Understanding the Electric Storm: Why Nerve Pain in Your Leg Feels So Different
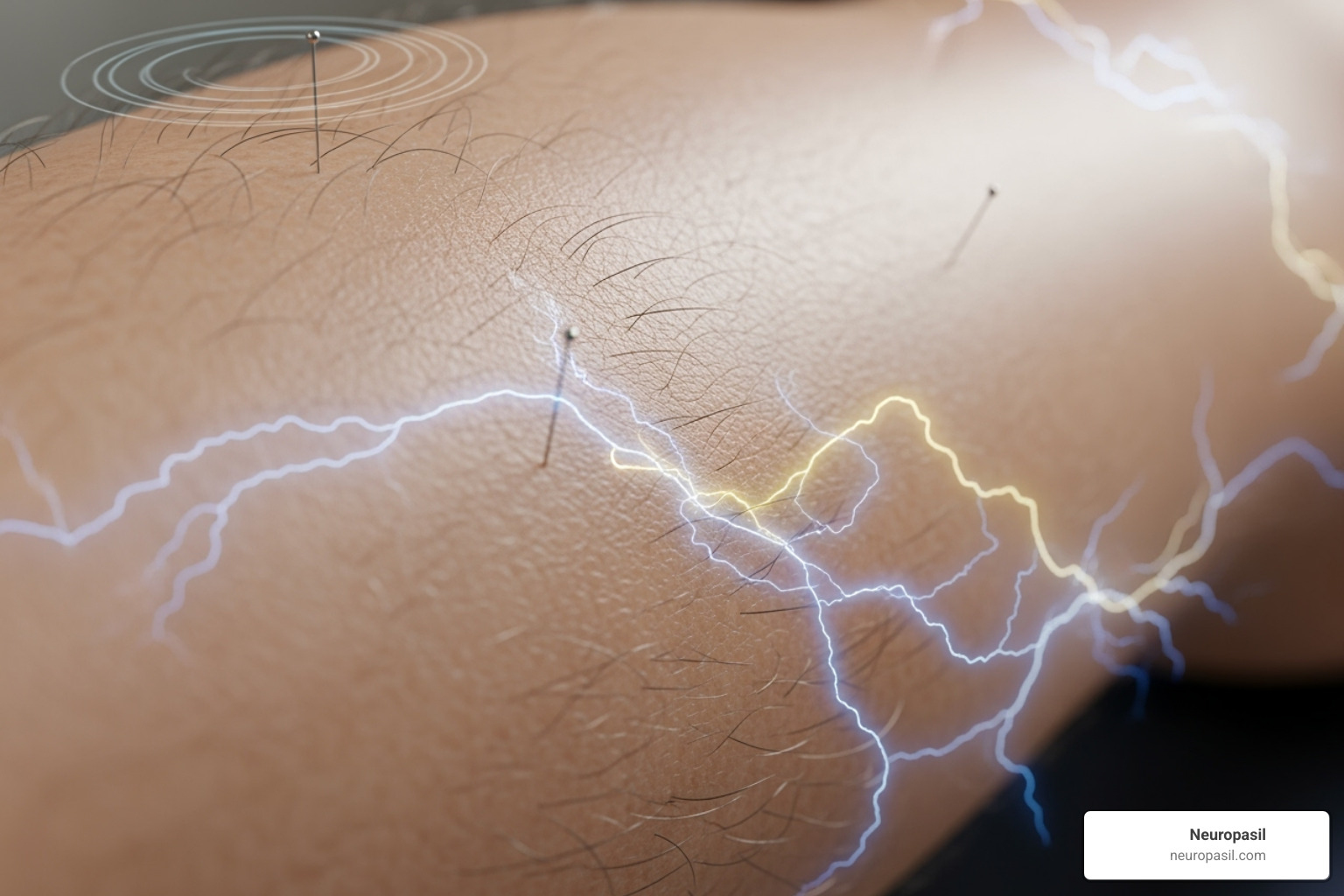
Answering what does nerve pain feel like in leg can be confusing. Unlike a familiar muscle ache, nerve pain brings strange sensations that feel alien to your body.
Common nerve pain sensations in the leg include:
- Burning or searing - like hot coals
- Electric shock or shooting pain - sudden jolts down your leg
- Tingling or "pins and needles" - like a foot falling asleep
- Numbness - areas that feel "dead" or disconnected
- Extreme sensitivity - where light touch is painful
- Crawling sensations - like bugs under the skin
This experience is common. About 40% of people in the U.S. experience some form of sciatica during their lifetime, a frequent cause of leg nerve pain. Overall, nerve pain affects roughly 1 in 20 people.
Nerve pain is distinct because it's your body's electrical wiring misfiring. Damaged, compressed, or irritated nerves send scrambled signals to your brain, creating sensations that feel nothing like muscle soreness or joint stiffness.
This guide will break down what nerve pain feels like, its causes, and what you can do. Understanding what's happening is the first step toward relief.

What Does Nerve Pain Feel Like in the Leg?: A Guide to the Sensations
If you've ever wondered what does nerve pain feel like in leg, you're not alone in finding it hard to describe. Unlike a typical ache, nerve pain feels foreign because it stems from your body's electrical wiring.
When nerves are damaged, compressed, or irritated (a condition called neuropathy), they send scrambled signals to your brain. This sensory disruption, known as paresthesia, creates unusual and uncomfortable sensations. You've likely felt a mild version when your leg "falls asleep." Pins and needles, medically known as paresthesia, are these burning or prickling sensations. When chronic, it signals a more significant nerve issue.
Common Descriptions: What Does Nerve Pain Feel Like in the Leg?
Patients use vivid words to describe nerve pain, signaling that something needs attention.
- Burning or searing pain: Often described as a hot poker or a deep, intense heat from within. Dr. Dominic King from Cleveland Clinic notes, "Nerve pain is more of a burning, fiery pain."
- Stabbing or sharp sensations: Feel like sudden, brief knife jabs that appear without warning.
- Shooting or electric shock-like pain: A startling jolt, like a lightning bolt traveling down your leg, often triggered by simple movements.
- Tingling or "pins and needles": A persistent prickling or buzzing feeling that lasts for hours or days.
- Numbness or a "dead" feeling: Parts of the leg feel heavy, unresponsive, or disconnected, as if you're wearing a thick sock.
- Crawling or itching sensations: An unsettling feeling of bugs moving under your skin or an intense itch that can't be scratched.
- Extreme sensitivity to touch (allodynia): Normally harmless sensations, like bed sheets or a light breeze, become painful.
- Feeling of hot or cold water: An unusual sensation of liquid trickling down your skin when nothing is there.
How Nerve Pain Can Change and Progress
Nerve pain often evolves. It may start as intermittent pain that comes and goes, but can become constant over time. Many people find it worsens at night, making sleep difficult as even the light touch of bed sheets becomes unbearable.
Spreading pain is another hallmark, especially in peripheral neuropathy. Discomfort often starts in the toes and gradually moves up the legs in a "stocking-glove pattern."
As nerve issues progress, you might also notice:
- Balance and coordination challenges: Difficulty walking on uneven surfaces or navigating stairs.
- Muscle weakness: Trouble lifting your foot (a condition called "foot drop") or climbing stairs.
- Loss of sensation: This increases the risk of unnoticed injuries, like cuts or bruises, especially on the feet.
For more details on symptom development, see our guide on peripheral neuropathy symptoms.
Why Am I Experiencing Nerve Pain in My Leg? Common Causes and Conditions
Now that we've explored what does nerve pain feel like in leg, let's look at the "why." Nerve pain signals that something is interfering with your nervous system. The most common culprits are nerve compression, damage (neuropathy), inflammation, and reduced blood flow.
Let's explore the specific conditions that cause these problems.
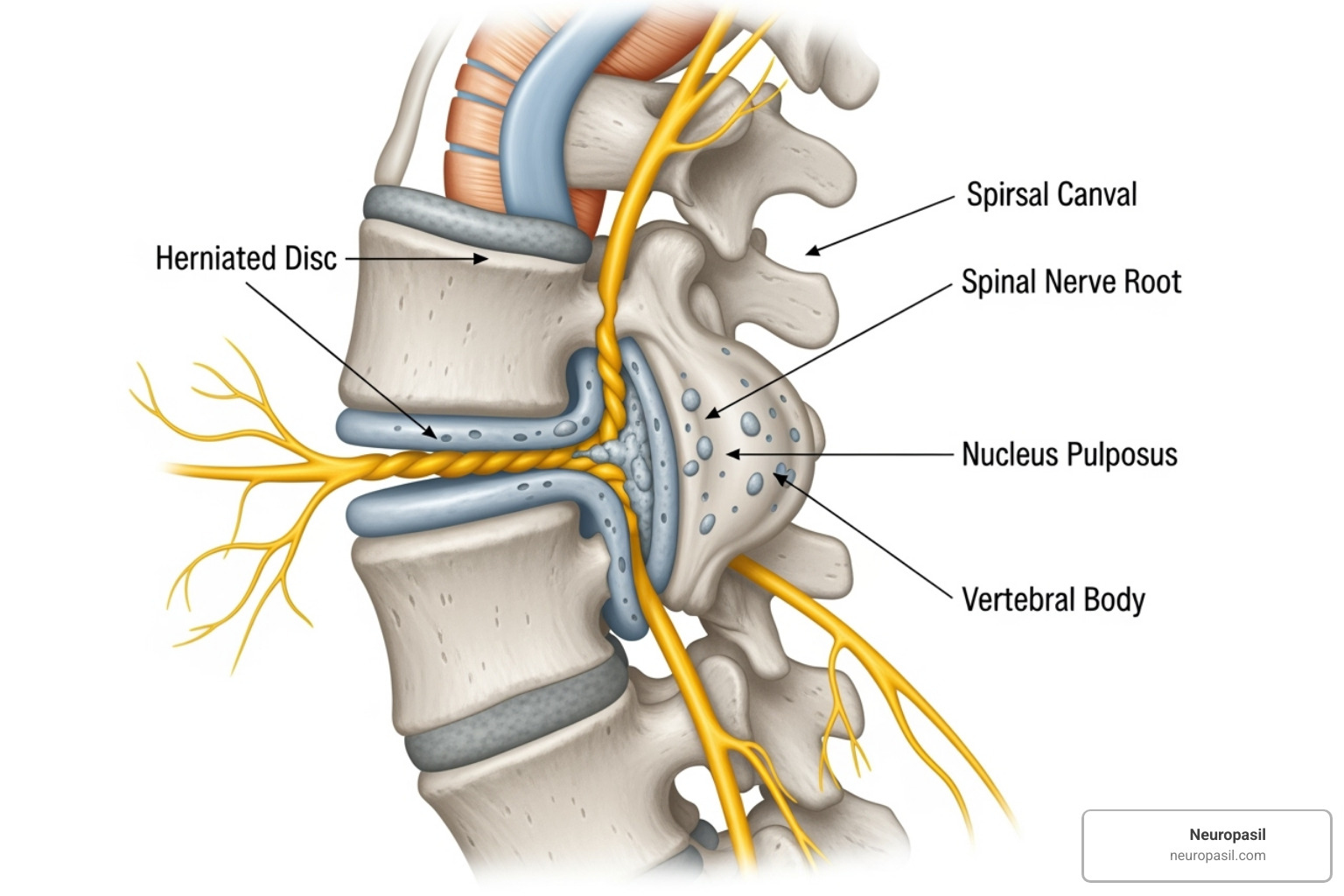
Sciatica and Radiculopathy
Sciatica is a common term for leg nerve pain, affecting about 40% of people in their lifetime. It's not a condition itself, but a symptom of irritation to the sciatic nerve, which runs from the lower back down each leg. You can learn more about its path in our guide on Understanding the Sciatic Nerve.
The radiating pain is often caused by:
- Herniated discs: Spinal cushions that bulge and press on nerve roots. 95% of lower back radiculopathy occurs at the L4-L5 and L5-S1 levels.
- Spinal stenosis: A narrowing of the spaces where nerves travel.
- Bone spurs: Bony growths that can poke at nerves.
- Piriformis syndrome: A muscle spasm in the buttock that squeezes the sciatic nerve.
Peripheral Neuropathy
This condition involves progressive damage to the peripheral nerves. Unlike sciatica, it often affects both legs equally.
Diabetes is the leading cause, with more than half of people with diabetes developing neuropathy. High blood sugar damages nerves and the small blood vessels that supply them. This typically causes a "stocking-glove" pattern of numbness and pain that starts in the toes and moves upward.
Other causes include vitamin B12 deficiency, chronic alcohol use, toxin exposure, infections like shingles, autoimmune diseases, and chemotherapy.
The Mayo Clinic offers more information on Peripheral neuropathy - Symptoms and causes.
Other Nerve-Related Conditions
- Meralgia Paresthetica: Compression of a nerve to the outer thigh, causing burning, tingling, or numbness. It's often triggered by tight clothing, weight gain, or pregnancy.
- Peroneal neuropathy: Damage to a nerve near the knee, causing "foot drop" (difficulty lifting the front of the foot) and weakness more than pain.
- Tarsal Tunnel Syndrome: A nerve is squeezed in the ankle, causing sharp, shooting pains in the foot, often worse at night.
- Neurogenic claudication: Leg pain, heaviness, or numbness that occurs with walking or standing but is relieved by sitting or leaning forward (like on a shopping cart).
Diagnosis and Differentiating Nerve Pain
When those strange sensations start affecting your leg, you need answers. The good news is that doctors have become quite skilled at solving the puzzle of nerve pain, but it takes some detective work to get to the bottom of what does nerve pain feel like in leg for you specifically.
Your journey to diagnosis typically starts with a heart-to-heart conversation with your healthcare provider. During this medical history review, they'll want to hear your story in detail. How would you describe what you're feeling? When did it all begin? Does anything make it better or worse? They'll also ask about your overall health, any medications you're taking, and whether you've had any recent injuries or illnesses.
Think of this conversation as painting a picture of your experience. The more vivid and accurate you can be about your symptoms, the clearer that picture becomes for your doctor.
Next comes the hands-on detective work during your physical examination. Your doctor will likely test your reflexes with that familiar little rubber hammer, check your muscle strength, and assess how well you can feel different sensations. They might use various textures, temperatures, or gentle pressure to map out exactly where and how your nerves are responding.
Sometimes, your doctor needs to look deeper beneath the surface. That's where specialized tests come in handy:
Nerve conduction studies (NCS) work like a speed test for your nerves. Small electrical pulses are sent through your nerves to measure how quickly signals travel. If there's damage, those signals slow down - kind of like internet running through a damaged cable.
Electromyography (EMG) often partners with NCS to measure the electrical chatter in your muscles. This test can reveal whether nerve damage is affecting how your muscles function.
For a detailed view of your spine and surrounding structures, MRI or CT scans can spot problems like herniated discs, narrowed spaces, bone spurs, or other issues that might be putting pressure on your nerves.
These tools work together to create a complete picture of what's happening in your body, guiding your doctor toward the right diagnosis and treatment approach.
Differentiating Symptoms: What Does Nerve Pain Feel Like in the Leg Compared to Other Pains?
Here's where things get interesting - and sometimes confusing. What does nerve pain feel like in leg compared to other types of pain? The distinction matters enormously because nerve pain plays by completely different rules than muscle aches or joint stiffness.
As experts at Cleveland Clinic point out, nerve pain often doesn't respond to typical pain relievers like ibuprofen or acetaminophen that work well for muscle and joint pain. It's like trying to fix a software problem with a hammer - you need the right tools for the job.
| Pain Type | What It Feels Like | Where You Feel It | What Makes It Better/Worse |
|---|---|---|---|
| Nerve Pain | Burning, shooting, electric shocks, stabbing, tingling, numbness, crawling sensations, extreme sensitivity to light touch | Follows nerve pathways (like down your leg for sciatica) or starts in fingers/toes and spreads inward | Can happen spontaneously, often worse at night, light touch may hurt, doesn't respond well to typical pain meds |
| Muscle Pain | Dull ache, soreness, throbbing, cramping, stiffness, tenderness when pressed | Specific muscle or muscle groups | Worse with use, better with rest, massage, heat/ice, responds to anti-inflammatory medications |
| Joint Pain | Achy, stiff, grinding sensation, sharp with movement | Centered around joints like knees, hips, ankles | Worse with movement or weight-bearing, stiff after rest (especially mornings), improves with appropriate movement and anti-inflammatories |
The key difference is that nerve pain often feels electric or fiery rather than the familiar ache of overworked muscles or stiff joints. Nerve pain can also bring along some unusual companions like numbness, muscle weakness, or balance problems that you typically don't see with muscle or joint issues.
If you're experiencing burning, shooting, or tingling sensations that seem to follow a path down your leg, or if light touch feels painful, you're likely dealing with nerve pain rather than a muscle strain or joint problem. Understanding this difference is crucial because it points your healthcare team toward the most effective treatment approach.
For a deeper dive into these distinctions, check out this helpful resource: What Is Nerve Pain (and How Does It Differ From Other Kinds of Pain?).
How to Manage and Support Nerve Health in the Leg

Dealing with the burning, tingling, or shooting pain in your leg can be overwhelming, but there are many effective ways to manage symptoms and support nerve health. A holistic approach that addresses the underlying cause while improving your quality of life is key.
Natural Approaches and Lifestyle Adjustments
Powerful, lasting improvements often come from everyday changes.
- Regular movement: Gentle activities like walking, stretching, and swimming improve blood flow to nerves and reduce stiffness. For sciatica, specific stretches can provide relief. Find more guidance in our article on More on Sciatica Pain.
- Healthy diet: An anti-inflammatory diet rich in colorful vegetables, fatty fish, and nuts can calm nerve irritation.
- Maintain a healthy weight: This reduces pressure on your spine and leg nerves.
- Good posture: Proper posture while sitting, standing, and sleeping prevents unnecessary strain on nerve pathways.
- Quitting smoking: Nicotine restricts blood flow, which is essential for nerve health and healing.
- Stress management: Stress amplifies pain. Techniques like meditation, deep breathing, or hobbies can break the stress-pain cycle.
Supporting Nerve Health and Comfort
Beyond lifestyle changes, you can take specific steps to support your nerves.
- Manage blood sugar: For those with diabetes, this is the most critical step to prevent further nerve damage.
- Make ergonomic adjustments: Ensure your chair and workspace don't put pressure on your nerves.
- Avoid repetitive motions: Take frequent breaks from activities that trigger your pain.
- Treat injuries promptly: Prevent minor issues from becoming chronic nerve problems.
- Strengthen your core: Strong core muscles support your spine and protect the nerve roots that go to your legs.
- Consider natural supplements: Ingredients like B vitamins (especially B12) and Alpha Lipoic Acid can support nerve health. At Neuropasil, we develop natural solutions designed to help you find comfort.
Always discuss new supplements or major lifestyle changes with your healthcare provider to ensure they are right for you.
Frequently Asked Questions about Leg Nerve Pain
Living with nerve pain brings up many questions. Here are answers to some of the most common ones about what does nerve pain feel like in leg and what to do about it.
When should I see a doctor for nerve pain in my leg?
It's always better to be cautious with nerve pain. You should see a doctor if:
- Your pain is severe, persistent, or disrupts your sleep and daily activities.
- You experience new or worsening weakness or numbness in your leg or foot.
- The pain follows an injury, such as a fall or car accident.
Seek immediate emergency care if you experience any loss of bladder or bowel control with your leg pain. This could signal cauda equina syndrome, a serious condition requiring urgent treatment.
As the Mayo Clinic advises, early diagnosis and treatment offer the best chance for controlling symptoms and preventing further nerve damage.
Can stress make nerve pain worse?
Yes, absolutely. Stress and nerve pain have a two-way relationship that can amplify discomfort. Chronic stress increases inflammation, causes muscle tension that can compress nerves, and heightens your brain's perception of pain. This can make even minor nerve irritation feel excruciating. Managing stress through relaxation techniques, exercise, or hobbies is a powerful tool for reducing pain.
Will nerve pain in my leg ever go away?
This depends on the cause of your pain and how quickly it's addressed. The outlook is often positive.
- Acute nerve pain, like many cases of sciatica, often resolves within weeks to months with proper care.
- For chronic nerve pain, significant improvement is very achievable, even if a complete cure isn't possible. Many people regain their quality of life through a combination of treatments and lifestyle changes.
The key is early intervention. The sooner you address the problem, the better your chances of preventing permanent damage. If the pain stems from an ongoing condition like diabetes, managing that disease is crucial for stabilizing or improving symptoms. Don't lose hope; with the right support, your body has a remarkable ability to heal.
Conclusion
Understanding what does nerve pain feel like in leg is the first step toward finding relief. We've explored the unique sensations—from burning and shooting pains to tingling and numbness—that signal an issue with your nervous system.
These symptoms are your body's call for attention. Whether the cause is sciatica, diabetic neuropathy, or another condition, this knowledge is empowering. It helps you communicate effectively with your doctor, differentiate nerve pain from other aches, and understand when to seek professional help.
Hope for relief is real. While nerve pain can be overwhelming, many people find significant improvement through early intervention, medical care, and natural lifestyle approaches. The journey requires patience, but you don't have to walk it alone.
At Neuropasil, we are committed to providing education and natural solutions to support your nerve health strategy. Every step toward better nerve health matters, and we're here to help.
Ready to explore natural approaches to nerve comfort? Find natural solutions for nerve pain relief and learn how we can be part of your journey toward feeling better.














