Why Diabetic Foot Pain Affects Millions of Americans Daily
Diabetic foot pain affects up to 50% of people with diabetes, making simple activities like walking or standing a painful challenge. This discomfort stems from nerve damage caused by high blood sugar, creating sensations from burning and tingling to sharp pains.
Quick Relief Guide for Diabetic Foot Pain:
- Immediate relief: Apply topical nerve pain relief cream directly to affected areas
- Daily management: Control blood sugar levels and inspect feet regularly
- Long-term prevention: Wear proper footwear and maintain good circulation
- Emergency signs: See a doctor for non-healing sores, infections, or loss of feeling
The main cause is diabetic neuropathy, where high glucose levels damage nerves in your feet. Poor circulation worsens this by slowing healing and increasing infection risk.
But here's the encouraging news: you don't have to live with constant foot pain. While diabetes requires ongoing management, targeted relief is possible through simple, effective methods.
I'm Tony Enrico, and I've spent years helping people find fast-acting solutions for nerve discomfort, including diabetic foot pain management. My experience shows that the right approach can provide meaningful relief and support your overall foot health.

Why Diabetes Causes Foot Pain
Understanding what causes diabetic foot pain is the first step toward relief. It's a chain reaction started by high blood sugar that primarily affects the nerves and blood vessels in your feet. Once you understand the cause, you can find effective relief and prevent future issues.
The Primary Culprit: Diabetic Neuropathy
The main cause of diabetic foot pain is diabetic neuropathy—nerve damage from prolonged high blood sugar. High glucose acts like a corrosive element on the delicate nerves in your feet, wearing away their protective coating over time.
This nerve damage is common, affecting up to 50% of people with diabetes, as explained by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK).
Symptoms vary, but often include tingling and numbness (like "pins and needles"), a persistent burning sensation (especially at night), or sharp, shooting pains.
What's particularly concerning is that some people lose sensation entirely, creating a risk for unnoticed injuries from heat, cold, or sharp objects. This loss of protective sensation can lead to serious complications.
Damaged nerves can also cause muscle weakness, affecting balance. Learn more in our guide on Peripheral Neuropathy Symptoms.
The Compounding Factor: Poor Circulation
While nerve damage creates pain, poor circulation makes everything worse. Diabetes also harms blood vessels, leading to a condition called Peripheral Artery Disease (PAD).
Damaged and narrowed blood vessels restrict blood flow, starving your feet of the oxygen and nutrients needed to stay healthy.
This reduced blood flow leads to serious problems. Slow healing becomes a major issue, and even minor cuts can take weeks to heal. It also dramatically increases your infection risk, as infection-fighting cells can't reach the area effectively.
Poor circulation also causes pain, like cramping in your legs and feet during activity, because muscles lack sufficient oxygen.
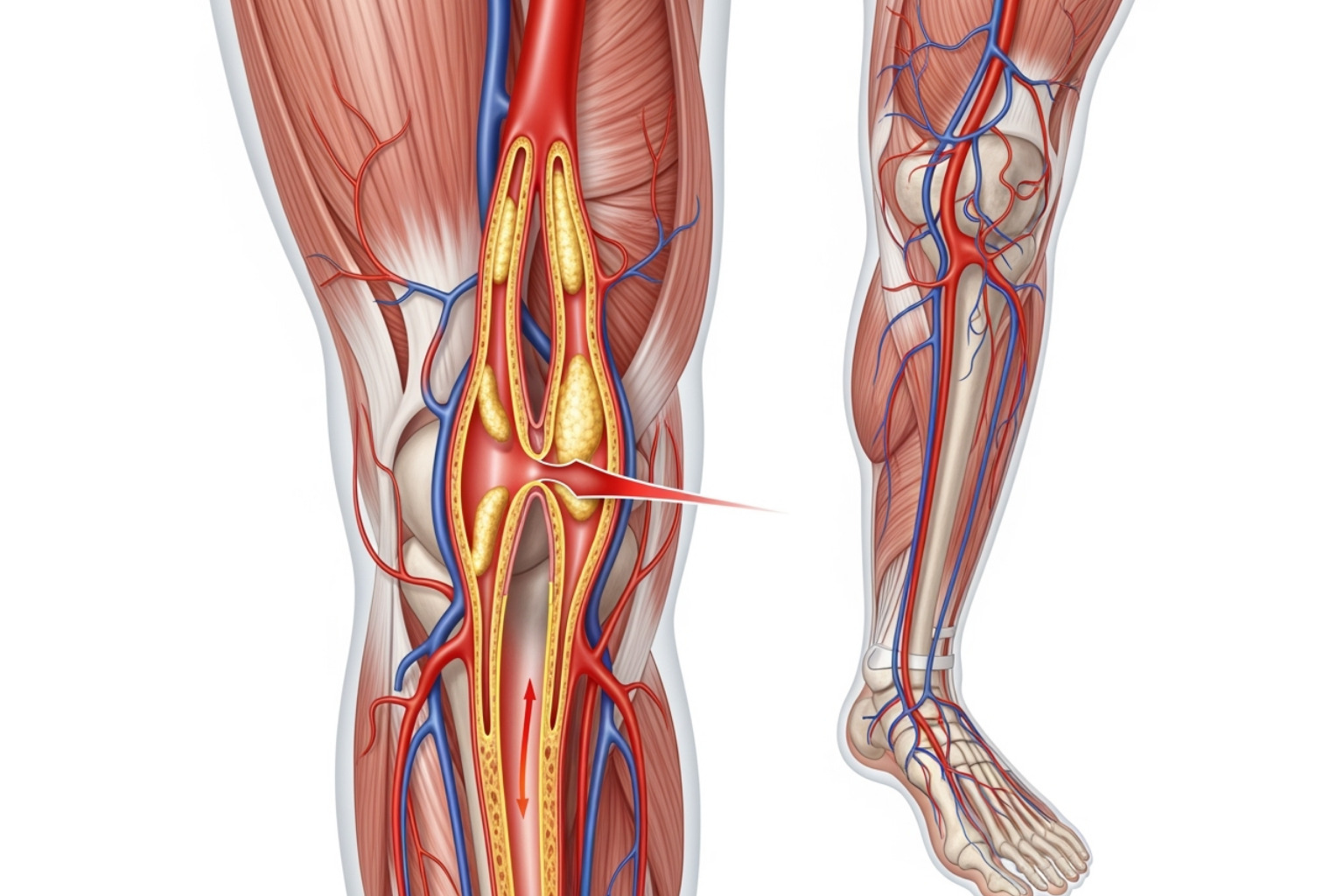
The combination of nerve damage and poor circulation is a dangerous mix. An unfelt injury due to neuropathy can't heal properly due to poor blood flow, which is why managing both is crucial.
This explains why targeted treatments, such as a nerve pain relief cream, are so effective: they address the pain at its source as you manage your overall diabetes.
The Simple, Fast-Acting Solution for Diabetic Foot Pain Relief
When diabetic foot pain disrupts your life, you need fast relief. While long-term management is key, sometimes you need to ease the burning, tingling, or stabbing pain now.
The good news is that targeted topical relief can provide fast-acting comfort, often within minutes.
How Neuropasil Nerve Pain Relief Cream Provides Targeted Relief
Unlike oral painkillers, a quality nerve pain relief cream like Neuropasil works directly at the source of your diabetic foot pain.
When applied to your feet, its active ingredients absorb quickly through the skin to target aggravated nerves. By bypassing the digestive system, it works faster than pills and avoids potential medication interactions.
Our customers often praise its fast absorption, feeling soothing effects in minutes. The cream works by calming overactive nerve endings that send false pain signals.
This localized action makes it highly effective for diabetic foot pain, directly treating the exact spot that hurts. As a nerve and muscle pain relief cream, Neuropasil also tackles the aches and stiffness that often accompany neuropathy.

Key Ingredients in Neuropasil for Effective Relief
Neuropasil's effectiveness comes from a blend of natural and proven ingredients. Developed in New York City, our formula combines nature with science for pain relief.
Menthol gives you an immediate cooling sensation. This helps interrupt those pain signals heading to your brain. It's especially soothing for the burning feelings often tied to diabetic foot pain.
Aloe Vera offers its legendary healing properties, calming and moisturizing dry, sensitive skin while other ingredients target the pain.
Urea is a key ingredient for diabetic foot care. This powerful moisturizer softens rough, dry skin and helps restore the skin's protective barrier, which is often compromised in people with diabetes.
Lidocaine is a powerful topical anesthetic that temporarily blocks nerve signals causing discomfort. It provides noticeable relief from the tingling, burning, and sharp pains of diabetic foot pain.
Together, these ingredients soothe nerves, protect skin, and provide comprehensive comfort for your feet.
A Comprehensive Plan to Prevent and Manage Foot Pain
Finding immediate relief from diabetic foot pain is just the beginning. Building a solid foundation of long-term care is the real game-changer for preventing future issues and serious complications.
Master Your Blood Sugar for Long-Term Nerve Health
Controlling your blood sugar is the most powerful way to prevent diabetic foot pain from worsening. High glucose attacks your nerves, but stable levels act as a shield.
- Maintain Your A1C Target: Keeping your A1C below 7% is a critical nerve protection plan. Tight blood sugar control can prevent nerve damage from progressing and may even improve symptoms like numbness and tingling.
- Eat a Balanced Diet: A diet of lean proteins, healthy fats, vegetables, fruits, and whole grains helps stabilize blood sugar, creating a healing environment for your nerves.
- Stay Active: Regular exercise like walking or swimming helps control blood sugar, improves circulation, and strengthens foot muscles. Always wear proper footwear and start slowly.
- Adhere to Medications: Take your diabetes medications as prescribed. If you're on Metformin, ask your doctor about testing for Vitamin B12 deficiency, as it's crucial for nerve health.
The American Diabetes Association provides excellent guidance on Steps to Prevent or Delay Nerve Damage, emphasizing proactive blood sugar management.
Your Daily Foot Care Checklist to Avoid Complications
Daily foot care is your insurance policy against serious complications. Catching problems early is critical when you have diabetes.

- Daily Inspection: Every day, check your feet for cuts, blisters, redness, swelling, or changes in color. Use a mirror to see the bottoms of your feet and check between your toes.
- Wash Gently: Use lukewarm water and mild soap daily. Avoid soaking. Dry thoroughly, especially between the toes, to prevent fungal infections.
- Moisturize Strategically: Apply a thin layer of unscented cream to the tops and bottoms of your feet to prevent cracking. Never put lotion between your toes, as moisture can cause fungal growth.
- Trim Nails Carefully: Cut toenails straight across and file sharp edges. See a podiatrist for thick, discolored, or hard-to-reach nails.
- Protect from Temperature Extremes: Reduced sensation increases burn risk. Never use heating pads on your feet and test water with your elbow.
- Promote Circulation: When sitting, lift your feet, wiggle your toes, and rotate your ankles to keep blood flowing.
The CDC offers comprehensive information on Diabetes and Your Feet, reinforcing these daily practices.
Choosing the Right Shoes to Prevent Diabetic Foot Pain
For people with diabetes, shoes are medical equipment. The right footwear prevents painful complications like blisters and ulcers.
- Choose Supportive, Cushioned Shoes: Look for good arch support and cushioning to distribute pressure evenly. Cushioned insoles add extra shock absorption.
- Ensure a Wide Toe Box: Your shoes should have enough room for your toes to wiggle freely. Avoid pointed shoes that cramp toes.
- Check for a Smooth Interior: The inside of your shoes should be free of seams or rough spots. Always check for foreign objects before putting them on.
- Wear Seamless, Moisture-Wicking Socks: Choose clean, dry socks made of cotton or moisture-wicking fabrics to prevent friction and irritation.
- Consider Therapeutic Shoes: If you have neuropathy, prescription therapeutic shoes offer superior protection. These are often covered by Medicare and other insurance.
- Never Go Barefoot: Always wear shoes or slippers, even indoors, to protect your feet from injuries you might not feel.
The right footwear is a simple, effective investment in your long-term foot health, preventing injuries that lead to serious diabetic foot pain.
Recognizing Serious Complications and When to See a Doctor
While managing diabetic foot pain is important, it's crucial to know when to seek immediate medical attention. Dangerous complications can develop silently due to reduced sensation from neuropathy. The nerve damage that causes pain can also mask serious injuries, so being alert to visual signs is critical.
- Foot ulcers: These open sores, common in about 15% of people with diabetes, often appear on the ball of the foot or big toe. They require immediate medical evaluation, even if painless, as they can lead to serious infections.
- Infections: Seek urgent care for redness, swelling, warmth, pus, or a foul odor. A minor cut can escalate quickly in people with diabetes.
- Non-healing sores: Any wound that doesn't improve in a few days needs a doctor's evaluation. Slow healing is normal, but no healing is a red flag.
- Skin discoloration and swelling: Purple, blue, or black skin can signal poor circulation or tissue death (gangrene). Sudden or persistent swelling also requires immediate medical attention.
- Charcot foot: This rare but serious condition weakens and fractures foot bones, often without pain. Signs include redness, swelling, and one foot being warmer than the other, which can lead to foot deformity.
- Other warning signs: Sudden loss of feeling, thick or ingrown toenails, and hair loss on the feet and lower legs all warrant a doctor's visit, as they can indicate worsening neuropathy or poor circulation.

Statistics show that untreated ulcers and infections are a leading cause of amputation in people with diabetes, highlighting the need for early detection and professional care.
Don't hesitate to contact your doctor or podiatrist when you notice any of these warning signs. The CDC provides excellent guidance on Diabetes Foot Problems: When to See Your Doctor, outlining specific symptoms that demand professional attention.
While topical treatments provide comfort for daily diabetic foot pain, they are part of a comprehensive care approach that includes knowing when professional help is essential.
Frequently Asked Questions about Diabetic Foot Pain
Living with diabetic foot pain raises many questions. Here are straightforward answers to some of the most common concerns we hear, helping you manage your condition with more confidence.
Can diabetic neuropathy be reversed?
This is a common and important question. While extensive nerve damage is generally considered permanent, that isn't the full story. We can halt its progression and often improve symptoms. The key is controlling your blood sugar. With better blood sugar management, some people see symptoms like numbness and tingling fade within a year.
Even if complete reversal isn't possible, symptom management dramatically improves quality of life. Keeping your A1C under 7% and maintaining a healthy lifestyle helps prevent further damage and leads to more comfortable days.
Are over-the-counter pain pills a good option for diabetic foot pain?
When diabetic foot pain flares up, it's tempting to grab an over-the-counter pain pill, but it's wise to pause if you have diabetes. Oral medications affect your entire system and can pose risks, especially for kidney health. They can also interact with other medications or affect blood sugar.
This is why topical relief is often a better first-line approach. A quality nerve pain relief cream like Neuropasil delivers targeted relief directly to the source, avoiding the systemic risks of oral medications. Always consult your doctor or pharmacist before starting any new medication.
How can I relieve diabetic foot pain at night?
Nighttime diabetic foot pain is a common problem, with burning or tingling often intensifying when you're trying to rest. Here are a few tips:
- Apply Neuropasil cream before bed. Its soothing ingredients calm aggravated nerves, providing relief so you can sleep. Apply it 20-30 minutes before bed to allow for absorption.
- Adjust your sleep environment. Keep bedding loose to avoid pressure on your feet. A bed cradle, which lifts sheets off your feet, can also be very helpful.
- Lift your feet with a pillow to improve circulation and reduce swelling. Gentle stretching, like ankle circles and foot flexing, can also help before bed.
- Try a lukewarm foot soak. Never use hot water. Test the temperature with your elbow first to prevent burns, and dry your feet completely afterward.
Experimenting with these tips can help you find a routine that leads to better, uninterrupted sleep.
Conclusion
Diabetic foot pain doesn't have to control your life. We've explored how high blood sugar damages nerves and blood vessels, leading to the frustrating cycle of pain that disrupts daily activities. But remember: relief is absolutely possible.
A simple solution like applying a targeted nerve pain relief cream like Neuropasil can provide fast-acting comfort. This topical approach delivers relief directly to the source, helping you get back to the activities you love.
Immediate relief is just the first step. A comprehensive care plan—managing blood sugar, daily foot inspections, proper footwear, and knowing when to see a doctor—is your foundation for long-term foot health and complication prevention.
While it may seem like a lot, many people successfully manage their diabetic foot pain and live full lives. Every small step you take toward better foot care makes a difference.
The key is to start today. Progress begins with action, whether it's applying a soothing cream, scheduling a podiatrist visit, or simply inspecting your feet.
Your feet carry you through life; don't let diabetic foot pain dictate your future.
Find fast-acting relief with Neuropasil Nerve Pain Relief Cream today, or explore our full range of solutions at Neuropasil.com and our blog for more insights at Neuropasil Blog.














