Understanding Diabetic Nerve Pain: What You Need to Know
Diabetic nerve pain affects nearly half of all people with diabetes, making it one of the most common and challenging complications of the disease. This condition, medically known as diabetic neuropathy, occurs when high blood sugar levels damage nerves throughout your body over time.
Quick Facts About Diabetic Nerve Pain:
- What it is: Nerve damage caused by prolonged high blood sugar levels
- Who it affects: Up to 50% of people with diabetes develop some form of neuropathy
- Common symptoms: Tingling, burning, sharp pain, numbness, or weakness
- Most affected areas: Feet and legs first, then hands and arms
- Pain intensity: Ranges from mild discomfort to severe, disabling pain
- When it occurs: Often worse at night and can disrupt sleep
The pain can feel like burning, electric shocks, or stabbing sensations. Some people describe it as "pins and needles" that never go away, while others experience numbness that makes it hard to feel cuts or injuries.
The good news? While diabetic nerve pain can be serious, it's often preventable and manageable. With proper blood sugar control, lifestyle changes, and the right treatment approach, you can slow progression and find meaningful relief.
Understanding your condition is the first step toward taking control. The more you know about how diabetes affects your nerves, the better equipped you'll be to protect yourself and manage any symptoms that develop.
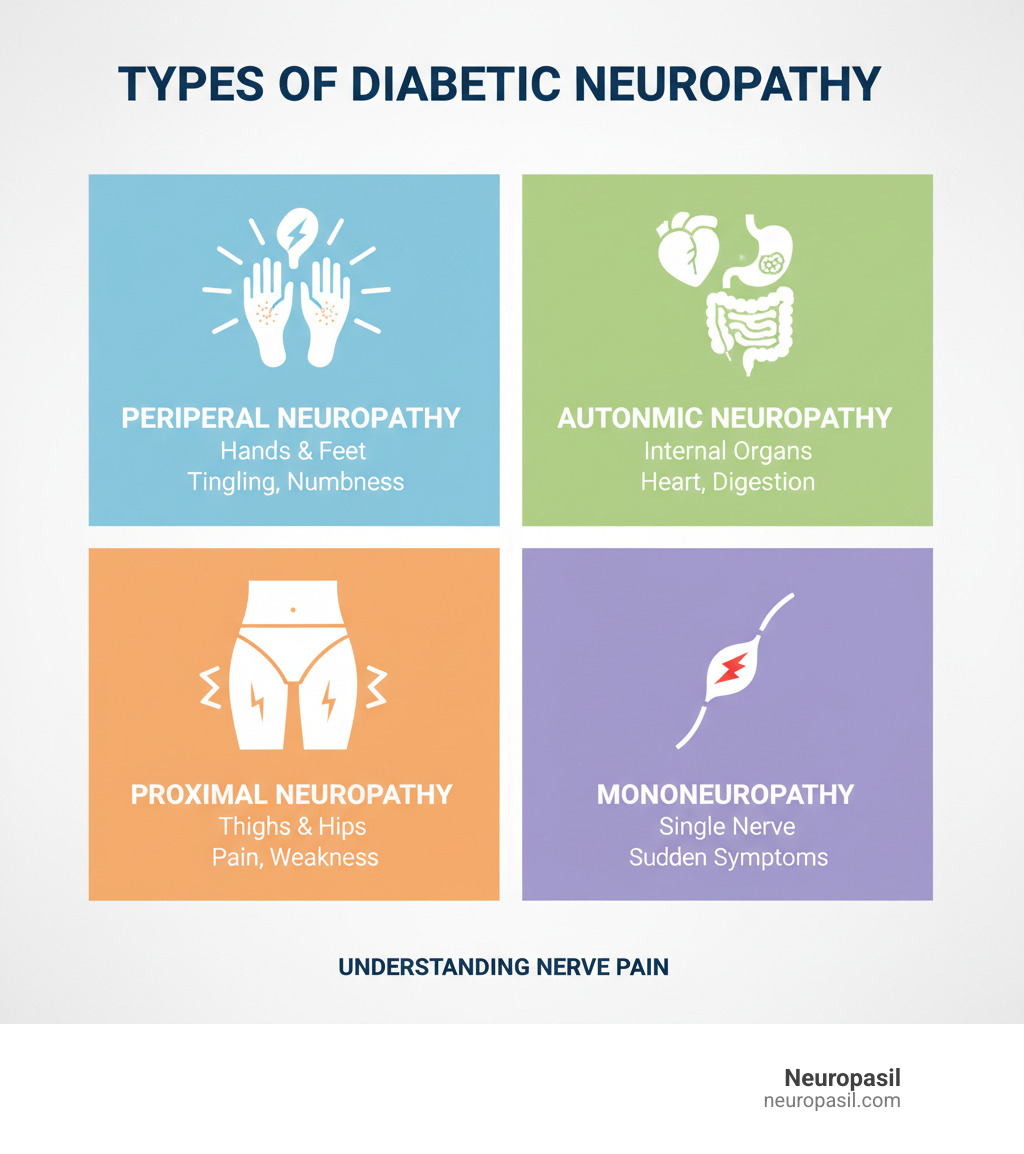
Understanding Diabetic Neuropathy: Types and Symptoms
Diabetic nerve damage, or diabetic nerve pain, is an umbrella term for several conditions. The common cause is prolonged high blood sugar, which damages nerves and the tiny blood vessels that nourish them. Up to 50% of people with diabetes develop some form of nerve damage, with symptoms ranging from subtle to severe burning pain, often at night.
Let's break down the four main types of diabetic neuropathy.
Peripheral Neuropathy
This is the most common type, affecting the feet and legs first, then often the hands and arms. Symptoms typically start in the toes and include tingling (pins and needles), numbness, burning sensations, or sharp pains, which are often worse at night.
This numbness can be dangerous, as it may hide a small cut or blister, leading to serious infections. It can also cause a loss of balance or a weakened grip. The pain from peripheral neuropathy affects 10% to 26% of people with diabetes, significantly impacting daily life. You can learn more about recognizing these early warning signs on our Peripheral Neuropathy Symptoms page.
Autonomic Neuropathy
This type damages the nerves controlling your automatic body functions, like heart rate, blood pressure, and digestion. It can cause dizziness upon standing, nausea, bloating, or issues with bladder control and sexual function.
A serious effect is the loss of warning signs for low blood sugar (hypoglycemia), as the body's normal response (shakiness, sweating) is silenced. Your sweat glands may also function abnormally, affecting temperature regulation. Over 30% of people with diabetes experience some form of autonomic neuropathy.
Proximal Neuropathy (Diabetic Amyotrophy)
More common in older adults with Type 2 diabetes, this type affects the thighs, hips, buttocks, or legs, usually on one side of the body. It can cause sudden, severe pain and weakness, making it difficult to stand from a sitting position. While it often improves over time, recovery can take months.
Mononeuropathy (Focal Neuropathy)
This is damage to a single specific nerve in the face, torso, or leg. It has a sudden onset and can cause conditions like Bell's palsy (facial weakness) or carpal tunnel syndrome. Though alarming, mononeuropathy often resolves on its own over weeks or months.
Catching any type of diabetic neuropathy early is key. Prompt recognition and blood sugar management improve your chances of slowing the damage and finding relief.
The Root Causes and Risk Factors of Nerve Damage
If you're dealing with diabetic nerve pain, understanding the cause is the first step toward management and prevention. The primary villain is high blood sugar (hyperglycemia), but it often works with other factors to damage your nerves.

The Role of High Blood Sugar
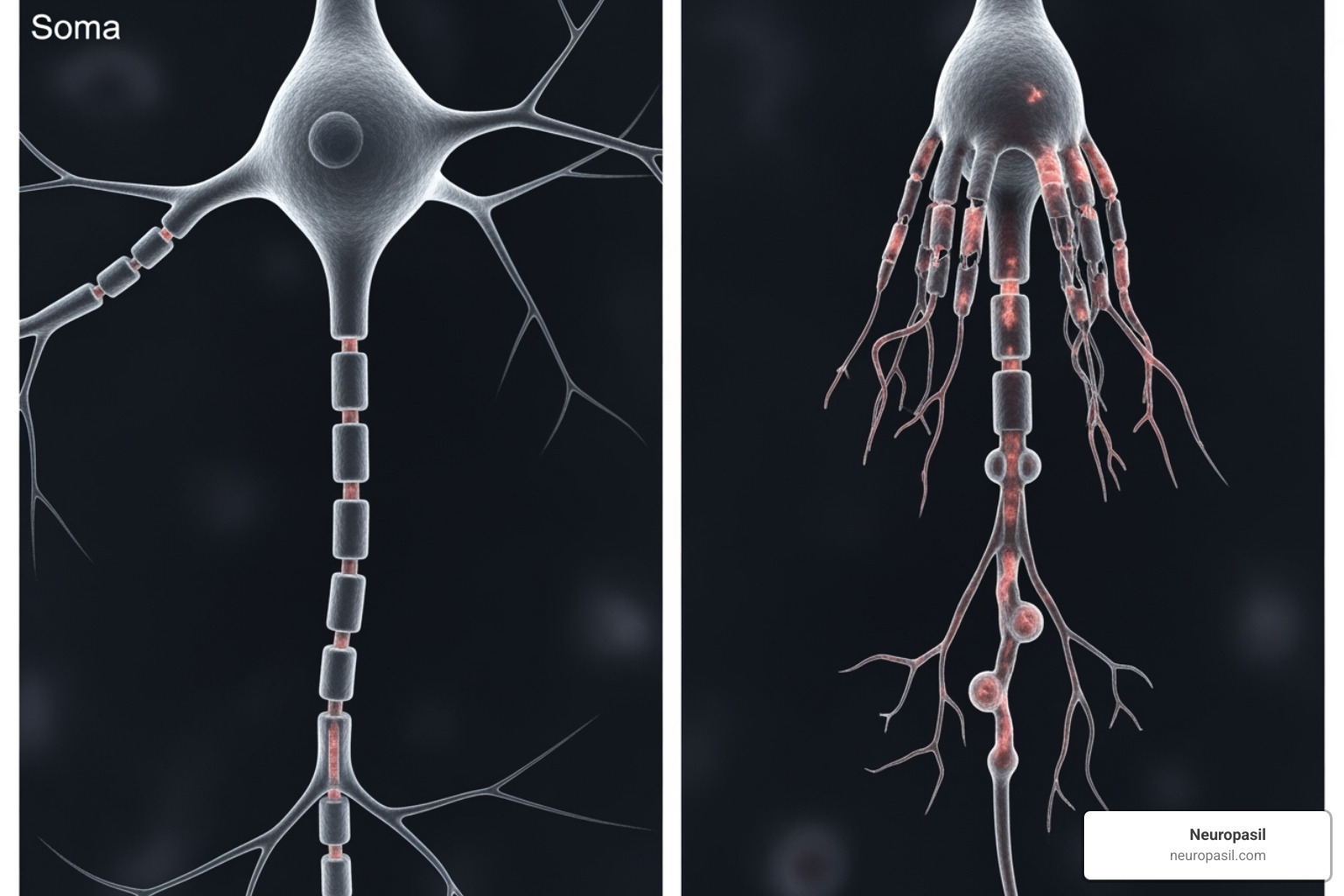
Excess sugar in your blood slowly damages nerves in two ways. First, it directly injures the nerve fibers. Second, it harms the tiny blood vessels (capillaries) that supply nerves with oxygen and nutrients, effectively starving them.
High glucose levels also trigger harmful chemical pathways. One process creates toxic substances like sorbitol that build up in nerves. Another produces free radicals that attack nerve cells. Furthermore, sugar can attach to proteins to form Advanced Glycation End Products (AGEs). These AGEs cause inflammation and make blood vessels stiff, worsening nerve damage.
Research shows that if your A1C levels remain above 7% for three or more years, your risk of neuropathy increases significantly. The scientific research on A1C levels and neuropathy risk highlights the importance of good blood sugar control. The duration of diabetes also matters; the longer you've had it, especially with poor control, the higher the risk.
Other Contributing Risk Factors
While high blood sugar is the main culprit, several other factors accelerate nerve damage:
- High blood pressure further damages the small blood vessels that feed your nerves, restricting blood flow.
- High cholesterol can clog blood vessels with fatty deposits, creating more roadblocks for blood trying to reach your nerves.
- Obesity contributes to chronic inflammation and insulin resistance, making blood sugar control more difficult.
- Kidney disease allows toxins to build up in the blood, which can poison nerves over time.
- Smoking is especially harmful, as it constricts blood vessels and severely limits the blood supply to already-damaged nerves. Quitting is one of the best things you can do for your nerve health. You can find helpful resources about quitting smoking.
- Alcohol use can cause nerve damage on its own (alcoholic neuropathy). Combining it with diabetes significantly increases the risk.
- Age and a family history of neuropathy are risk factors you cannot control but are important to be aware of.
Many of these risk factors are manageable. Every positive change you make—from better blood sugar control to lower blood pressure—helps protect your nerves and can slow down existing damage.
How Neuropathy is Diagnosed and Its Potential Complications
Early diagnosis of diabetic nerve pain is a game-changer. It allows you to slow the condition's progression and prevent serious problems. Since symptoms often develop gradually, regular screening is essential—annually after a Type 2 diabetes diagnosis, or five years after a Type 1 diagnosis.

Diagnostic Tests and Procedures
A diagnosis begins with a discussion of your symptoms, such as tingling, numbness, or pain. A physical exam will follow, where your doctor checks your reflexes, muscle strength, and ability to feel light touch, temperature, and vibration.
A comprehensive foot exam is critical, as this is where problems often start. Your doctor will look for cuts, sores, and other abnormalities. Key diagnostic tests include:
- Monofilament test: A soft nylon thread is pressed against your foot to check for loss of protective sensation.
- Nerve conduction studies: These measure the speed of electrical signals in your nerves.
- Electromyography (EMG): This test measures how your muscles respond to nerve signals.
- Quantitative sensory testing: This checks your ability to feel vibrations and temperature changes.
- Autonomic function tests: These evaluate how well automatic body functions, like heart rate and blood pressure, are working.
The Dangers of Ignoring Symptoms
Ignoring diabetic nerve pain can lead to severe, life-altering complications. Fortunately, most are preventable with proper care.
- Foot ulcers and infections: Numbness can cause small cuts or blisters to go unnoticed. Due to slower healing, these minor injuries can become serious infections.
- Amputation: If a foot infection becomes severe and leads to gangrene, amputation may be necessary to save a person's life. This devastating outcome is almost always preventable with regular foot care.
- Charcot foot: In this condition, bones in the foot weaken and break without any pain sensation. Continued walking on the injured foot leads to severe deformity.
- Falls and mobility issues: Weakness and numbness in the legs and feet can impair balance, increasing the risk of falls and fractures.
- Chronic pain: The constant burning and shooting pains can severely impact sleep, mood, and overall quality of life.
- Autonomic neuropathy risks: This can affect heart rhythm, blood pressure, and digestion, and may even mask the warning signs of life-threatening low blood sugar.
Early detection and proactive management are your best defense against these complications. If you experience any signs of diabetic nerve pain, speak with your healthcare team.
A Comprehensive Guide to Managing Diabetic Nerve Pain
Living with diabetic nerve pain doesn't mean you are powerless. While there is no cure, combining medical treatments and lifestyle changes can significantly improve your quality of life. Effective management works on two fronts: relieving current symptoms and slowing down further nerve damage.
| Medical Treatments | Lifestyle Changes |
|---|---|
| Oral Medications: Anticonvulsants, Antidepressants, Opioids (second/third line) | Blood Sugar Control: Maintain A1C below 7% |
| Topical Treatments: Capsaicin cream, Lidocaine patches | Diet: Healthy, balanced meal plan |
| Other Agents: Alpha-lipoic acid, Vasodilators | Exercise: Regular, low-impact activity |
| Physical Therapy: Strength, balance, flexibility | Foot Care: Daily checks, proper hygiene, appropriate footwear |
| Alternative Therapies: Acupuncture, TENS units | Avoidance: Quit smoking, limit alcohol |
| Mental Health: Stress management, support groups |
Prevention: The First Line of Defense
The best treatment is prevention. This centers on strict blood sugar management, aiming for an A1C below 7% for most adults. Regular checkups, including annual comprehensive foot exams, serve as an early warning system. Daily foot care is also essential: inspect your feet for any cuts or blisters, wash and dry them thoroughly, and always wear clean socks with well-fitting, closed-toe shoes.
Medical Treatments for Diabetic Nerve Pain
When pain becomes a daily issue, medical treatments can offer relief. The goal is to reduce pain to a manageable level.
Oral Medications: Anticonvulsants like pregabalin (Lyrica) and gabapentin (Neurontin) work by calming overexcited nerves. Antidepressants such as duloxetine (Cymbalta) and amitriptyline are also highly effective for nerve pain, even in people who are not depressed. Duloxetine is FDA-approved specifically for diabetic nerve pain. Opioids like tramadol or tapentadol may be prescribed for severe pain when other treatments fail, but they are used cautiously due to addiction risks.
Topical Treatments: Capsaicin cream (from chili peppers) and lidocaine patches can provide targeted relief to a specific area without systemic side effects.
Other Treatments: Alpha-lipoic acid, an antioxidant, may help with nerve repair. Physical therapy can improve strength and balance, while TENS units use mild electrical currents to reduce pain signals.
Finding the right treatment can take time, as you may need to try different medications or combinations. It often takes several weeks to determine if a treatment is effective.
Lifestyle Changes for Easing Diabetic Nerve Pain
Lifestyle changes are powerful tools that create an environment for your nerves to thrive.
- Diet: A balanced diet provides essential nutrients, like B vitamins, that support nerve function.
- Exercise: Gentle, low-impact activities like walking, swimming, or yoga improve circulation to damaged nerves and release natural pain-relieving endorphins.
- Stress Management: Techniques like meditation and deep breathing can reduce stress, which often worsens pain perception and affects blood sugar.
- Avoid Harmful Habits: Quitting smoking and avoiding alcohol are critical steps. Smoking restricts blood flow, while alcohol is directly toxic to nerves.
By combining medical treatments with these daily habits, you give yourself the best chance to reduce pain and prevent complications.
Frequently Asked Questions about Diabetic Nerve Pain
When you're dealing with diabetic nerve pain, it's natural to have questions. Here are clear, honest answers to some of the most common concerns.
Can diabetic nerve damage be reversed?
The potential for reversal depends on the severity of the damage. In the early stages, some people see symptoms like numbness and tingling improve or even disappear within a year of achieving strict blood sugar control. For long-standing, severe neuropathy, complete reversal is less likely.
However, it is always possible to slow the progression of damage and manage symptoms effectively. Your nerves have some capacity to regenerate, and excellent blood sugar control provides the best environment for this. The key is to focus on what you can control: your blood sugar, lifestyle, and treatment plan.
What does diabetic nerve pain feel like?
Diabetic nerve pain is different for everyone, but there are common patterns. Symptoms often worsen at night and can disrupt sleep. The most frequent sensations include:
- A burning feeling, often described as feet being too close to a fire, that usually starts in the toes.
- Tingling or "pins and needles," similar to a limb "falling asleep" but not waking up.
- Sharp, stabbing, or electric-like pains that can shoot through the feet or hands without warning.
- Numbness, which is dangerous because it can hide injuries like cuts or blisters.
- Extreme sensitivity (allodynia), where a light touch from something like bedsheets can feel excruciating.
When should I see a doctor about nerve pain?
You should see a doctor promptly, as diabetic nerve pain typically gets worse, not better, without treatment. Don't wait for symptoms to become severe. Seek medical advice for any of the following:
- Any new or persistent tingling, numbness, or pain, especially in your feet and hands.
- Burning or shooting pains that interfere with your sleep or daily activities.
- Any sores, cuts, blisters, or infections on your feet, particularly if you didn't feel the initial injury.
- Symptoms of autonomic neuropathy, such as dizziness when standing, digestive problems, or changes in bladder control.
Even without symptoms, annual foot exams are essential for everyone with diabetes to catch problems early.
Conclusion: Taking Control of Your Nerve Health
Living with diabetic nerve pain doesn't have to mean accepting a life of discomfort and limitations. Throughout this guide, we've explored the complex world of diabetic neuropathy—from understanding the different types and their unique symptoms to finding the root causes that damage our precious nerve pathways. Most importantly, we've outlined a clear roadmap for taking charge of your nerve health.
The evidence is overwhelming: proactive management works. While we can't promise a complete cure, the combination of tight blood sugar control, thoughtful lifestyle choices, regular medical care, and targeted treatments can dramatically improve your daily experience. Think of it as building a protective shield around your nerves—every healthy choice you make strengthens that defense.
Your daily actions matter more than you might realize. That consistent blood sugar monitoring, the daily foot inspection that takes just two minutes, the evening walk around the block, and even choosing water over that sugary drink—these seemingly small decisions compound into powerful protection against nerve damage progression.
You're not alone in this journey. Your healthcare team is your ally, ready to help you steer treatment options and adjust your care plan as needed. Don't hesitate to speak up about new symptoms, ask questions about your medications, or request referrals to specialists when you need them. Being your own advocate is one of the most important skills you can develop.
The path forward requires patience and persistence. Some treatments take weeks to show their full benefit, and finding the right combination of approaches often involves some trial and adjustment. But with each step you take toward better nerve health, you're investing in more comfortable days, better sleep, and the freedom to enjoy the activities that matter most to you.
At Neuropasil, we understand the daily challenges of managing nerve discomfort, and we're committed to supporting your journey with natural solutions that complement your comprehensive care plan. When you're ready to explore how targeted nutritional support might improve your nerve health strategy, we're here to help you take that next step toward greater comfort and wellbeing.














