Understanding Why Your Heel Hurts
What causes heel pain? The answer isn't always simple, but most heel pain stems from a handful of common conditions. Here's what you need to know:
The Most Common Causes:
- Plantar fasciitis - Inflammation of the tissue band running along your foot's bottom (the #1 cause)
- Achilles tendon issues - Irritation or inflammation at the back of your heel
- Heel spurs - Bony growths often linked to chronic plantar fasciitis
- Bursitis - Inflamed fluid-filled sacs cushioning your heel
- Stress injuries - Small cracks or overuse damage to the heel bone
- Nerve compression - Pinched nerves like tarsal tunnel syndrome
Less Common but Important:
- Structural problems (flat feet, high arches, fat pad thinning)
- Systemic diseases (arthritis, diabetes-related nerve damage)
- Injuries (bone bruises, fractures)
Most heel pain develops gradually from overuse, poor footwear, or abnormal walking patterns. The good news? About 95% of cases improve with conservative treatment - no surgery needed.
Heel pain is one of the most common foot complaints that brings people to doctors and podiatrists. It can strike suddenly or build slowly over time, turning simple activities like getting out of bed or walking to your car into painful ordeals.
Your heel - specifically the calcaneus bone cushioned by a thick pad of fatty tissue - bears tremendous stress with every step. In fact, every mile you walk puts about 60 tons of pressure on each foot. When that pressure exceeds what your heel can handle, pain follows.
Why does this matter? Because understanding what causes heel pain is the first step toward finding relief. Whether you're an athlete dealing with training pain, someone whose job keeps you on their feet all day, or just trying to enjoy a morning walk without wincing, identifying the root cause helps you choose the right treatment approach.
This guide will walk you through the most common causes of heel pain, help you recognize which condition might be affecting you, explain when to seek professional help, and share practical relief strategies you can start using today.
I'm Tony Enrico, and through my work with Neuropasil, I've helped thousands of people find relief from nerve and muscle pain, including the stubborn discomfort that comes with conditions like plantar fasciitis. My mission is to help you understand what causes heel pain so you can take the right steps toward lasting comfort and get back to doing what you love.

Important What causes heel pain? terms:
What Causes Heel Pain? The Most Common Culprits
When we talk about what causes heel pain, we often think of a few key conditions that account for the majority of cases. These are the usual suspects that bring people into our offices seeking relief. Understanding these common culprits is crucial for effective treatment.

The most common causes of heel pain typically involve inflammation or damage to the soft tissues surrounding the heel bone. Let's explore the specifics:
Plantar Fasciitis: The #1 Cause of Stabbing Heel Pain
If you've ever felt a sharp, stabbing pain in your heel, especially with your first steps in the morning, you've likely experienced plantar fasciitis. This condition is, by far, the most common answer to what causes heel pain?
Plantar fasciitis occurs when the plantar fascia, a thick band of tissue that runs along the bottom of your foot from your heel to your toes, becomes inflamed. This ligament acts like a shock absorber and supports the arch of your foot. When it's subjected to excessive tension and stress, small tears can develop, leading to inflammation and pain.
The pain from plantar fasciitis is often described as a sharp, stabbing sensation, particularly noticeable:
- With the first steps out of bed in the morning.
- After long periods of rest, such as sitting for an extended time.
- After exercise, though it may lessen during activity.
Risk factors for plantar fasciitis include having flat feet or high arches, prolonged standing, obesity, and wearing unsupportive footwear. For more in-depth information, you can explore our guide on Plantar Fasciitis.
Achilles Tendon Discomfort: Pain at the Back of Your Heel
Another frequent answer to what causes heel pain? is Achilles tendon discomfort, often manifesting as Achilles tendinitis. The Achilles tendon is the largest and strongest tendon in your body, connecting your calf muscles to your heel bone. It's crucial for walking, running, and jumping.
When this tendon becomes inflamed or irritated, it can cause pain at the back of your heel. This is particularly common among runners and other athletes due to overuse and repetitive stress. The pain may start as a mild ache after exercise and gradually worsen over time.
Symptoms often include:
- Pain and stiffness along the Achilles tendon, especially in the morning.
- Pain along the back of the heel that worsens with activity.
- Tenderness or swelling at the back of the heel.
Maintaining the flexibility of your Achilles tendon is key to preventing this type of heel pain. For general information about Heel Pain, you can refer to our resources.
Heel Spurs: Are They the Real Problem?
Heel spurs are bony growths that can develop on the underside of your heel bone, often where the plantar fascia attaches. While they might sound like a direct cause of pain, the truth is a bit more nuanced. It's estimated that a significant portion of the population (studies show about one in 10 individuals) has heel spurs without experiencing any pain whatsoever.
So, if you have a heel spur, what causes heel pain in your case? Often, the pain isn't from the spur itself, but from the associated inflammation of the surrounding soft tissues, particularly the plantar fascia. Heel spurs are frequently seen in people with long-standing plantar fasciitis, as the chronic tension and inflammation can lead to calcium deposits forming over time.
Think of it this way: the spur is often a symptom of chronic stress, not the primary cause of your discomfort. The actual pain usually comes from the inflamed plantar fascia or other irritated soft tissues nearby. To learn more about these bony growths, you can find further details on heel spurs.
Less Common Conditions That Can Lead to Heel Pain
While plantar fasciitis and Achilles tendon issues dominate the discussion of what causes heel pain, other, less common conditions can also be culprits. These may involve structural problems, nerve impingements, or even systemic diseases.
Structural Issues and Injuries
Several structural issues and direct injuries can also answer the question, "what causes heel pain?"
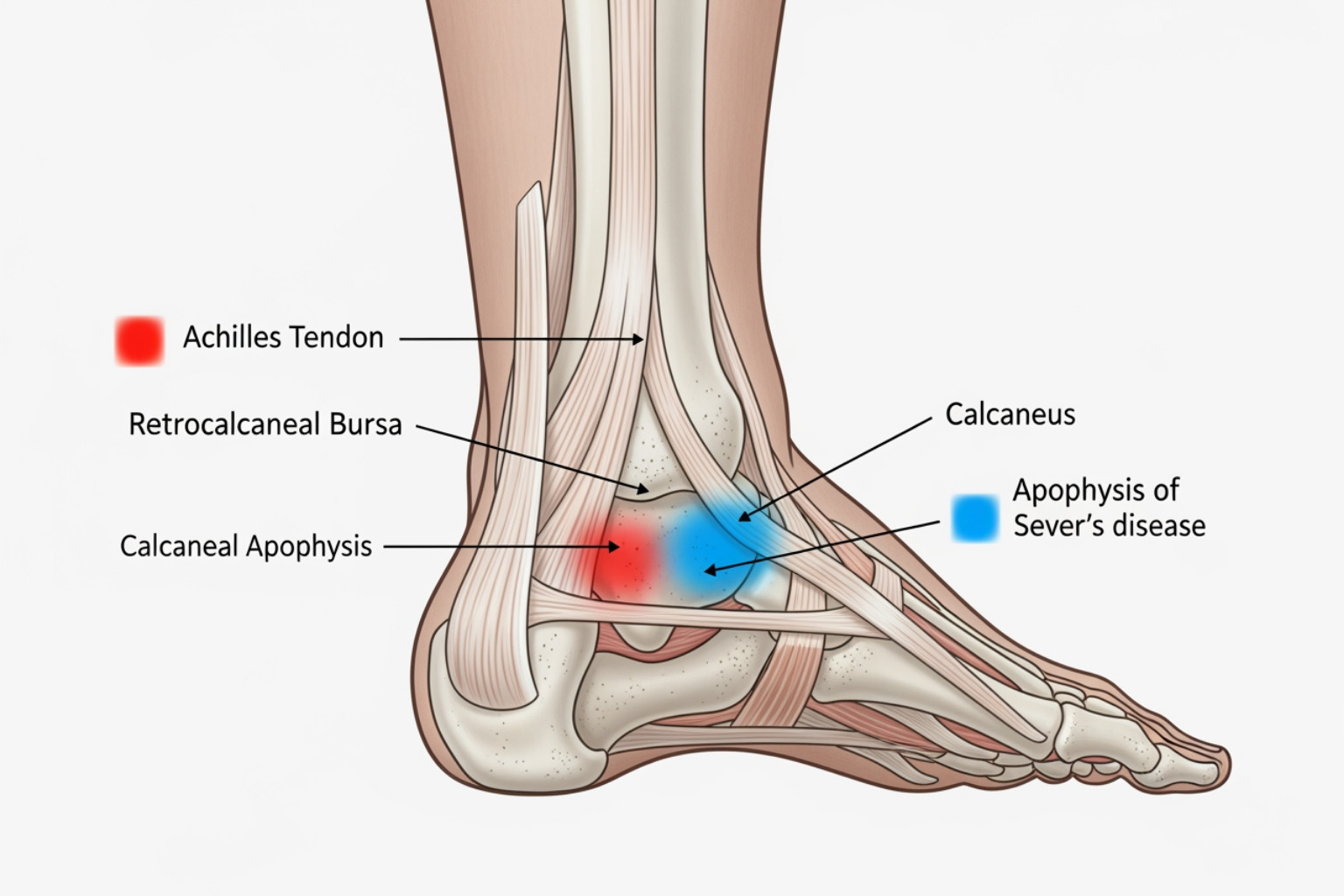
- Bursitis: Bursae are small, fluid-filled sacs that cushion bones, tendons, and muscles around joints. When the bursa located at the back of your heel (retrocalcaneal bursa) becomes inflamed, typically from overuse or pressure from tight shoes, it leads to pain, swelling, and tenderness. This is known as retrocalcaneal bursitis.
- Haglund's Deformity (Pump Bump): This is a bony enlargement on the back of the heel bone, often at the point where the Achilles tendon attaches. It's sometimes called "pump bump" because it can be exacerbated by the rigid backs of certain shoes, like high heels, which rub against the area and cause irritation and bursitis.
- Stress Injury (Stress Fracture): Unlike an acute fracture from a sudden injury, a stress injury is a tiny crack in the heel bone (calcaneus) that develops over time from repetitive stress. This is common in athletes or individuals who suddenly increase their activity levels. The pain typically worsens with activity and improves with rest.
- Fat Pad Atrophy: The heel is naturally cushioned by a thick pad of fatty tissue. Over time, due to aging, repeated impact, or certain medical conditions (like diabetes), this fat pad can thin out or lose its elasticity. When this happens, the heel bone loses some of its natural shock absorption, leading to pain, especially when walking on hard surfaces.
- Bone Bruise (Contusion): A direct impact, like stepping hard on a sharp object or landing awkwardly, can cause a bone bruise on the heel. This results in sharply painful, localized tenderness.
- Sever’s Disease (Calcaneal Apophysitis): This condition is the most common cause of heel pain in children aged eight to 16, particularly active children. It's an inflammation of the growth plate in the heel bone, caused by repetitive stress and muscle strain during growth spurts, often from activities like running and jumping. The pain typically resolves as the child's growth plate fuses. You can find more details on various heel pain causes from Mayo Clinic.
Nerve-Related Pain and Systemic Diseases
Sometimes, the answer to what causes heel pain lies outside of direct structural damage to the heel itself, involving nerves or underlying systemic conditions.
- Tarsal Tunnel Syndrome: Similar to carpal tunnel syndrome in the wrist, tarsal tunnel syndrome occurs when the tibial nerve, which runs along the inside of your ankle and into your foot, becomes compressed or pinched. This can cause pain, numbness, tingling, or burning sensations in the heel, arch, and toes. For more insights into nerve compression, you might find our article on Freedom from the Squeeze: How to Relieve a Pinched Nerve helpful.
- Peripheral Neuropathy: While peripheral neuropathy can affect various parts of the body, it often manifests in the feet. Damage to the peripheral nerves can lead to pain, burning, tingling, or numbness in the heels and other areas of the foot. One common cause of peripheral neuropathy is diabetes. For a deeper dive into this connection, refer to Diabetic Neuropathy Explained: Navigating Nerve Pain with Diabetes.
- Arthritis (Rheumatoid, Gout, Psoriatic, Reactive, Ankylosing Spondylitis): Various forms of arthritis can cause heel pain. Inflammatory arthritis conditions can affect the joints in the foot, including those around the heel. Gout, for example, can cause sudden, severe pain and swelling in the foot, often affecting the big toe but capable of impacting the heel. Rheumatoid arthritis can cause joint inflammation and damage throughout the body, including the feet. If you're interested in understanding more about arthritis, check out our Arthritis 101 guide.
Diagnosis, Risk Factors, and When to See a Doctor
Understanding what causes heel pain is a critical first step, but just as important is knowing if you're at risk, how a medical professional diagnoses the issue, and when it's time to seek their expertise.
Are You at Risk for Developing Heel Pain?
Several factors can increase your likelihood of developing heel pain. Recognizing these risk factors can help us take proactive steps to prevent discomfort.
- Obesity/Excess Weight: Carrying extra pounds places increased stress on your feet, especially your heels, which bear the brunt of your body weight with every step. This added pressure can strain the plantar fascia and other heel structures.
- Improper Footwear: Wearing shoes that lack adequate arch support, cushioning, or stability can contribute significantly to heel pain. Worn-out shoes, high heels, or walking barefoot on hard surfaces regularly are also common culprits.
- High-Impact Activities: Sports and activities that involve a lot of running, jumping, or sudden stops and starts (like basketball, tennis, or long-distance running) put repetitive stress on the heels, increasing the risk of conditions like plantar fasciitis and Achilles tendinitis.
- Prolonged Standing: Jobs or activities that require long hours on your feet, especially on hard surfaces like concrete, can lead to overuse and inflammation of heel tissues.
- Foot Mechanics (Flat Feet, High Arches): Both excessively flat feet (pronation) and very high arches can alter the distribution of weight across your foot, placing abnormal stress on the plantar fascia and other heel structures.
- Age: While heel pain can affect anyone, certain conditions like plantar fasciitis are more common in middle-aged individuals (40-60 years old). Sever's disease, as mentioned, is specific to active children.
- Pregnancy: The added weight and hormonal changes during pregnancy can loosen ligaments and increase pressure on the feet, sometimes leading to heel pain.
How Doctors Diagnose the Cause of Heel Pain
When you visit a healthcare provider for heel pain, their goal is to pinpoint what causes heel pain in your specific situation. This typically involves a thorough process:
-
Medical History: Your doctor will ask detailed questions about your symptoms, including:
- When did the pain start?
- Where exactly does it hurt (bottom, back, side)?
- What activities make it worse or better?
- Is the pain worse in the morning or after rest?
- What kind of shoes do you wear?
- What are your daily activities or exercise routines?
-
Physical Exam: The doctor will carefully examine your foot and ankle. This often includes:
- Palpation: Gently pressing on different areas of your heel to locate the precise source of pain and tenderness.
- Range of Motion: Assessing the flexibility and strength of your ankle and foot muscles.
- Gait Analysis: Observing how you walk to identify any biomechanical issues or abnormal walking styles that might be contributing to the pain.
-
Imaging Tests: While not always necessary, imaging can help confirm a diagnosis or rule out other conditions:
- X-rays: These can show bony abnormalities like heel spurs, stress fractures, or signs of arthritis.
- MRI (Magnetic Resonance Imaging) or Ultrasound: These are less commonly used for initial diagnosis but may be ordered if X-rays are inconclusive or if your doctor suspects soft tissue damage (like an Achilles tendon tear) or nerve entrapment.
A comprehensive evaluation helps ensure an accurate diagnosis, which is the foundation for an effective treatment plan. For more information on diagnosis, you can refer to the American Academy of Orthopaedic Surgeons.
When to Seek Medical Help for Your Heel Pain
While many cases of mild heel pain can improve with rest and home care, it's crucial to know when to consult a medical professional. Don't hesitate to seek help if:
- Severe Pain and Swelling: If you experience intense pain, significant swelling, inflammation, or stiffness in your heel, especially after an injury.
- Inability to Walk Normally: If the pain is so severe that you cannot put weight on your heel or walk properly.
- Pain Persists Over 2 Weeks: If your heel pain doesn't improve after a couple of weeks of consistent rest, ice, and other home remedies.
- Signs of Infection: If you notice redness spreading, warmth, pus, or develop a fever along with your heel pain.
- Numbness or Tingling: If you experience numbness, tingling, or a "pins and needles" sensation in your heel or foot, as this could indicate nerve involvement.
Ignoring persistent heel pain can lead to chronic issues and potentially impact your overall mobility and quality of life. If you're unsure, it's always best to get a professional opinion. You can find an orthopaedist through resources like the AAOS.
A Practical Guide to Heel Pain Relief and Prevention
The good news is that most heel pain responds well to conservative treatments. Less than 5% of patients with chronic heel pain ultimately require surgery. This means that with the right approach, we can often find relief and get you back on your feet without invasive procedures.
At-Home Remedies for Fast Relief
When trying to manage heel pain at home, a multi-faceted approach often yields the best results. Here are some strategies we recommend:
- Rest and Activity Modification: This is often the first and most crucial step. Avoid activities that aggravate your heel pain, such as prolonged standing, running, or high-impact sports. Switch to low-impact exercises like swimming or cycling to stay active without stressing your heels.
- Ice Therapy: Applying ice can help reduce inflammation and numb the pain. Use an ice pack or a bag of frozen peas wrapped in a thin towel for 15-20 minutes, several times a day.
-
Stretching Exercises: Regular stretching can significantly relieve tension in the plantar fascia and calf muscles.
- Calf Stretch: Lean against a wall with one foot forward, knee bent, and the other foot back, leg straight. Lean forward until you feel a stretch in your calf. Hold for 30 seconds, repeat 3 times per leg.
- Plantar Fascia Stretch: Sit down and cross your affected foot over your opposite knee. Grab your toes and pull them back towards your shin until you feel a stretch in the arch of your foot. Hold for 30 seconds, repeat 3 times per foot.
- Towel Stretch: Sit with your legs extended. Loop a towel around the ball of your affected foot and gently pull the towel towards you, keeping your knee straight. Hold for 30 seconds, repeat 3 times.
- Over-the-Counter Pain Relievers: Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen can help reduce pain and inflammation. Always follow dosage instructions.
- Supportive Footwear: Wear shoes that provide good arch support and cushioning. Avoid walking barefoot, especially on hard surfaces. Consider wearing slippers or sandals with arch support around the house. For more ideas on how to find comfort, check out our guide on Step Up Your Comfort: Remedies for Aching Feet.
- Topical Pain Relief Creams: For targeted relief, topical creams can be a great option. Products containing ingredients like menthol, aloe, and urea can help soothe discomfort and reduce inflammation. Our Neuropasil nerve pain relief cream, for instance, is formulated to provide fast-acting relief for various types of pain, including the discomfort associated with conditions like plantar fasciitis. You can learn more about finding effective solutions in The Complete Guide to Effective Foot Pain Creams.
When to Seek Professional Care
While at-home remedies are often effective, sometimes professional intervention is necessary to truly understand what causes heel pain and develop a comprehensive treatment plan.
- Physical Therapy Guidance: A physical therapist can provide custom exercises, stretches, and techniques to strengthen the muscles supporting your foot, improve flexibility, and correct gait abnormalities. They might also use modalities like massage or ultrasound therapy.
- Custom Recommendations from a Healthcare Provider: Your doctor might recommend specific shoe inserts (orthotics) to provide extra support, correct biomechanical imbalances, or cushion your heel. These can be over-the-counter or custom-made.
- Night Splints: For plantar fasciitis, wearing a night splint can be very effective. It holds your foot in a slightly flexed position while you sleep, gently stretching the plantar fascia and Achilles tendon, which can significantly reduce morning pain.
- Medical Evaluation for Persistent Pain: If your pain persists despite consistent home care and physical therapy, your doctor may consider other options like corticosteroid injections (though these are used sparingly due to potential tissue weakening) or Extracorporeal Shockwave Therapy (ESWT) for stubborn cases.
- Surgery (Rare, Last Resort): As mentioned, surgery is rarely needed for heel pain, typically only considered after 9-12 months of unsuccessful non-surgical care. It may involve releasing the plantar fascia, removing a heel spur, or addressing nerve compression.
Simple Steps to Prevent Heel Pain
Prevention is always better than cure! By adopting some simple habits, we can significantly reduce our risk of developing heel pain:
- Maintain a Healthy Weight: Reducing excess weight lessens the load on your feet and heels, easing stress on the plantar fascia and other structures.
- Wear Properly Fitting, Supportive Shoes: Choose shoes with good arch support, adequate cushioning, and a firm heel counter. Ensure they fit well – not too tight, not too loose.
- Avoid Worn-Out Shoes: Replace athletic shoes every 300-500 miles or when the cushioning and support are visibly worn. We even recommend rotating between two pairs of shoes to allow cushioning materials to rebound between uses.
- Warm-Up and Stretch: Always warm up before any physical activity and include gentle stretches for your calves and plantar fascia. This helps keep your foot and heel tendons flexible. Check out tips to prevent running injuries for more ideas.
- Pacing Activities: Gradually increase the intensity and duration of new activities. Don't overdo it too quickly, especially when starting a new exercise regimen.
Frequently Asked Questions About Heel Pain
We hear many similar questions from those dealing with heel pain. Here are some of the most common ones:
Why does my heel hurt so much in the morning?
Morning heel pain is a classic symptom of plantar fasciitis. When you sleep, your plantar fascia naturally shortens and tightens. When you take your first steps out of bed, this tightened band is suddenly stretched, often causing a sharp, stabbing pain. As you move, the fascia may loosen up, and the pain might decrease, only to return after periods of rest. Reduced blood flow to the area during rest and inflammation also contribute to this "start-up pain."
Can heel pain go away on its own?
Mild cases of heel pain, especially those caused by temporary overuse, can sometimes resolve with simple rest and activity modification. However, if the pain is persistent, severe, or lasts for more than a few weeks despite home care, it's unlikely to disappear completely without intervention. Ignoring persistent heel pain can lead to chronic issues, structural changes, and compensatory pain in other areas like your knees, hips, or back. It's always best to address the problem proactively.
What is the fastest way to relieve heel pain?
There's no single "fastest" cure, as relief often comes from a combination of strategies. To quickly alleviate heel pain, we recommend a multi-pronged approach:
- Rest: Reduce activities that aggravate the pain.
- Ice: Apply ice to the affected area to reduce inflammation.
- Gentle Stretching: Perform regular calf and plantar fascia stretches.
- Supportive Shoes: Wear well-cushioned shoes with good arch support, and avoid walking barefoot.
- Over-the-Counter Anti-inflammatories: Medications like ibuprofen can help manage pain and inflammation.
- Topical Relief Creams: For targeted, fast-acting relief, consider applying a topical cream. Neuropasil nerve pain relief cream, with its blend of menthol, aloe, and urea, can provide soothing comfort directly to the painful area, helping to reduce discomfort quickly.
Conclusion
Understanding what causes heel pain is the crucial first step toward finding lasting relief. We've explored the most common culprits like plantar fasciitis and Achilles tendon discomfort, as well as less frequent but equally important conditions involving structural issues, nerve impingement, and systemic diseases.
The good news is that for the vast majority of cases, heel pain can be effectively managed with conservative treatments and proactive prevention strategies. Whether it's through proper footwear, targeted stretches, activity modification, or supportive topical solutions, taking charge of your heel health is within reach.
Early diagnosis and consistent care are key. If you're experiencing persistent heel pain that interferes with your daily life, don't hesitate to seek professional medical advice. For soothing relief from discomfort associated with conditions like plantar fasciitis, Neuropasil's natural formula can be a helpful part of your home care routine.
Discover our fast-acting relief cream
References
- American Academy of Orthopaedic Surgeons. Heel Pain.
- American Academy of Orthopaedic Surgeons. Sever's Disease.
- American Family Physician. Diagnosis and Treatment of Plantar Fasciitis.
- American Podiatric Medical Association. Heel Pain.
- Cleveland Clinic. Heel Spurs.
- Cleveland Clinic. How to Prevent Running Injuries.
- Mayo Clinic. Heel pain Causes.














