Understanding the Most Common Form of Arthritis
Osteoarthritis (OA) is the most prevalent type of arthritis, affecting over 32.5 million adults in the U.S. It's a degenerative joint disease where the protective cartilage on the ends of bones wears down over time, causing pain, stiffness, and reduced mobility. While it can affect any joint, it most commonly impacts the hands, knees, hips, and spine.
Contrary to popular belief, OA isn't just age-related "wear and tear." It's a complex disease affecting the entire joint—cartilage, bone, and surrounding tissues. The cartilage breaks down, bones can change shape, and the joint lining may become inflamed, all contributing to discomfort. After age 50, it becomes more common in women than men.
For active individuals and athletes, understanding OA is crucial for adapting routines and maintaining quality of life. With proper management, it's possible to stay active and find effective relief.
I'm Tony Enrico, and through my work developing pain relief formulas like Neuropasil, I've seen how natural ingredients can ease joint discomfort. My experience shows that combining targeted topical treatments with smart joint care strategies makes a significant difference in managing osteoarthritis symptoms.
Identifying the Signs: Symptoms and Complications
When osteoarthritis develops, symptoms typically appear gradually. What starts as minor stiffness can progress into daily discomfort. Key signs include:
- Pain with movement: Aching in a joint after activity, which may become persistent over time.
- Morning stiffness: Joints feel stiff upon waking, usually lasting less than 30 minutes.
- Swelling and tenderness: Inflammation or fluid buildup can make the joint tender to the touch.
- Loss of flexibility: Difficulty fully bending or straightening a joint, limiting range of motion.
- Grating sensation (crepitus): A grinding or popping sound or feeling as roughened cartilage surfaces rub together.
- Bone spurs: Hard lumps that can form around the affected joint, contributing to pain and stiffness.
How Osteoarthritis Affects Different Joints
Osteoarthritis targets joints differently, especially those that bear weight or perform repetitive motions.
- Hands: Bony enlargements on finger joints (Heberden's and Bouchard's nodes) and pain at the base of the thumb can make gripping difficult.
- Knees: A grinding sensation, feelings of instability, and pain when using stairs are common.
- Hips: Pain often radiates to the groin, inner thigh, or buttocks, making walking and bending uncomfortable.
- Spine: Stiffness and pain in the neck or lower back can occur. In severe cases, bone spurs can press on nerves, causing pain or numbness in the arms or legs.
Potential Complications and Long-Term Effects
Living with osteoarthritis can lead to broader challenges beyond joint pain.
- Chronic pain: Persistent discomfort that can range from a dull ache to sharp pain.
- Reduced mobility: As joint damage progresses, daily tasks like walking or dressing may become difficult.
- Sleep disturbances: Joint pain can make it hard to find a comfortable position, leading to fatigue.
- Depression and anxiety: The emotional toll of chronic pain and lifestyle limitations can be significant.
- Increased risk of falls: Painful, unstable joints and weaker surrounding muscles increase the risk of falls and fractures by up to 30%.
Recognizing these symptoms and potential complications early is the first step toward effective management. With the right strategies, including targeted topical treatments, many people with osteoarthritis continue to live active, fulfilling lives.
Uncovering the Causes, Risks, and Types of Osteoarthritis
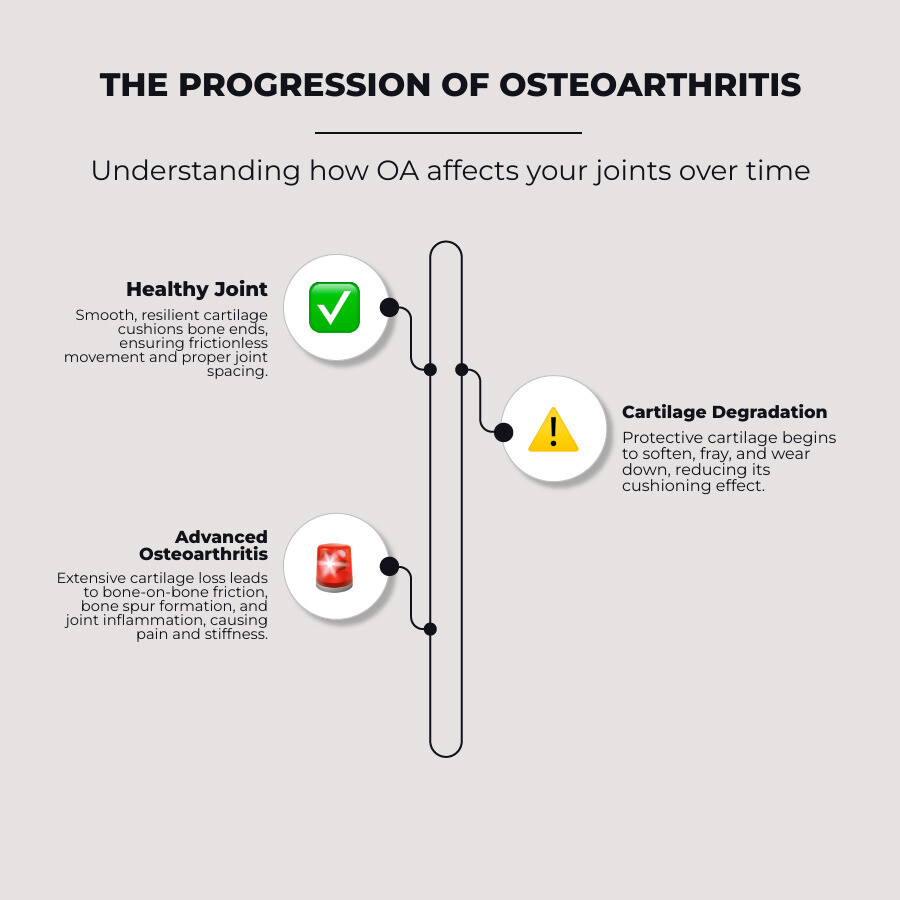
Osteoarthritis is a complex process where the joint's internal structures break down. It begins with the deterioration of cartilage, the smooth tissue cushioning our bones. As cartilage wears away, it leads to painful bone-on-bone friction. The underlying bone may also change and form bone spurs, while the joint lining can become inflamed, causing further pain and stiffness.
Several factors can increase your risk of developing osteoarthritis:
- Older Age: The risk increases with time, with over 80% of adults over 55 showing some signs of OA on X-rays.
- Gender: Women are more likely to develop OA after age 50, especially post-menopause.
- Obesity: Extra weight adds stress to weight-bearing joints like knees and hips. Fat tissue also produces inflammatory proteins that can damage joints.
- Previous Injuries: A past joint injury or surgery can alter joint mechanics and lead to OA years later.
- Repetitive Stress: Certain jobs or sports that place repeated stress on a particular joint can accelerate wear.
- Family History: A genetic predisposition can make you more likely to develop the condition.
- Bone Deformities: Improperly formed joints can lead to uneven wear and tear.
- Metabolic Diseases: Conditions like diabetes can affect cartilage health, making it more prone to breakdown.
Primary vs. Secondary Osteoarthritis Explained
Osteoarthritis is generally categorized into two main types:
Primary Osteoarthritis: This is the most common form, developing gradually over many years without a single, clear cause. It's often linked to aging, genetics, and other cumulative risk factors.
Secondary Osteoarthritis: This type is triggered by a specific cause. It can result from a previous joint injury, another form of arthritis like rheumatoid arthritis, or a metabolic disease like diabetes. Because there's an identifiable trigger, it can sometimes develop in younger individuals.
Knowing your risk factors is empowering. It allows you to make informed decisions about weight management, joint protection, and when to seek professional help for persistent pain.
Diagnosis and When to Seek Medical Help
If persistent joint pain is interfering with your life, a healthcare provider can determine the cause. The diagnostic process is systematic and designed to get a clear picture of your joint health.
For more information, the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) is an excellent resource: Information on Osteoarthritis Diagnosis from NIAMS
The Diagnostic Process: What to Expect
No single test diagnoses osteoarthritis, so doctors use a combination of methods:
- Physical Examination: Your doctor will check your joints for tenderness, swelling, and range of motion, listening for any grinding sounds (crepitus).
- Medical History Review: Discussing your symptoms, past injuries, and family history helps identify patterns consistent with OA.
- X-rays: This is often the first imaging test. It can reveal joint space narrowing and bone spurs, which are key signs of osteoarthritis.
- Magnetic Resonance Imaging (MRI): An MRI provides more detailed images of soft tissues like cartilage and ligaments and may be used if the diagnosis is unclear.
- Blood Tests: These are used to rule out other types of arthritis, such as rheumatoid arthritis, which require different treatments.
- Joint Fluid Analysis: In some cases, a fluid sample may be drawn from the joint to check for infection or gout crystals.
When to See a Doctor for Your Joint Pain
Don't wait until the pain is unbearable. Early intervention often leads to better long-term outcomes. You should see a doctor if:
- Pain is persistent or worsening and doesn't improve with rest.
- Symptoms interfere with daily activities like walking, sleeping, or working.
- You experience joint swelling, redness, or instability that doesn't resolve.
Getting an accurate diagnosis is the first step toward creating an effective treatment plan, slowing the progression of osteoarthritis, and maintaining your quality of life.
A Comprehensive Approach to Managing Osteoarthritis
While there is no cure for osteoarthritis, the condition is highly manageable. The goals are to manage symptoms, improve joint function, and slow the disease's progression. A comprehensive approach combining lifestyle changes, targeted treatments, and self-care can help you maintain an active, fulfilling life.

Lifestyle Modifications and Self-Care Strategies
Powerful management tools often start at home with practical, daily changes.
- Low-Impact Exercise: Movement is medicine for arthritic joints. Activities like walking, swimming, cycling, and gentle yoga strengthen muscles that support your joints without adding stress. Aim for about 150 minutes of moderate activity per week, starting with what you can manage.
- Weight Management: Losing even a small amount of weight can significantly reduce joint pain. Every pound lost removes four pounds of pressure from your knees and hips.
- Healthy Diet: An anti-inflammatory diet rich in fruits, vegetables, whole grains, and omega-3 fatty acids can help reduce inflammation and support a healthy weight.
- Heat and Cold Therapy: Use a warm bath or heating pad to ease stiffness and a cold pack to numb pain and reduce swelling.
- Joint Protection: Be mindful of how you move, take breaks during repetitive tasks, and use tools that make daily activities easier on your joints.
For more pain management strategies, explore our guide: Managing Arthritis Pain: A Guide to Long-Lasting Relief
Targeted Relief for Osteoarthritis Pain
When you need direct relief, targeted treatments can provide the comfort needed to stay active.

- Topical Pain Relievers: Creams and gels are excellent for localized joint pain, delivering relief directly to the source with fewer systemic side effects. This is why we developed Neuropasil Nerve Pain & Muscle Cream. Its natural formula with aloe, urea, and menthol provides fast, soothing relief for joint discomfort and associated muscle soreness.
- Physical and Occupational Therapy: A physical therapist can design a personalized exercise program to improve strength and flexibility. An occupational therapist can teach you new ways to perform daily tasks with less joint stress.
- Assistive Devices: Braces, shoe inserts, or canes can provide stability, reduce pain, and help you move with confidence.
Advanced Options for Severe Osteoarthritis
If conservative treatments no longer provide enough relief, it may be time to discuss advanced options with your healthcare provider. This is a logical next step in your care journey. Even with severe osteoarthritis, the focus remains on maximizing function and managing symptoms through supportive care, which may include more intensive therapies or different medications. Ongoing self-care, including the use of topical treatments like Neuropasil, remains a crucial part of your management plan.
Frequently Asked Questions about Osteoarthritis
Here are clear, honest answers to the most common questions about living with osteoarthritis.
Can osteoarthritis be cured?
No, a cure for osteoarthritis does not currently exist. The damage to cartilage and joint structures is generally permanent. However, this doesn't mean you are without options. Treatment focuses on effectively managing symptoms, slowing the condition's progression, and maintaining your quality of life so you can continue doing the activities you love.
What is the best exercise for someone with osteoarthritis?
There isn't one single "best" exercise, as the ideal routine depends on your affected joints and fitness level. However, the most beneficial types of movement include:
- Low-impact aerobic exercises: Walking, swimming, water aerobics, and cycling are excellent for cardiovascular health without stressing joints.
- Strengthening exercises: Strong muscles act as shock absorbers for your joints. A physical therapist can guide you on targeting the right muscle groups.
- Flexibility and balance exercises: Gentle stretching, yoga, and Tai Chi can combat stiffness and reduce your risk of falls.
Always consult a healthcare provider before starting a new exercise program.
Does diet play a role in managing osteoarthritis?
Yes, your diet can significantly impact your symptoms. While no diet can cure osteoarthritis, focusing on these areas can help:
- Maintaining a healthy weight: This is the most critical dietary factor. Losing excess weight dramatically reduces stress on weight-bearing joints like the knees and hips.
- Eating anti-inflammatory foods: A diet rich in colorful fruits, vegetables, whole grains, and lean proteins may help reduce inflammation.
- Consuming Omega-3 fatty acids: Found in fatty fish, walnuts, and flaxseeds, these have well-documented anti-inflammatory properties.
- Ensuring adequate Vitamin D and Calcium: These nutrients are vital for bone health, which provides the foundation for your joints.
A healthy diet is a key component of your overall osteoarthritis management plan, especially when combined with exercise and targeted treatments like our Neuropasil cream.
Conclusion: Taking Control of Your Joint Health
We've covered what osteoarthritis is, how to recognize its signs, and the many ways you can effectively manage this common condition. The most important takeaway is this: osteoarthritis is manageable, and it does not have to control your life.
Empowerment comes from understanding your condition and taking proactive steps. By combining lifestyle strategies like low-impact exercise and weight management with targeted treatments, you can significantly improve your daily comfort and mobility.
This is where products like our Neuropasil Nerve Pain & Muscle Cream can make a real difference. Our natural formula, with Aloe, Urea, and Menthol, is designed to provide soothing relief right where you need it, helping with the joint discomfort and muscle tension that often accompany osteoarthritis.
Don't let joint discomfort hold you back. Take the first step toward better joint health today. Your future self will thank you for it.
Find targeted, soothing relief for your joint discomfort with our Nerve Pain & Muscle Cream















