Why Aching Legs After Walking Doesn't Have to Be Your Reality
Aching legs after walking is one of the most common complaints among active adults and athletes—but it doesn't have to stop you from enjoying the simple pleasure of a daily walk. Whether it's a dull throb, sharp pain, or lingering cramps, understanding why your legs hurt is the first step toward finding real relief.
Quick Answer: What Causes Aching Legs After Walking?
| Cause | What It Is | Key Symptom |
|---|---|---|
| Muscle Soreness (DOMS) | Small tears in muscle fibers from overuse | Stiffness, tenderness 12-24 hours later |
| Walking Injuries | Hamstring strain, IT band syndrome, Achilles pain | Sharp or shooting pain in specific areas |
| Joint Pain | Arthritis or inflammation in knees, hips, ankles | Stiffness, swelling, difficulty moving |
| Claudication (PAD) | Poor blood flow to leg muscles | Cramping during activity, relief with rest |
| Nerve Issues | Sciatica, spinal stenosis, neuropathy | Radiating pain, numbness, tingling |
The good news? Most leg pain after walking is completely preventable with the right approach. Sometimes it's as simple as warming up properly or investing in better shoes. Other times, it signals something deeper—like poor circulation or nerve compression—that needs medical attention.
I'm Tony Enrico, and I created Neuropasil after witnessing too many people give up on activities they love because of persistent pain, including aching legs after walking. Through research and real-world testing, I've helped thousands reclaim their mobility with fast-acting, natural relief that works.
This guide will walk you through the most common causes of leg pain after walking, when to worry (and when not to), and proven strategies to prevent and relieve discomfort—so you can keep moving without fear.
Aching legs after walking terms simplified:
- lactic acid in legs
- calf muscles hurt
- muscle ache remedy.
What is Delayed Onset Muscle Soreness (DOMS)? DOMS is the familiar muscle pain, stiffness, and tenderness that develops 12 to 24 hours after an unfamiliar or intense physical activity. It's not a sign of injury in the serious sense, but rather an indication that your muscles have been challenged in a new way. When you engage muscles more than usual, tiny, microscopic tears occur in the muscle fibers. As your body repairs these micro-tears, it leads to inflammation and discomfort, which we perceive as soreness. Think of it as your muscles getting stronger and adapting to the new demands.
The American College of Sports Medicine notes that DOMS develops 12-24 hours after a walk that places unusual stress on your muscles, like picking up your speed or walking downhill. In severe cases, you might also experience leg swelling and joint stiffness. While uncomfortable, DOMS is a normal part of the muscle adaptation process. For more on how to recover, check out our Leg DOMS Recovery Survival Guide.
Common Walking Injuries and Tendon Pain
While DOMS is usually benign, aching legs after walking can also stem from more specific injuries, particularly those affecting our tendons. These conditions often arise from overuse, improper form, or insufficient preparation.
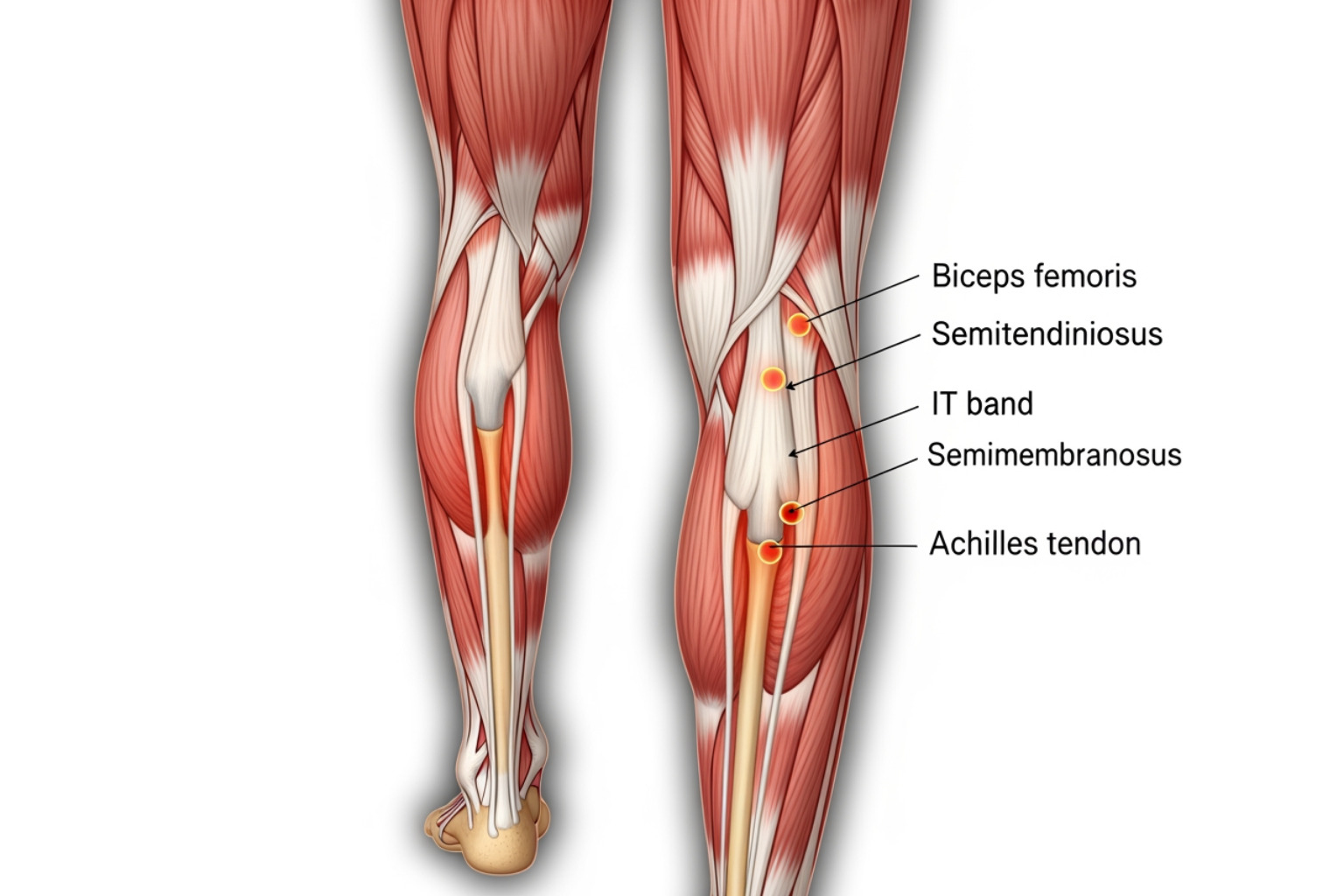
- Hamstring Strain: The hamstrings are a group of three muscles at the back of your thigh. A strain occurs when these muscles are overstretched or torn, often due to sudden movements, insufficient warm-up, or muscle imbalance. You might feel pain behind the thigh or knee, especially during or after walking, along with stiffness. The best way to treat sore hamstrings is with RICE (Rest, Ice, Compression, and Elevation) and gentle stretching once the muscles are warm.
- IT Band Syndrome: The iliotibial (IT) band is a thick band of connective tissue running along the outside of your thigh from your hip to your knee. When it becomes tight or inflamed, it can cause pain on the outside of the knee, often described as clicking or popping. Long-distance walking, especially on sloped roads, can aggravate the IT band. To prevent further injury, stretching all leg muscles (hamstrings, quads, calves, hip flexors) after warming up is crucial, along with foam rolling the IT band.
- Achilles Tendonitis: The Achilles tendon connects your calf muscles to your heel bone. Inflammation of this tendon, known as Achilles tendonitis, typically causes pain and tenderness at the back of the heel, especially after increased walking frequency or distance. Rest, ice, elevation, and anti-inflammatories can help ease the pain. Proper warm-up and stretching, including a wall stretch for the Achilles tendon, are recommended for prevention.
- Plantar Fasciitis: This condition affects the plantar fascia, a thick band of tissue running along the bottom of your foot, connecting your heel to your toes. It causes sharp, stabbing pain in the heel, especially with the first steps in the morning or after prolonged walking.
- Shin Splints: Medial tibial stress syndrome, commonly known as shin splints, causes pain along the inner edge of the shin bone. It's often an overuse injury that occurs when the muscles, tendons, and bone tissue around the shin become inflamed due to increased activity, poor footwear, or walking on hard surfaces.
For more detailed guidance on how to manage these common walking-related pains, Virtua Health offers excellent advice on how to treat common walking injuries.
The Role of Joint and Foot Pain
Beyond muscle and tendon issues, our joints and feet play a significant role in how our legs feel after walking. Conditions like arthritis or biomechanical issues in the feet can turn a pleasant stroll into a painful ordeal.
Arthritis Impact Joint pain, particularly from arthritis, can be a major contributor to aching legs after walking. Arthritis, especially osteoarthritis, involves the breakdown of cartilage cushioning our joints. Walking, while beneficial, places a small but constant amount of stress on weight-bearing joints like the knees, hips, and ankles. For those with arthritis, this stress can worsen inflammation and stiffness, leading to pain after activity. The Arthritis Foundation provides comprehensive information on osteoarthritis. Managing arthritis often involves a balance of activity and rest, along with strategies to reduce joint stress.
Foot Mechanics Our feet are the foundation of our body, and any issues here can ripple up to cause leg pain.
- Flat Feet (Pes Planus): When the arches of your feet collapse, it can alter your gait and put extra strain on your ankles, shins, and knees, leading to aching.
- High Arches (Pes Cavus): Conversely, unusually high arches can lead to insufficient shock absorption, concentrating impact forces on specific areas of the foot and leg.
- Unsupportive Footwear: Wearing shoes that lack proper cushioning or arch support can intensify discomfort, especially when walking on hard surfaces like pavement. This is particularly relevant in urban environments like New York City, where concrete sidewalks are the norm. Ill-fitting shoes can also contribute to a host of problems, including plantar fasciitis and bunions, which can alter your walking mechanics and cause secondary leg pain.
Addressing joint and foot pain often requires a multifaceted approach, including appropriate footwear, orthotics, and targeted exercises. For broader strategies on managing leg discomfort, explore our article on Easing Aches: Simple Solutions for Leg Pain Relief.
When Leg Pain Signals a Deeper Medical Issue
While many instances of aching legs after walking are benign and related to muscle fatigue or minor injuries, sometimes pain can be a red flag for more serious underlying medical conditions. It’s crucial to distinguish between simple aches and symptoms that warrant professional medical attention.
Vascular Problems: Claudication, PAD, and DVT
Problems with blood flow are a significant cause of leg pain that often manifests during or after walking.
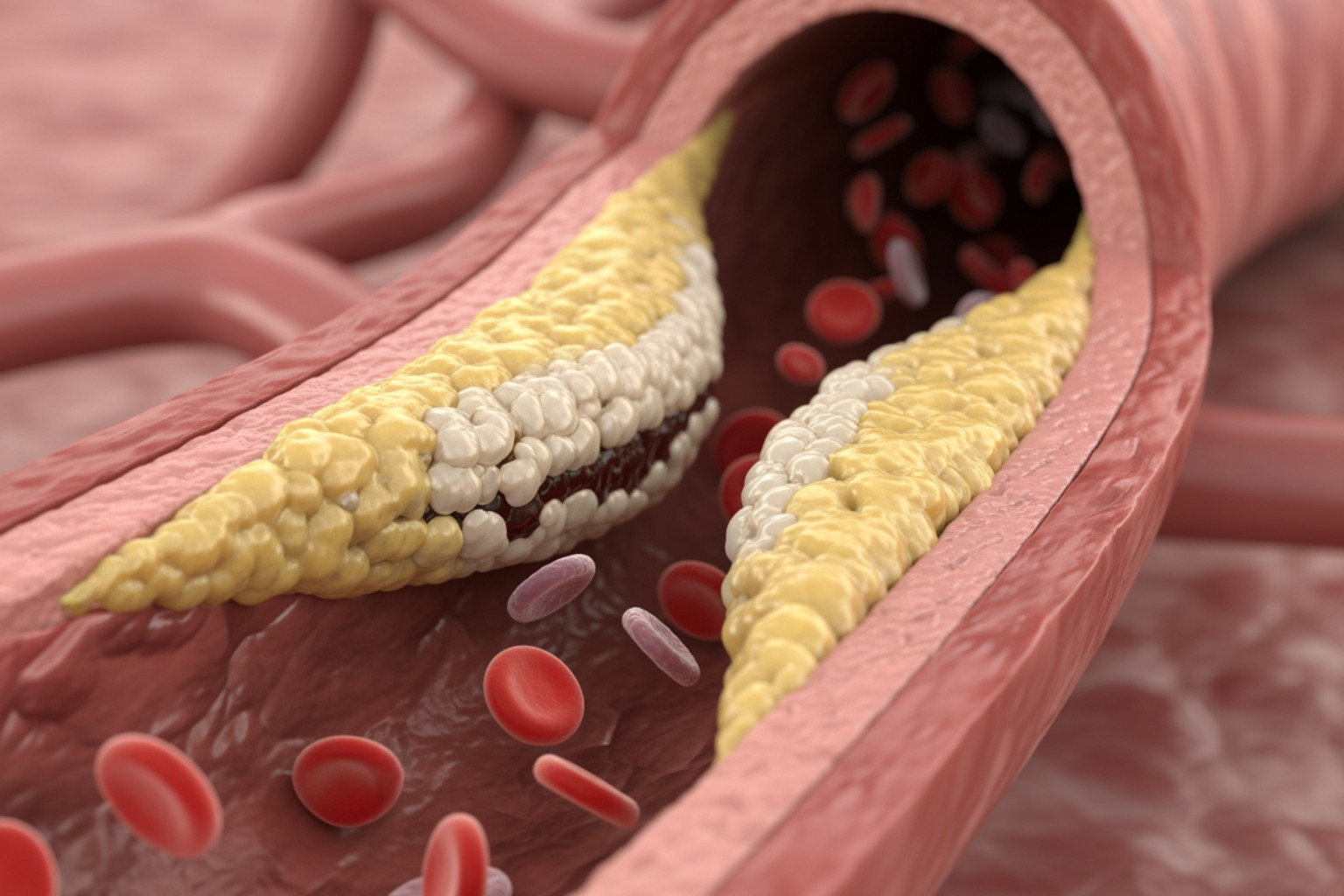
Claudication and Peripheral Artery Disease (PAD) Claudication is leg pain caused by insufficient blood flow to muscles during exercise. It's often a cramp, ache, or fatigue in the calves, thighs, or hips that occurs after walking a certain distance and time. The hallmark of claudication is that the pain eases relatively quickly with rest, only to return when activity resumes. This "walk-rest-walk" pattern is a strong indicator of Peripheral Artery Disease (PAD).
PAD is a condition where the arteries that supply blood to your limbs, most commonly your legs, become narrowed. This narrowing is usually due to atherosclerosis—the buildup of plaque (fats, cholesterol, and other substances) on the artery walls. When the arteries narrow, your leg muscles don't receive enough oxygenated blood to meet the demands of exercise, leading to pain. The Cleveland Clinic provides a comprehensive overview of claudication symptoms and causes.
People with PAD are six to seven times more likely to have a heart attack, stroke, or transient ischemic attack than people without it. This statistic from Harvard Health underscores the seriousness of PAD; persistent leg pain, even if it eases with rest, should never be ignored. Regular exercise, a healthy diet, managing blood sugar, cholesterol, and blood pressure, and quitting smoking are key preventive measures.
Deep Vein Thrombosis (DVT) Another serious vascular condition is Deep Vein Thrombosis (DVT), which involves a blood clot forming in a deep vein, usually in the leg. Unlike claudication, DVT pain is often constant and not necessarily triggered by activity. Signs of DVT can include:
- Swelling in one leg (rarely both)
- Pain or tenderness in the leg, often starting in the calf
- Warmth in the affected leg
- Redness or discoloration of the skin
DVT is a medical emergency because the clot can break loose and travel to the lungs, causing a pulmonary embolism. If you experience these symptoms, especially after prolonged inactivity (like a long flight or bed rest), seek emergency medical care immediately.
Nerve-Related Pain: Sciatica, Spinal Stenosis, and Neuropathy
Nerve issues can also cause aching legs after walking, often presenting with distinct symptoms like radiating pain, numbness, or tingling.
Pinched Nerves and Sciatica A pinched nerve occurs when too much pressure is applied to a nerve by surrounding tissues, such as bones, cartilage, muscles, or tendons. In the legs, a common example is sciatica. Sciatica refers to pain that radiates along the path of the sciatic nerve, which branches from your lower back through your hips and buttocks and down each leg. It typically affects only one side of your body. Symptoms can include:
- Sharp, shooting pain down the leg
- Numbness or tingling (often described as "pins and needles")
- Muscle weakness in the affected leg or foot
- Pain that worsens with prolonged sitting or certain movements, and can sometimes be aggravated by walking.
Lumbar Spinal Stenosis Lumbar spinal stenosis is a narrowing of the spinal canal in the lower back, which can put pressure on the spinal cord and nerve roots. This compression can lead to leg pain, numbness, tingling, or weakness, especially when walking or standing for extended periods. A classic symptom is that the pain is often relieved by leaning forward (like pushing a shopping cart) or sitting down. Diagnosis typically involves symptom assessment and imaging tests like MRI or CT scans. Treatment can range from physical therapy and pain relievers to injections or, in severe cases, surgery.
Diabetic Neuropathy Diabetic neuropathy is a type of nerve damage that can occur if you have diabetes. High blood sugar levels can injure nerve fibers throughout your body, but diabetic neuropathy most often damages nerves in your legs and feet. Symptoms can include:
- Numbness or reduced ability to feel pain or temperature changes
- Tingling or burning sensations
- Sharp pains or cramps
- Increased sensitivity to touch
- Muscle weakness
- Loss of reflexes
Managing blood sugar levels is paramount for preventing and slowing the progression of diabetic neuropathy. Treatments can include pain relievers, antidepressants, or anticonvulsants to help manage the nerve pain. For a deeper dive into nerve-related leg pain, refer to our Complete Guide to Leg Nerve Pain Causes Relief.
Your Action Plan for Relief and Prevention
Now that we've explored the various causes of aching legs after walking, let's shift our focus to proactive strategies. Our goal is to combine immediate relief techniques with long-term prevention methods, ensuring you can enjoy your walks without discomfort.
At-Home Remedies for Aching Legs After Walking
When your legs are tired or sore from a walk, these home remedies can provide comfort and promote recovery.
- Rest and Recovery: This is often the most straightforward and effective remedy. Give your legs the break they deserve. For DOMS, a day or two of reduced activity can make a huge difference.
-
RICE Method: For acute soreness or minor strains, the RICE protocol (Rest, Ice, Compression, Elevation) is your best friend.
- Rest: Avoid activities that aggravate the pain.
- Ice: Apply a cold compress to the affected area for 15-20 minutes several times a day to reduce inflammation and soreness.
- Compression: Use an elastic bandage to gently compress the area, which can help reduce swelling.
- Elevation: Raise your legs above your heart to further reduce swelling.
- Gentle Stretching and Foam Rolling: Once the initial acute pain subsides, gentle stretching can improve flexibility and blood flow, while foam rolling can help release tight muscles and fascia.
- Hydration: We can't stress this enough! Dehydration can lead to muscle cramps and fatigue. Make sure you're drinking enough water before, during, and after your walks.
- Proper Nutrition for Muscle Repair: Fuel your body with adequate protein to support muscle repair and recovery. A balanced diet rich in vitamins and minerals (especially magnesium, potassium, and calcium) is essential for muscle function.
For more detailed strategies on how to bounce back quickly, read our guide on How to Relieve Sore Legs and Recover Quickly.
Proactive Prevention: The Keys to Pain-Free Walks
Preventing aching legs after walking is always better than treating them. Incorporating these practices into your routine can make a significant difference.
- Proper Warm-Up Routines: Never skip your warm-up! A 5-10 minute warm-up, including light cardio and dynamic stretches, prepares your muscles for activity, increases blood flow, and reduces the risk of injury. This could be a brisk walk, arm circles, leg swings, or torso twists.
-
Building Strength and Flexibility: Strong, flexible muscles are less prone to injury and fatigue. Incorporate a balanced exercise routine that includes:
- Calf Raises: Strengthens calf muscles and Achilles tendon.
- Squats: Works glutes, quads, and hamstrings.
- Lunges: Improves strength and balance in each leg individually.
- Glute Bridges: Strengthens glutes and hamstrings, crucial for hip stability.
- Hamstring Curls: Directly targets hamstring strength.
- Stretching: Focus on hamstrings, quadriceps, calves, and hip flexors after your walk to maintain flexibility.
-
Importance of Supportive Footwear: Your shoes are your most important piece of walking equipment.
- Choosing the Right Shoes: Invest in properly fitted, supportive, and cushioned footwear. Look for shoes that match your foot type and gait. Replace your walking shoes every 6 months or 300-400 miles, as their cushioning and support degrade over time (source).
- Considering Orthotics: If you have specific foot mechanics issues like flat feet or high arches, custom or over-the-counter orthotics can provide additional support and correct biomechanical imbalances.
- Gradual Progression: Avoid the "too much, too soon" trap. Gradually increase your walking distance, duration, or intensity by no more than 10% per week. This allows your body time to adapt and strengthen without excessive strain. Listen to your body and incorporate rest days, especially when starting a new routine or increasing your activity level.
Finding Fast, Soothing Relief with Neuropasil Cream
Despite our best preventive efforts, sometimes aching legs after walking still creep in. That's where targeted, fast-acting relief becomes invaluable. At Neuropasil, we understand the frustration of persistent pain and have developed a targeted solution.
How Neuropasil's Nerve and Muscle Pain Relief Cream Works Neuropasil offers natural, fast-acting topical creams for nerve pain and sore muscles. Our unique formula is powered by key natural ingredients:
- Menthol: Provides a cooling sensation that distracts from pain and helps to relax muscles.
- Aloe: Known for its soothing and anti-inflammatory properties, it helps calm irritated skin and tissues.
- Urea: Improves the absorption of other ingredients, allowing them to penetrate deeper for more effective relief.
This powerful combination works together to provide targeted, soothing relief for various types of pain. Many of our loyal customers, from active individuals to athletes, testify to using Neuropasil for neuropathy, sciatica, plantar fasciitis, strains, sprains, general aches and pains, and joint discomfort. It’s perfect for those moments when your muscles are sore and your nerves are screaming for a break.
Our fast-acting, all-natural formula provides relief that helps you get back to your routine quickly. For those seeking immediate comfort for sore muscles and nerve discomfort, topical creams offer a convenient and effective solution. Find how Neuropasil can be your ally against aching legs after walking by exploring our guide to the best pain-relieving creams. Ready to experience the difference? Discover Neuropasil's All-Natural Relief Cream today.
When to Seek Professional Medical Advice
While many aches can be managed at home, some symptoms require professional medical advice. Ignoring red flags can delay diagnosis of a serious underlying problem.
You should consider consulting a healthcare professional if you experience any of the following:
- Severe or Persistent Pain: If your leg pain is intense, doesn't improve with rest and home care after a few days, or significantly interferes with your daily activities, it's time to see a doctor.
- Pain that Worsens Despite Home Care: If your pain continues to intensify even after applying RICE, stretching, and resting, it could indicate a more significant issue.
- Numbness or Weakness in the Legs: These symptoms, especially if accompanied by radiating pain, could point to nerve compression (like sciatica or spinal stenosis) that requires medical evaluation.
- Swelling, Redness, or Warmth in One Leg: These are classic signs of Deep Vein Thrombosis (DVT), a medical emergency (source). Seek immediate medical attention.
- Pain at Rest: If you experience leg pain even when you're not walking or exercising, particularly at night, it could be a sign of Peripheral Artery Disease (PAD) or other vascular issues.
- Changes in Skin Color or Temperature: Discoloration (paleness, blueness, or redness), coldness, or non-healing sores on your legs or feet are serious signs of poor circulation.
- Pain accompanied by Fever or Chills: This could indicate an infection.
Who to See:
- Primary Care Doctor: Your first point of contact for any persistent or concerning symptoms. They can diagnose common issues or refer you to a specialist.
- Sports Medicine Specialist: If your pain is clearly exercise-related and persistent, a sports medicine doctor can help diagnose and manage musculoskeletal injuries. You can schedule an appointment with a specialist if needed.
- Physical Therapist: For rehabilitation, strengthening, and correcting biomechanical issues contributing to your pain. They can create a personalized exercise program to address your specific needs.
- Vascular Specialist: If PAD or DVT is suspected, a vascular specialist can perform diagnostic tests and recommend appropriate treatment.
- Neurologist: For complex nerve-related pain, a neurologist can provide specialized diagnosis and management.
While some soreness after a long walk can be normal, persistent or severe leg pain shouldn’t be a regular part of your daily life. Listening to your body and knowing when to seek professional help is a vital part of maintaining your long-term health and mobility.
Frequently Asked Questions about Aching Legs After Walking
We get a lot of questions about this topic, so let's tackle some of the most common ones we hear.
Why do my legs ache after walking when I'm out of shape?
If you're new to walking, it's common to experience aching legs after walking due to Delayed Onset Muscle Soreness (DOMS). Unconditioned muscles develop microscopic tears from the new exertion. As your body repairs these tears, it causes inflammation, stiffness, and pain. Your muscles are essentially adapting and getting stronger. The key here is to start slowly and gradually increase your walking time and intensity. Don't try to go from zero to marathon in a week; your legs will thank you!
Can dehydration cause leg pain after walking?
Absolutely, yes! Dehydration is a significant cause of aching legs after walking. When you're dehydrated, your body's electrolyte balance (sodium, potassium, magnesium, calcium) can be thrown off. These electrolytes are crucial for proper muscle function, including contraction and relaxation. An imbalance can lead to muscle cramps, spasms, and fatigue (source). Without enough fluid, your muscles also become less efficient at flushing out metabolic waste products, which can contribute to soreness. It's crucial to stay well-hydrated throughout the day, especially before, during, and after your walk. Water is best, but for longer or more intense walks, an electrolyte-rich drink can be beneficial.
How long should I rest my aching legs after walking?
The duration of rest depends entirely on the cause and severity of your leg pain.
- For mild soreness (DOMS): A day or two of rest is usually sufficient. Light activity, such as gentle stretching, a very easy walk, or active recovery (like swimming), can actually help reduce soreness by increasing blood flow to the muscles.
- For more severe pain or a suspected injury: If you suspect a strain or sprain, it's best to rest for 24-48 hours and apply the RICE method (Rest, Ice, Compression, Elevation). Avoid putting weight on the affected leg if the pain is sharp.
- For persistent or worsening pain: If your pain doesn't improve after a few days of rest, or if it gets worse, it's a sign that you should seek medical advice. As we discussed, pain that signals deeper issues like DVT or PAD requires prompt professional attention. Always listen to your body; it's usually pretty good at telling you what it needs!
Conclusion
Aching legs after walking doesn't have to be your new normal. By understanding the common causes—from muscle soreness and minor injuries to more serious vascular and nerve conditions—you can take proactive steps to prevent and manage discomfort. Simple strategies like proper warm-ups, building strength, supportive footwear, and gradual progression can make a world of difference.
And for those times when your legs still demand attention, targeted solutions like Neuropasil's fast-acting, all-natural nerve and muscle pain relief cream can provide the soothing comfort you need to keep moving. Don't let leg pain hold you back from enjoying the many benefits of walking. Empower yourself with knowledge, listen to your body, and take control of your leg health so you can stride confidently through life!
Explore more resources on muscle and nerve health and find how we can help you stay active and pain-free.
References
- American College of Sports Medicine. (n.d.). Delayed Onset Muscle Soreness (DOMS). Retrieved from https://www.acsm.org/docs/default-source/files-for-resource-library/delayed-onset-muscle-soreness-(doms).pdf?sfvrsn=8f430e18_2
- Arthritis Foundation. (n.d.). Osteoarthritis. Retrieved from https://www.arthritis.org/diseases/osteoarthritis
- Centers for Disease Control and Prevention. (n.d.). Facts About Deep Vein Thrombosis. Retrieved from https://www.cdc.gov/ncbddd/dvt/facts.html
- Cleveland Clinic. (n.d.). Claudication. Retrieved from https://my.clevelandclinic.org/health/diseases/21972-claudication
- Cleveland Clinic. (n.d.). Dehydration and Exercise: Why Water Is So Important. Retrieved from https://health.clevelandclinic.org/dehydration-and-exercise-why-water-is-so-important
- Harvard Health Publishing. (2022). When walking makes your legs hurt. Retrieved from https://www.health.harvard.edu/pain/when-walking-makes-your-legs-hurt
- Hospital for Special Surgery. (n.d.). How to Choose the Right Walking Shoes. Retrieved from https://www.hss.edu/article_how-to-choose-walking-shoes.asp
- Mayo Clinic. (2023). Claudication - Symptoms & causes. Retrieved from https://www.mayoclinic.org/diseases-conditions/claudication/symptoms-causes/syc-20370952
- Virtua Health. (n.d.). Why Your Daily Walk May Be Making You Really Sore. Retrieved from https://www.virtua.org/articles/why-your-daily-walk-may-be-making-you-really-sore














