Understanding the Pain and Finding Your Path to Relief
If a sciatica flare up has you searching for fast relief from its sharp, radiating leg pain, you're in the right place. Here's what you need to know.
Immediate Relief:
- Stay active with gentle movement; avoid bed rest.
- Apply cold packs for 15-20 minutes to reduce inflammation.
- Use heat therapy after 48 hours to relax muscles.
- Try gentle stretches like the knee-to-chest pose.
- Apply a topical pain relief cream to the affected area.
When to See a Doctor:
- Pain persists for more than 4-6 weeks.
- You lose bladder or bowel control.
- Severe weakness or numbness develops in your leg.
Sciatica affects about 40% of people in the U.S., but the good news is that 80-90% recover without surgery, often within a few weeks. A sciatica flare up occurs when the sciatic nerve, your body's longest nerve, is compressed or irritated by a herniated disc, spinal stenosis, or muscle strain. This causes the tell-tale burning, tingling, or electric shock sensation.
I'm Tony Enrico, and at Neuropasil, we've helped thousands find relief from nerve and muscle pain, including sciatica flare up episodes, by understanding triggers and applying effective relief strategies.
Sciatica flare up terms to know:
What Is a Sciatica Flare-Up and What Does It Feel Like?
Sciatica isn't a condition but a symptom of an issue affecting the sciatic nerve. It feels like a sharp, shooting pain or electric shock traveling from your lower back down your leg, making daily activities like standing or walking difficult.
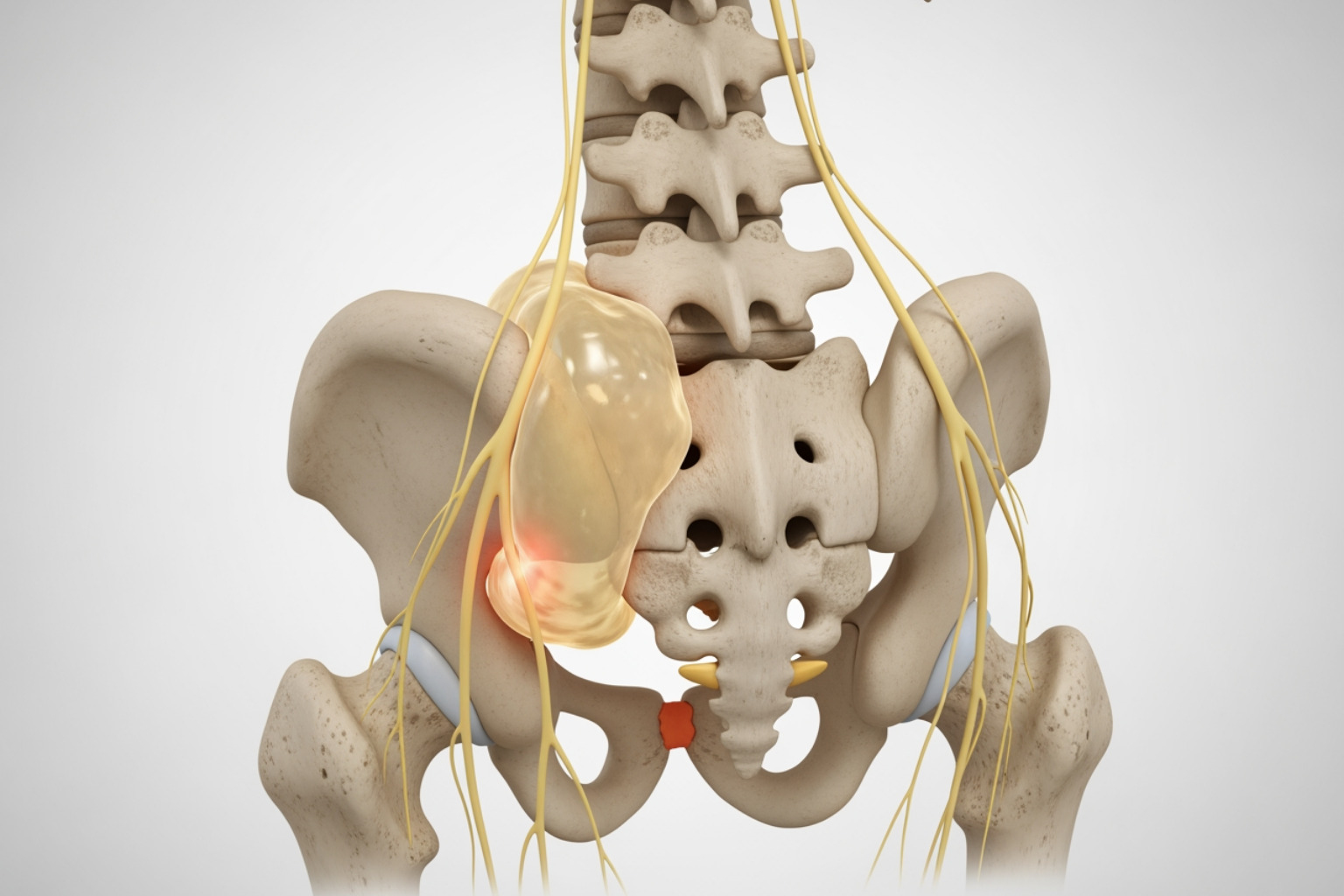
A sciatica flare up occurs when the sciatic nerve—the body's longest nerve, running from the lower back down to the foot—gets irritated, inflamed, or compressed. This nerve root compression is technically called radiculopathy.
Several factors can cause this compression:
- Herniated Disk: The most common cause, where a spinal disc's soft center pushes out and presses on nerve roots.
- Spinal Stenosis: A narrowing of the spinal canal that puts pressure on the sciatic nerve, common in older adults.
- Bone Spurs: Bony growths on the vertebrae that can impinge on nerve roots.
- Piriformis Syndrome: When the piriformis muscle in the buttocks tightens and compresses the sciatic nerve.
- Other Causes: Less common triggers include tumors, infections, or lower back injuries.
Treating the root cause is key for long-term relief. As medical experts note, sciatica is a symptom involving radiating leg pain, not just back pain. Identifying the true underlying issue is crucial for effective treatment. What doctors wish patients knew about sciatica.
Symptoms of a Sciatica Flare-Up
A sciatica flare up has unmistakable symptoms, typically affecting one side of the body:
- Sharp, Shooting Pain: An intense, electric shock-like sensation down the leg.
- Burning Sensation: A searing or burning pain along the nerve's path.
- Tingling or "Pins and Needles": A sensation of the leg "falling asleep."
- Muscle Weakness: A weak feeling in the affected leg or foot, sometimes leading to "foot drop."
- Numbness: Reduced sensation or numbness in parts of the leg or foot.
- Pain Worse When Sitting: Pain often intensifies with prolonged sitting, coughing, or sneezing.
- One-Sided Pain: Symptoms usually affect only one leg.
The defining characteristic of sciatica is pain radiating down the leg. For more details on symptoms and their causes, explore More on sciatica symptoms and causes.
The Most Common Triggers for a Sciatica Flare Up
Understanding what triggers your sciatica flare up is the first step toward managing it. While an underlying issue like a herniated disc may be constant, certain factors can aggravate it. Recognizing these triggers empowers you to make proactive changes.
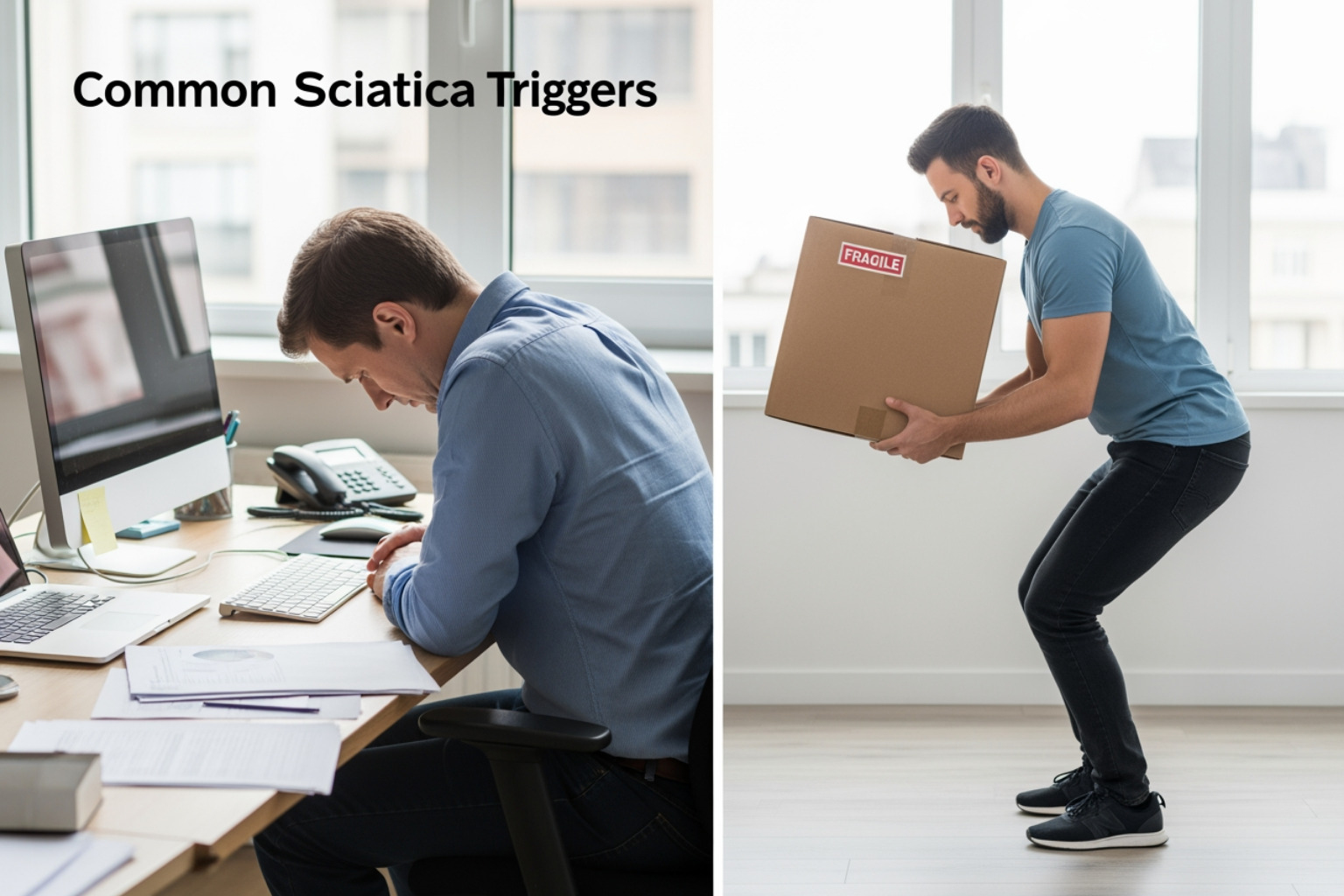
Physical and Postural Triggers
Daily habits and movements play a significant role in triggering a sciatica flare up:
- Prolonged Sitting: Sitting for long periods, especially with poor posture, puts pressure on your lower back and can compress the sciatic nerve.
- Poor Posture: Slouching or hunching while sitting, standing, or sleeping can misalign your spine and stress the sciatic nerve.
- Improper Lifting: Lifting heavy objects by bending at your waist instead of your knees strains your lower back and can trigger sciatica.
- Sudden Twisting: Quick, uncontrolled twisting movements can irritate the sciatic nerve, especially when lifting.
- Muscle Strain or Spasm: Tight muscles in the lower back, hips, or glutes (like the piriformis) can directly compress the nerve.
- Lack of Core Strength: A weak core forces your back muscles to overwork, leading to fatigue and potential injury that can affect the sciatic nerve.
Learn more about how pinched nerves contribute to pain in this A-Z Guide to Pinched Nerves.
Lifestyle and Environmental Factors
Broader lifestyle choices can also influence your risk of a sciatica flare up:
- Excess Weight: Extra weight, especially around the abdomen, increases the load on your spine and can contribute to nerve compression.
- Sedentary Lifestyle: Lack of physical activity leads to weak muscles, stiff joints, and poor circulation, increasing sciatica risk.
- High Heels: Wearing high heels alters your posture, pushing your pelvis forward and increasing pressure on the lower back and sciatic nerve.
- Pregnancy-Related Pressure: Hormonal changes and the weight of a growing uterus can loosen ligaments and put direct pressure on the sciatic nerve. Find tips here: How to Deal with Sciatica While Pregnant.
- Smoking: Nicotine can damage spinal tissue and reduce blood supply to spinal structures, weakening them and increasing the risk of chronic pain.
The Cleveland Clinic also provides comprehensive information on sciatica risk factors: Sciatica information from Cleveland Clinic.
Emotional and Dietary Triggers
Your emotional state and diet can also play a role in a sciatica flare up:
- Stress and Anxiety: High stress levels can cause muscle tension that irritates the sciatic nerve and may also lower your pain threshold.
- Inflammatory Diet: A diet high in processed foods, sugar, and unhealthy fats can promote systemic inflammation, which may exacerbate nerve pain. Following an anti-inflammatory diet may help manage symptoms.
- Dehydration: Your spinal discs are partly made of water, and dehydration can negatively affect their health, potentially contributing to conditions that cause sciatica.
For insights on how diet impacts chronic pain, see our guide: Beyond Meds: Natural Ways to Ease Fibromyalgia Symptoms.
How to Get Immediate Relief at Home
When a sciatica flare up strikes, you need immediate relief. These effective self-care strategies can help you manage pain and reduce inflammation at home.
For more proven strategies, check out: Sciatica SOS: Proven Strategies for Immediate Pain Relief.
Gentle Movement and Stretching
Avoiding prolonged bed rest is crucial. While a day of rest might be needed for severe pain, inactivity can worsen stiffness. Gentle movement helps shorten the duration of symptoms.
Try these gentle movements and stretches:
- Light Walking: Short walks keep your spine mobile and muscles from tightening.
- Cat-Cow Stretch: On your hands and knees, gently arch your back on an inhale and round your spine on an exhale to mobilize the spine.
- Knee-to-Chest Stretch: Lie on your back and gently pull one knee toward your chest, holding for 20-30 seconds. Repeat on the other side.
- Seated Hamstring Stretch: Sit with one leg extended, the other bent. Lean forward from your hips with a straight back to feel a gentle stretch.
Stop immediately if any stretch increases your pain.
Hot and Cold Therapy
Alternating hot and cold therapy can be very effective for a sciatica flare up:
- Cold Packs for Inflammation: For the first 48 hours, apply a cold pack wrapped in a towel to the painful area for 15-20 minutes at a time. Cold constricts blood vessels, reducing inflammation and numbing pain. Research supports cryotherapy for pain relief: Scientific research on cryotherapy for pain.
- Heat Packs for Muscle Relaxation: After 48 hours, switch to heat. A warm bath or heating pad can relax tight muscles and improve blood flow.
- Alternating Therapy: Some people find relief by alternating between hot and cold. Experiment to see what works for you.
Topical Solutions for a Sciatica Flare Up
For targeted relief, topical creams can be a game-changer during a sciatica flare up. At Neuropasil, we specialize in natural, fast-acting topical solutions. Our creams are powered by a blend of Aloe, Urea, and Menthol to address nerve pain and sore muscles.
How they work:
- Cooling and Soothing: Menthol provides a cooling sensation that distracts from pain signals.
- Deep Penetration: Urea helps the active ingredients penetrate deeper into the tissue.
- Anti-Inflammatory Support: Aloe vera offers soothing and anti-inflammatory properties.
Applying a nerve pain relief cream directly to your lower back, buttocks, and leg can provide localized comfort. Many of our customers across the United States have found Neuropasil invaluable for managing sciatica and other nerve pains.
For a guide on choosing the right cream, explore: The Ultimate Guide to Best Cream for Sciatica Pain.
Long-Term Strategies to Prevent Future Flare-Ups
While immediate relief is crucial during a sciatica flare up, preventing future episodes is the real goal. This requires a proactive approach to build resilience in your body.
For a comprehensive look at key changes, check out: How to Stop Debilitating Sciatica Pain with 5 Easy Changes.
Core Strengthening and Regular Exercise
A strong core acts as a natural support for your spine, preventing a sciatica flare up. Regular, low-impact exercise is key to protecting your back and nerve health.
-
Low-Impact Aerobics: Choose activities that don't jar your spine, such as:
- Swimming: Water's buoyancy reduces stress on your spine and joints.
- Yoga: Gentle poses can improve flexibility, strength, and relaxation.
- Pilates: This focuses on core strength, posture, and body awareness.
-
Core Exercises: Target deep abdominal and back muscles with exercises like:
- Planks: Strengthens your entire core without spinal movement.
- Bird-Dog: Improves core and back stability.
- Pelvic Tilts: Strengthens deep abdominal muscles.
Consistency is key, even 15-30 minutes a few times a week. The principle of targeted exercise for strength and flexibility is universal for pain prevention: Cheat Sheet to Shoulder Recovery Workouts.
Ergonomics and Lifestyle Adjustments for a Sciatica Flare Up
Thoughtful adjustments to your daily habits can significantly reduce your risk of a sciatica flare up.
Here's a list of ergonomic and lifestyle tips:
-
Workspace Ergonomics:
- Use an ergonomic chair with good lumbar support.
- Keep feet flat on the floor, knees slightly higher than hips, and avoid crossing your legs.
- Position your monitor at eye level.
- Take regular breaks to stand and stretch every 30-60 minutes.
-
Proper Posture:
- When standing, rest one foot on a stool to relieve back pressure.
- Sleep on your side with a pillow between your knees or on your back with a pillow under your knees.
-
Correct Lifting:
- Always bend at your knees, not your waist, with a straight back.
- Hold objects close to your body and avoid twisting while lifting.
- Healthy Weight: A balanced diet and regular exercise are crucial to maintain a healthy weight and reduce spinal strain.
- Quitting Smoking: Nicotine impairs blood flow to spinal tissues, increasing the risk of degeneration and pain.
For more insights into managing lower back pain, explore: Lower Back Pain 101: Causes & Relief.
When to See a Doctor for Sciatica Pain
While many sciatica flare ups can be managed at home, it's crucial to know when to seek professional medical help to avoid serious complications.
Harvard Health offers guidance on when to see a doctor: What should you do when sciatica flares?.
Red Flag Symptoms Requiring Immediate Attention
These critical signs warrant immediate medical evaluation (go to an emergency room):
- Loss of Bladder or Bowel Control: This may indicate Cauda Equina Syndrome, a rare but severe condition requiring urgent intervention.
- Sudden, Severe Weakness or Numbness: Seek immediate care for significant, rapidly worsening weakness or numbness in your leg, foot, or groin.
- Pain After a Traumatic Injury: If sciatica pain starts after a fall or accident, get checked for spinal damage.
- Trouble Walking or Balancing: If pain or weakness severely impairs your ability to walk, see a doctor immediately.
When to Schedule a Doctor's Visit
Consult a healthcare professional in these situations:
- Pain Persists: If your sciatica flare up doesn't improve after a few weeks of consistent self-care.
- Severe Pain: If the pain is severe and limits daily activities despite home treatment.
- Ineffective Self-Care: If home remedies haven't provided significant relief.
- Recurring Flare-Ups: If you experience frequent flare-ups, a doctor can help identify the underlying cause and create a long-term management plan.
The Mayo Clinic also emphasizes when to seek medical attention: Sciatica - Symptoms and causes from Mayo Clinic. Early diagnosis can prevent acute sciatica from becoming a chronic condition.
Frequently Asked Questions about Sciatica Flare-Ups
We understand you have questions about a sciatica flare up. Here are answers to some common inquiries.
How long does a sciatica flare-up typically last?
The duration of a sciatica flare up varies. For many, it lasts from a few days to a couple of weeks. According to experts, most people (80-90%) with sciatica improve without surgery, often within several weeks. Recovery time depends on the severity of nerve compression, your overall health, and adherence to treatment. If pain persists, it can become chronic.
Should I rest or stay active during a flare-up?
The general advice is to stay gently active. While a day or two of rest may be necessary for severe pain, prolonged bed rest is discouraged as it can lead to stiffness and worsen pain.
We recommend:
- Gentle Movement: Light walking and gentle stretches improve circulation and reduce stiffness.
- Listen to Your Body: Use a "traffic light" approach to pain. Green zone (mild pain) is okay to continue; yellow zone (moderate pain) means modify the activity; red zone (severe pain) means stop immediately.
- Modify Activities: If an activity hurts, find a different way to do it or avoid it temporarily.
The goal is to balance activity and rest to maintain flexibility without aggravating your pain.
Can a sciatica flare-up affect both legs?
Sciatica typically affects only one leg because nerve compression usually occurs on one side of the spine.
However, in rare cases, a sciatica flare up can affect both legs. This might happen with a central disc herniation or spinal stenosis that compresses nerve roots on both sides. Sciatica symptoms in both legs is a "red flag" that warrants immediate medical evaluation, as it can indicate a more serious condition like Cauda Equina Syndrome.
Conclusion
A sciatica flare up is a painful challenge, but understanding its triggers and management strategies is the first step toward relief. Most people find significant improvement by combining immediate self-care with long-term lifestyle adjustments.
Key takeaways:
- Identify your triggers to avoid them.
- Use home remedies like gentle movement, hot/cold therapy, and topical solutions for immediate relief.
- Focus on long-term prevention through core strength, good posture, and a healthy weight.
- Know when to see a doctor for persistent pain or red flag symptoms.
For targeted, on-the-spot relief from nerve and muscle pain during a flare-up, many find comfort with natural topical solutions like Neuropasil. Our creams, with Aloe, Urea, and Menthol, are designed for fast-acting, soothing relief right where you need it.
Find your fast-acting pain relief cream today and take a proactive step towards managing your sciatica flare up effectively.
References
- What doctors wish patients knew about sciatica – AMA
- Sciatica: Simple Symptoms, Complex Causes Explained – Neuropasil Blog
- A-Z Guide to Pinched Nerves – Neuropasil Blog
- How to Deal with Sciatica While Pregnant – Neuropasil Blog
- Sciatica – Cleveland Clinic
- Beyond Meds: Natural Ways to Ease Fibromyalgia Symptoms – Neuropasil Blog
- Sciatica SOS: Proven Strategies for Immediate Pain Relief – Neuropasil Blog
- Cryotherapy for pain – PubMed
- The Ultimate Guide to Best Cream for Sciatica Pain – Neuropasil Blog
- How to Stop Debilitating Sciatica Pain with 5 Easy Changes – Neuropasil Blog
- Cheat Sheet to Shoulder Recovery Workouts – Neuropasil Blog
- Lower Back Pain 101: Causes & Relief – Neuropasil Blog
- What should you do when sciatica flares? – Harvard Health
- Sciatica – Symptoms and causes – Mayo Clinic
- Sciatica – Johns Hopkins Medicine
- Sciatica Causes – Spine-health
- Foods that fight inflammation – Harvard Health
- Five Ways to Maintain a Healthy Spine – University of Maryland Medical System














