, we invite you to Explore natural solutions for nerve pain relief.
Your current discomfort is likely temporary. Brighter, pain-free days are ahead.















